Autor : Uribe EchevarrĂa, Loli1, Bertolin, Andrea V.1, Hidalgo, Gabriela1,2, Arato, Gisela1, Aguilera, Jesica1, Ălvarez Rurth1, Cadamuro, Gonzalo1, Marangoni, Alberto1, GonzĂĄlez, AnalĂa3, Maldonado, Cristina A.2,4, Quintar, Amado2,4
1Sanatorio Allende, CĂłrdoba Argentina.
2Universidad Nacional de CĂłrdoba, Faculty of Medical Sciences, Electron Microscopy Center.
3School of Exact Sciences, Physics and Natural Sciences.
4 National Scientific and Technical Research Council (CONICET), Research Institute on Health Sciences (INICSA).
https://doi.org/10.56538/ramr.LALM2453
Correspondencia : Loli
Uribe Echevarría Mail: loliuribe@hotmail.com
ABSTRACT
Chronic
obstructive pulmonary disease (COPD) is preventable by definition; however, there
are some steps that need to be taken in order to attain that goal. Its heterogeÂneous
nature is one of the main obstacles and challenges. In this regard, the risk
facÂtors for COPD are evolving beyond smoking. Despite the precision of the
spirometry in diagnosing COPD, it is not sensitive enough to identify
individuals at risk, thus, a new approach is required for precision medicine in
lung health. For that reason, we launched a Multidisciplinary Unit with new
approaches to prevention, risk prediction, definition, diagnosis, and
treatments that can make significant changes. The goals are focused on
preventing the development of COPD through a new medical care approach intended
for patients in the Pre-COPD stage, as well as translational research for understanding
the theragnostic markers of the disease.
Key
words: COPD;
Pre-COPD; Early diagnosis
RESUMEN
La
enfermedad pulmonar obstructiva crónica (EPOC) por definición es
prevenible sin embargo aún faltan gestos para alcanzar este objetivo. Su
carácter heterogéneo es uno de los principales obstáculos
y retos. Al respecto, los factores de riesgo de EPOC están
evolucionando, más allá del fumar. La espirometría a pesar
de su precisión en el diagnóstico de la EPOC, no es sensible para
identificar individuos de riesgo por lo que se requiere de un nuevo abordaje de
medicina de precisión en la salud pulmoÂnar. Es por ello que lanzamos
una unidad multidisciplinaria de nuevos abordajes de prevención,
predicción de riesgos, definición, diagnóstico y
tratamientos que puedan generar cambios significativos. Los objetivos se
focalizan en evitar el desarrollo de la EPOC a través de un nuevo
enfoque en la asistencia médica del paciente en la etapa Pre-EPOC, como
así también en la investigación traslacional para el conocimiento
de marcadores teragnósticos de la enfermedad.
Palabras
clave: EPOC;
Pre-EPOC; Diagnóstico precoz
Received: 04/02/2023
Accepted: 18/04/2023
INTRODUCTION
Chronic
obstructive pulmonary disease (COPD) is one of the leading causes of death
worldwide and represents a significant burden on public health in terms of lost
productivity and direct, indirect, and associated costs1. According to its definition,2 COPD is
preventable. But, unlike other chronic diseases such as cardiovascular
diseases, very few efforts have been made to attain that goal, probÂably due to
its heterogeneous nature.
Currently,
COPD poses important challenges. First of all, the global pattern of COPD risk
facÂtors is evolving. Although smoking is the main contributor to COPD,3-4 other risk
factors such as exposure to environmental pollution in low socio-economic
countries have become imporÂtant, as well as vaping and marijuana in young
people.2 In
fact, one-third of COPD cases are not related to smoking or environmental
exposure, but rather to physiopathogenic mechanisms involved in the trajectory
of lung function since the early stages of life, such as low birth weight,
prematurity, and intrauterine toxic exposure; childhood infectious and
obstructive respiratory diseases, the effects of tuberculosis, and physical
inactivity.5
Secondly,
COPD often has late diagnosis. While spirometry is a non-invasive, accessible,
and reproducible test with diagnostic precision for COPD, it is not the most
sensitive test to identify individuals at risk before they get sick, because by
the time the spirometry detects an obstruction or restriction, significant
damage to the airways has already occurred.6-10
Finally,
current scientific perspectives emphaÂsize the eradication of COPD10, 11. In
this sense, Martinez et al13 have proposed
the concept of foÂcusing on a pre-COPD stage in order to achieve these
objectives. It is hopeful to be able to identify individuals at risk of
developing COPD and to implement preventive and follow-up measures, or possible
early therapeutic interventions in this group of patients in order to modify
the course of the disease and reduce morbidity and mortality, and the burden on
public health.
Consequently,
the current risk model and preÂdiction instruments are inadequate and require a
new approach to precision medicine in lung health. This is why we
launched a Multidisciplinary Unit of new approaches to prevention, risk
prediction, definition, diagnosis, and treatments that can make significant
changes.
The
objectives of the Pre-COPD unit are
âą
To identify risks of respiratory diseases during gestation and intrauterine
development.
âą
Emphasize the prevention of risk factors, early diagnosis, and treatment of
obstructive respiraÂtory diseases during childhood.
âą
Preserve lung health and primary prevention of COPD.
âą
Detect risk factors in early stages and stratify them.
âą
Optimize the care of patients at risk.
âą
Modify the course of the disease.
âą
Educate and raise awareness among the population about COPD prevention and
care.
âą
Generate translational research activities in the field.
âą
Train human resources with expertise in the area.
Medical
assistance services
âą
Prevention and diagnosis of respiratory diseases during pregnancy.
âą
Prevention, diagnosis, and treatment of obstructive and infectious respiratory
diseases during childhood.
âą
Follow-up of children with high-risk of respiratory disease until adulthood.
âą
Care for teenagers and young adults with exposure to risk of respiratory
disease.
âą
Primary prevention of COPD in high-risk groups.
âą
Early diagnosis of COPD â Pre COPD.
âą
Medical assistance for smoking cessation.
âą
Personalized care for patients at risk of developing COPD in order to prevent
the development of the disease.
âą
Respiratory rehabilitation.
âą
Education of the patient and his/her family regarding COPD prevention and care.
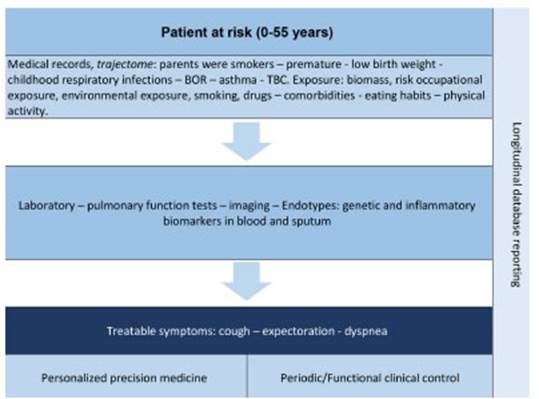
This comprehensive care starts from conception, identifying smoking mothers and fathers at risk of developing COPD; pregnancies at risk of developÂing respiratory disease; children aged 0 to 15 with obstructive and infectious respiratory disease; adults 16 to 55 years, with or without respiratory symptoms, smokers, and individuals exposed to inhalable materials such as all kinds of smoke, dust, and irritating and chemical vapors. In this way, the patient is identified and diagnosed, a perÂsonalized treatment is administered, and periodic 86 follow-up and evaluation are carried out in order to preserve functional lung capacity and respiratory health. Figure 2 (https://www.sanatorioallende.com/landing/unidad-de-pre-epoc#general).
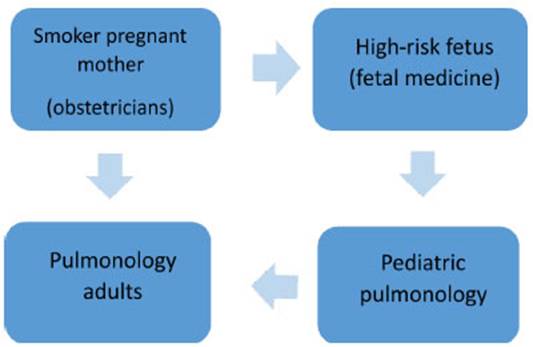
According
to the patientâs age group, the treatÂing physician varies. The obstetrician
refers parÂents with risk of COPD to the adult pulmonologist, while the newborn
is referred to the pediatrician.
The
pediatrician then refers the patient to the adult pulmonologist for
clinical/functional follow-up and prevention of disease development when the
patient reaches 16 years of age.
Teaching - human
resources training - community outreach activities
Monthly
meetings are held at the institution with the members of the Unit to discuss
clinical cases in order to improve their management, update the related
bibliography, research, and plan outreach activities for the population. In
terms of human resources training, two fellows are pursuing their doctoral
degrees in the area. Virtual campaigns are conducted annually reÂgarding COPD
awareness, early diagnosis, and smoking cessation.
Research
COPD
is heterogeneous in its mechanisms of development and progression, and is
drastically different in each patient, thus requiring the use of precision medicine
for its approach.14 In
this sense, there are significant gaps in the research being conducted
worldwide, with limitations in the understanding of the diseaseâs development
mechanisms that hinder the progress of precision medicine. To fill these
gaps, research is necesÂsary at the cellular, molecular, and genetic levels;
likewise, the development of imaging technologies and the detailed analysis of
clinical data promÂise to provide an unprecedented level of clarity regarding
the knowledge of physiopathogenic mechanisms of the disease and to prevent its
development.
The
actions that the Unit is carrying out in this regard, focusing on a precision
medicine, are:
âą
Storage, analysis, and monitoring of clinical and functional data of patients
at risk of developing COPD in the digital REDCAP system for longitudinal data
analysis (Graphic 2).
âą
Translational research on the mechanisms of COPD development. Cellular and omic
(proteomic, genomic) analysis in cooperation with basic researchers from the Universidad
Nacional de Córdoba.
âą
Analysis of potential early theragnostic COPD markers.
According
to the involved specialty, a trajecÂtome is prepared, that is to
say, the patientâs entire history of risk and functional factors in the
different stages of respiratory development is inÂcluded. A phenotype and
inflammatory endotypes are identified. Depending on the symptoms, the
therapeutic approach is personalized and precise, and includes hygienic and
dietary measures. The clinical and functional follow-up is periodic, and the
data are stored for subsequent analysis.
REFERENCES
1.
Polverino F, Celli B. The Challenge of Controlling the COPD Epidemic: Unmet
Needs. Am J Med 2018;131:1-6. https://doi.org/10.1016/j.amjmed.2018.05.001
2.
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy
for the diagnosis, management, and prevention of chronic obstructive pulmonary
disease. URL https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.1-25Nov20_WMV.pdf.
3.
Wang C, Xu J, Yang L, Xu Y, et al. Prevalence and risk factors of chronic
obstructive pulmonary disease in China (the China Pulmonary Health [CPH]
study): a national cross-sectional study. Lancet 2018; 391:1706-17. https://doi.org/10.1016/S0140-6736(18)30841-9
4.
Han MK, Agusti A, Celli BR, et al. From GOLD 0 to Pre- COPD. Am J Respir Crit
Care Med. 2021;203:414-23.
https://doi.org/10.1164/rccm.202008-3328PP
5.
Martinez FJ, Han MK, Allinson JP, Barr RG, et al. At the Root: Defining and
Halting Progression of Early Chronic Obstructive Pulmonary Disease. Am J Respir
Crit Care Med. 2018;197:1540-51.
https://doi.org/10.1164/rccm.201710-2028PP
6.
Harvey BG, Strulovici-Barel Y, Kaner RJ, et al. Risk of COPD with obstruction
in active smokers with normal spirometry and reduced diffusion capacity. Eur
Respir J. 2015;46:1589-97. https://doi.org/10.1183/13993003.02377-2014
7.
Csikesz NG, Gartman EJ. New developments in the assessÂment of COPD: early
diagnosis is key. Int J Chron Obstruct Pulmon Dis. 2014;9:277-86.
https://doi.org/10.2147/COPD.S46198
8.
Celli BR, Agustí A. COPD: time to improve its taxÂonomy?
ERJ Open Res. 2018;4:00132-2017. https://doi.org/10.1183/23120541.00132-2017
9.
Bose S, Pascoe C, McEvoy C. Lifetime lung function trajectories and COPD: when
the train derails. Lancet Respir Med. 2023;11:221-22.
https://doi.org/10.1016/S2213-2600(22)00391-5
10.
Stolz D, Mkorombindo T, Schumann DM, et al. Towards the elimination of chronic
obstructive pulmonary disease: a Lancet Commission. Lancet. 2022;400:921-72.
https://doi.org/10.1016/S0140-6736(22)01273-9
11.
Dharmage SC, Bui DS, Walters EH, et al. Lifetime spiromÂetry patterns of
obstruction and restriction, and their risk factors and outcomes: a prospective
cohort study. Lancet Respir Med. 2023;11:273-82.
https://doi.org/10.1016/S2213-2600(22)00364-288
12.
Dransfield M, Stolz D, Kleinert S; Lancet COPD CommisÂsioners. Towards
eradication of chronic obstructive pulmoÂnary disease: a Lancet Commission.
Lancet. 2019;393:1786- 8.
https://doi.org/10.1016/S0140-6736(19)30950-X
13.
Martinez FJ, Agusti A, Celli BR, et al. Treatment Trials in Young Patients with
Chronic Obstructive PulmoÂnary Disease and Pre-Chronic Obstructive Pulmonary
Disease Patients: Time to Move Forward. Am J Respir Crit Care Med. 2022;205:275-87. https://doi.org/10.1164/rccm.202107-1663SO
14.
Postow L. Critical Challenges and Compelling Questions for Chronic Obstructive
Pulmonary Disease. Moving the Field Forward: A National Heart, Lung, and Blood
InÂstitute Perspective. Ann Am Thorac Soc. 2018;15:S282-
S284. https://doi.org/10.1513/AnnalsATS.201808-587MG