Autor : Carreño Saavedra, Ruth1, Bigot, MarÃa de los Ãngeles1, Tummino, Carlos1
1 Hospital Nacional Prof. A. Posadas (El Palomar, P. of Buenos Aires, Argentina).
https://doi.org/10.56538/ramr.LOXC4713
Correspondencia : Ruth Carreño Saavedra. E-mail: rupacasa@gmail.com
CASE REPORT
22-year-old
female patient with history of bronchial asthma since childhood. The patient was
referred to the bronchoscopy service to be evaluated for suspected
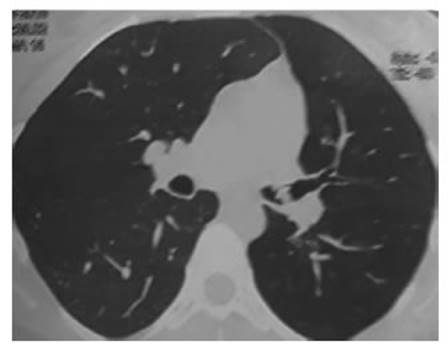
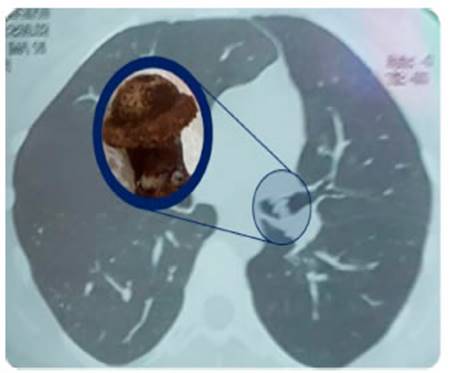
endoluminal tumor. She brings a normal spirometry. The chest tomography
shows endoluminal lesion at
the left main bronchus (LMB). The tomography also shows volume reduction of the left lung field
with homolateral mediastinal laterality and herniation of the right lung towards
the left. The physical examination
shows generalized sibilance
in the left lung field, without
any other alteration.
We performed a fibrobronchoscopy where we observed a thick
division spur 4 cm away from the
base of the left main bronchus (LMB). At first we thought
it was the
bronchus spur that divides the upper and lower lobe, but immediately
after such âspurâ we saw
a rounded, off-white, wrinkled, mobile lesion. It is
assumed that the image interpreted
as a spur could be an adhesion located
at the distal level of the LMB that doesnât
allow access to bronchial segmentation or the removal
of the mobile lesion that we
observed. We performed radiofrequency ablation at the middle part of the adhesion. After
cutting the adhesion, it was
possible to access the normal bronchial segmentation and remove with a biopsy bracket
the off-white formation that was covered with
fibrin and desiccated mucus
secretions. When we analyzed it
outside the patient, after removing the layer
of secretions, we could identify the cap of a pen.


The patient remembered that when she was
5 years old, she was playing
with a pen and aspirated the cap. Our patient
has a favorable evolution, she
no longer needs bronchodilator treatment because she is
better and has no symptoms.
DISCUSSION
The aspiration of a foreign body is
an uncommon clinical entity in adults and requires a high index of clinical
suspicion for its diagnosis, especially in people without a history of foreign body aspiration or without the
presence of any of the risk factors,
such as advanced age, use of sedatives, neurological or neuromuscular disorders, traumatisms, alcoholism or handling
of tracheostomy cannulas1-3.
Foreign bodies can be
classified in organic and inorganic substances; the aspiration of the latter is
common in children and young people who
introduce the substance into their mouth
as entertainment1 .
A
chest tomography is recommended to see the location
and size of the foreign body in the airway, being
the tomography more sensitive and specific for the diagnosis2-4.
Late
diagnosis of the aspiration
of a foreign body in the airways causes chronic respiratory sympÂtoms, namely sibilance, dyspnea, and recurring infections, which are commonly confused with other
respiratory diseases such as asthma, among others. Thus,
wrong treatments are indicated without any improvement1-3,
6.
When a foreign body remains in the airway for
long periods of time, it produces an inflammatory reaction localized in the airway that can result in the appearance
of granulation tissue due to inflamÂmation and hyperplasia of the adjacent bronchial mucosa and is present the
whole time between the aspiration event and the removal
of the foreign body, originating anatomical alterations that are visible through
bronchoscopy4, 5.
Flexible
bronchoscopy is safe, it allows
for a more complete study of
the airways and has a high rate of success
in the identification and removal of foreign bodies1-4.
Conflict of interest
No
conflict of interest to
declare.
Acknowledgement
Fabricio
Crudo (graphic designer).
REFERENCES
1.
Blanco Ramos M, Botana-Rial M, García-Fontán
E, Fernández-Villar A, Gallas Torreira M. Update in the extraction
of airway foreign bodies in adults. J Thorac Dis. 2016;8:3452-6.
https://doi.org/10.21037/jtd.2016.11.32
2.
Ma W, Hu J, Yang M, Yang Y,
Xu M. Application of
flexible fiberoptic bronchoscopy
in the removal of adult airway foreign
bodies. BMC Surg. 2020;20:165. https://doi.org/10.1186/s12893-020-00825-5.
3.
Sancho-Chust JN, Molina V, Vañes
S, Pulido AM, Maestre L, Chiner E. Utility of Flexible Bronchoscopy for Airway Foreign
Bodies Removal in Adults. J Clin Med. 2020;9:1409.
https://doi.org/10.3390/jcm9051409.
4.
Hewlett JC, Rickman OB, Lentz
RJ, Prakash UB, Maldonado F. Foreign
body aspiration in adult airways: therapeutic apÂproach. J Thorac Dis. 2017;9:3398-409.
https://doi.org/10.21037/jtd.2017.06.137.
5.
Sehgal IS, Dhooria S, Ram B, et al. Foreign Body Inhalation in the Adult Population:
Experience of 25,998 Bronchoscopies
and Systematic Review of the Literature. Respir Care. 2015;60:1438-48.
https://doi.org/10.4187/respcare.03976.
6.
Kann K, Long B, Koyfman A. Clinical Mimics: An Emergency Medicine-Focused Review of Asthma Mimics. J Emerg Med. 2017;53:195-201.
https://doi.org/10.1016/j.jemermed.2017.01.005.