Autor : Calle, Catalina Alexandra1, Rosales, MarĂa Fernanda2, MacĂas Eddyn, RubĂ©n2
1Pulmonology Service, Axxis Hospital de Especialidades, Quito, Ecuador. 2Pulmonology Service, Hospital Carlos Andrade MarĂn, Quito, Ecuador.
https://doi.org./10.56538/ramr.VFNQ2915
Correspondencia : Catalina Calle E-mail: cata2906@hotmail.com
ABSTRACT
Introduction: idiopathic pulmonary fibrosis is a progressive, fatal disease characterÂized
by the findings of usual interstitial pneumonia in a high resolution tomography
or lung biopsy, or in a multidisciplinary discussion, also discarding other
etiologies such as connective tissue diseases or diseases associated with toxic
exposure.
The objective of this work was to
know the clinical characteristics, lung function and survival of the group of
patients diagnosed with idiopathic pulmonary fibrosis who were evaluated at the
Interstitial Lung Disease Clinic of the Hospital Carlos Andrade Marín.
Materials and methods: retrospective, cross-sectional, observational study. The study
population consisted of patients diagnosed with idiopathic pulmonary fibrosis who had been treated at the Interstitial Lung
Disease Clinic of the Hospital Carlos AnÂdrade Marín
between January, 2018 and February, 2020.
Results: 85.7% of the 35 patients with idiopathic pulmonary fibrosis included in
the analysis were male. At the time of the diagnosis, the mean age was 69.7
years (SD [standard deviation]: 9.26, range: 38-87 years). 20% and 37.1% of
patients showed dyspnea grade 3 and 4, respectively. 60% had smoking history.
45.7% of the diagnoses were made
with a multidisciplinary clinical evaluation and high resolution computed axial
tomography.
Conclusions: we have reported the largest cohort of patients with idiopathic pulmoÂnary
fibrosis in Ecuador; our results identified similar populations with other
study groups where the high resolution computed tomography and
multidisciplinary analysis are the most used methods for the diagnosis.
Key words: Idiopathic pulmonary fibrosis; Emphysema; Survival
RESUMEN
Introducción: la fibrosis pulmonar idiopática es una enfermedad progresiva y fatal
caracterizada por el hallazgo de neumonía intersticial usual en
tomografía de alta resolución o biopsia pulmonar, o en
discusión multidisciplinar y el descarte de otras etiologías como
enfermedades del tejido conectivo o exposicionales.
En cuanto a los objetivos de este trabajo, consisten en
conocer las características clíÂnicas, la función pulmonar
y la supervivencia del grupo de pacientes con diagnóstico de fibrosis
pulmonar idiopática evaluados en la clínica de intersticiales del
Hospital Carlos Andrade Marín.
Materiales y métodos: se trata de un estudio transversal, retrospectivo, observacioÂnal. La
población de estudio la constituyeron los pacientes con
diagnóstico de fibrosis pulmonar idiopática atendidos en la
clínica de intersticiales del Hospital Carlos AnÂdrade Marín
entre enero del 2018 y febrero del 2020.
Resultados: de 35 pacientes con fibrosis pulmonar idiopática incluidos para el
análiÂsis, el 85,7 % fueron del sexo masculino. Al momento del
diagnóstico, la edad promeÂdio fue de 69,7 años (DE: 9,26, Rango:
38-87 años). El 20 % y 37,1 % presentaron disnea de grado 3 y grado 4,
respectivamente. El 60 % presentaron antecedentes de tabaquismo.
El 45,7% de los diagnósticos se hicieron tanto con
evaluación clínica multidisciplinaria y tomografía axial
computarizada de alta resolución.
Conclusiones: hemos informado la mayor cohorte de fibrosis pulmonar idiopática en
el Ecuador, nuestros resultados han identificado poblaciones similares con
otros gruÂpos de estudio en los que la tomografía computarizada de alta
resolución y el análisis multidisciplinar son los métodos
más utilizados en el diagnóstico.
Palabras clave: Fibrosis pulmonar idiopática; Enfisema; Sobrevida
Received: 5/16/2022
Accepted: 8/23/2022
INTRODUCTION
Idiopathic pulmonary fibrosis
(IPF) is a progresÂsive fibrosing interstitial
disease of unknown oriÂgin and poor prognosis, which ranges between 2 and 5
years of survival from time of diagnosis. It is the most common form of diffuse
interstitial lung disease (DILD), with a prevalence that oscillates between
twelve cases for every 100,000 women and 20 cases for every 100,000 men.1
This disease has an insidious
onset of sympÂtoms, with non-specific symptoms characterized by progressive
dyspnea, dry cough, Velcro-type tele-inspiratory
crackles and acropachy.1
The diagnosis is based on the
findings of usual interstitial pneumonia (UIP) in the high resolution computed
tomography (HRCT) or lung biopsy, or in a multidisciplinary discussion, also
discarding other etiologies, such as connecÂtive tissue diseases or diseases
associated with toxic exposure. Treatment is based on antifibrotic
agents, symptom management, and respiratory rehabilitation.2, 3
The first Latin American study
reported 761 ill patients diagnosed with idiopathic pulmonary fibrosis, where
Argentina and Mexico had the largest number of reported patients, 30.5% and
27.3%, respectively. 1.7% (n = 13) of the cases were from Ecuador.4
There are no DILD data in
Ecuador, so the naÂtional epidemiologic characterization is complex. Taking this
situation into account, the Hospital de Especialidad
Carlos Andrade Marín has created a DILD Clinic
of national reference, which was established in a multidisciplinary way, thus
allowÂing for the optimization of diagnosis, treatment, and registration processes.
Furthermore, access to antifibrotic treatment in the
country is limited, on the one hand, due to the little availability in
specialized care centers, and on the other hand, to the cost of these drugs.
This situation has a negative impact on survival, as shown by Cottin.5
The objective of this work was to
know the cliniÂcal characteristics, lung function and survival of the group of
patients diagnosed with IPF who were evaluated at the Interstitial Lung Disease
Clinic of the Hospital Carlos Andrade Marín.
MATERIALS AND METHODS
Retrospective,
cross-sectional, observational study.The study population consisted of patients diagnosed with IPF who had been treated at the Interstitial Lung Disease
Clinic of the Hospital Carlos Andrade Marín
between January, 2018 and February, 2020.
Inclusion criteria comprised
adult patients who met the diagnostic criteria of the 2012 and 2018
ATS/ERS/JRS/ ALAT Guidelines for UIP, confirmed through tomography or lung
biopsy, in whom a secondary disease was discarded; also, the patients who had
been analyzed by a multidisciÂplinary committee, with complete medical records
were included. Exclusion criteria: pediatric patients, patients with other
secondary interstitial diseases, or neoplasia, and
those who didn’t do the lung function tests.
Variables under evaluation: age,
sex, tobacco use, gastroesophageal reflux disease,
pulmonary emphysema, family history of pulmonary fibrosis, clinical
characteristics (cough, grade of dyspnea, Velcro-type crackles, acropachy), respiratory functional characteristics, such as
forced vital capacity (FVC) in liters and expressed as percentage of predictive
value, diffusing capacity of the lungs for carbon monoxide (DLCO) as percentage
of predictive value, six-minute walk test, diagnostic method (HRCT, lung biopsy
or multidisciplinary discussion) and treatment.
In smokers, we calculated the
smoke index according to the number of packs consumed per year. The Charlson index was used to describe comorbidities.6
Statistical analysis
The descriptive analysis of
qualitative variables was carried out by calculating absolute and relative
frequencies. The results of quantitative variables were expressed as mean
values, since data distribution was normal according to the Kolmogórov-Smirnov
test.
Factors taken into account for
the analysis of survival were: sex, age, smoking history, diagnosis of
pulmonary emphysema, Charlson index, grade of
dyspnea, systolic pressure of pulmonary artery and treatment with disease
modifiers. Survival was assessed in general and according to different factors
with Kaplan-Meier models; and the Log Rank Mantel Cox test was used to
establish differences between the survival gaps. The association of mortality
with risk factors was calculated through Cox Regression, obtaining the hazard
ratio values with their corresponding confidence intervals. Ap-value
of less than 0.05 was taken into account for statistical significance.
RESULTS
One patient was excluded from a
total of 36 poÂtentially eligible patients, due to incomplete lung function
tests.
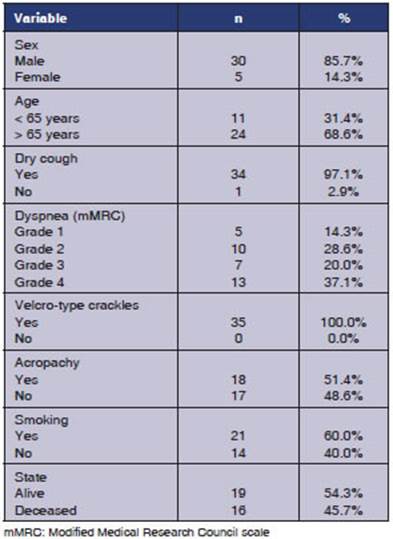
Table 1 shows the general
characteristics of the participants. 85.7% were male. At the time of the
diagnosis, the mean age was 69.7 years (SD: 9.26, range: 38-87 years). 20% and
37.1% of patients showed dyspnea grade 3 and 4, respectively. 60% had smoking
history. The mean amount of packs/ year among smokers was 9.1 (SD: 11.45).
45.7% died during the follow-up period.
With regard to clinical history,
diagnosis and treatment, 22.9% and 8.6% were diagnosed with gastroesophageal
reflux and pulmonary emphyÂsema, respectively. 45.7% of the diagnoses were made
both through multidisciplinary clinical evaluation and HRCT. 28.6% received
treatment with disease-modifying drugs (17.1%, nintedanib
and 11,4%, pirfenidone)
(Table 2).
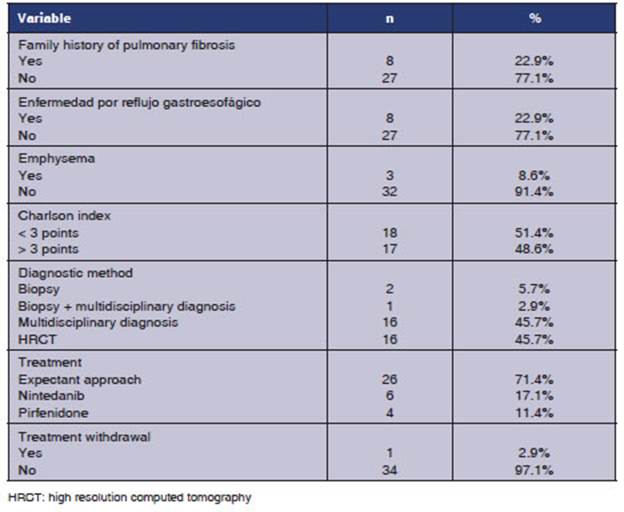
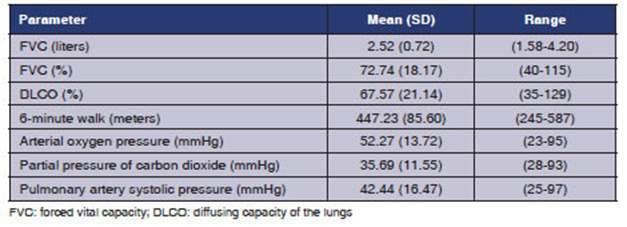
Table 3 shows the physiological
parameters evaluated in patients with IPF. The mean FVC obtained was 72.74%
(range: 40 to 115), whereas the DLCO was 67.57% (range: 35-129). The mean
distance travelled in the six-minute walk test was 447.23 m (SD: 85.60). The mean
value of arterial oxygen pressure (mmHg) was 52-27 (SD: 13.72) with the height
of Quito (2850 m). The mean value of the pulmonary artery systolic pressure was
42.44 mmHg (SD: 16.47).
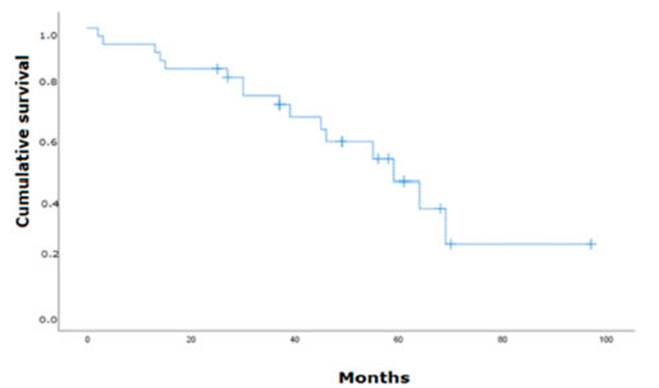
Mean survival of analyzed
patients was 57.24 months (95% CI: 45.07%-69.41%, SD: 6.21). When reaching 15
months of follow-up, around 15% (n = 5) of patients died. At 30 and 45
months, the cumulative mortality was 24% (n=8) and 36% (n=13). Until 65 months,
the cumulative mortality reached 63% (n=22)
(Figure 1).
Factors associated with survival
are explained in Table 4. The diagnosis of pulmonary emphyÂsema was
significantly associated with reduced survival time (HR: 4.210, 95% CI:
1.133-15.643, p = 0.032). Furthermore, patients older than 65 years (HR:
2.559, 95% CI: 0.779-8.409, p = 0.122), non-smokers (HR: 2.518
0.913-6.948, p = 0.075) with pulmonary hypertension (HR: 3.947, 95% CI:
0.926-16.832, p = 0.063) show clinically relevant mortality associations
(Table 3).
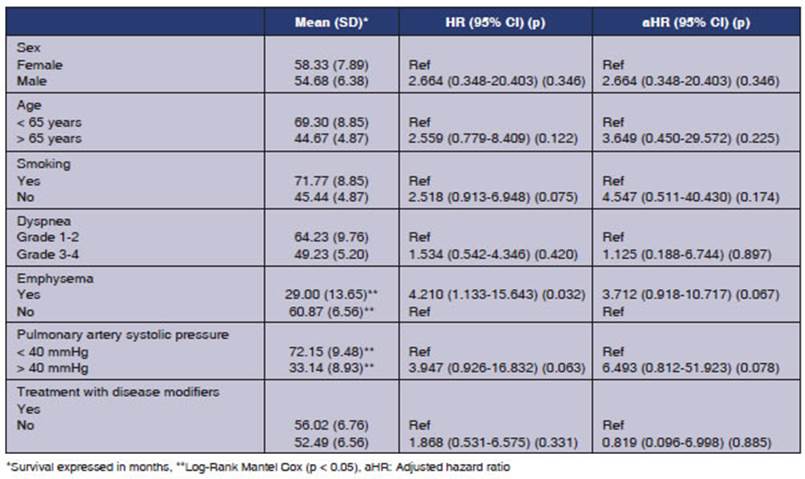
The widest gaps in mean survival values
accordÂing to the Kaplan-Meier analyses were observed in the following factors:
age (< 65 years: 69.3 months versus > 65 years: 44.67), smoking
(non-smokers: 45.44 months versus smokers: 71.77 months), diÂagnosis of
emphysema (Yes: 29 months versus No: 60.87 months) and value of pulmonary
artery sysÂtolic pressure (< 40 mmHg: 72.15 months versus > 40 mmHg: 33.14 months). Both the history of pulmonary
emphysema and the value of the pulÂmonary artery systolic pressure showed
statistical significance in the Log-Rank Mantel Cox Test (p = 0.019) and
(p = 0.046), respectively.
DISCUSSION
The evaluation of
this cohort of patients with IPF in a developing country such as Ecuador showed
the common characteristics of this disease as reÂgards its clinical and
functional parameters and diagnostic methods.
The mean age at the
time of the diagnosis was consistent with what is described in the literature,
as well as the higher prevalence of men.4,
5, 7
According to the
current ATS/ERS Guidelines, the lung biopsy is not necessary to establish the
IPF diagnosis in patients with tomographic features that confirm UIP, they should even be avoided due to the significant risk
of morbidity and mortality. Taking these reasoning and current guidelines into consideration,
in this study we observe a reduction of only 3% in the number of lung biopsies.
This percentage seems to be much lower than the one observed in other series.8
In any case, as it has been informed in the literature in the
past few years, there is a tendency to reduce the number of biopsies performed
in patients with this disease, as reported by the Korean cohort analyzed by
Sung Woo Moon.9
In the study of Wuyts, which analyzed 277 paÂtients diagnosed with IPF,
there was family history in 7% of patients, a low percentage compared to our
research. It would be interesting in the long run to analyze this population
genetically.10
The FVC was similar
to PANTHER-NAC, higher than ASCEND, and lower than NPULSIS-1 and INPULSIS-2.11-13
Furthermore, the DLCO exÂpressed in percentage and other
parameters of lung function, indicated less severe disease in our study group.14
Comorbid conditions
are increasingly being observed among patients with DILD. Data suggest a higher
prevalence of several comorbidities in paÂtients with IPF compared to the
general population. 48.6% of the study group has a Charlson
index score of > 3, representing lower values in comparison to those of the Cottin study, which reports 47.3% with a Charlson index score of > 5. This could be partly
explained by the younger age of our cohort of patients.4
Pulmonary hypertension and pulmonary emphysema are associated
with reduced survival time, as reported by the Mexican study of Mejía et al, with a HR for emphysema of 1.99
(1.12-3.53) p = 0.018, a PASP (pulmonary artery systolic pressure) of
more than 75 mmHg, and HR of 1.88 (1.01-3.48) p = 0.04 for pulmonary
hypertension.15
IPF is a disease with
a high mortality rate. Thanks to the ATS/ERS guidelines, a diagnostic method
has been standardized, thus allowing timely treatment. On the other hand,
global epiÂdemiological data have been obtained, with which significant
breakthrough has been made in the research of this disease.
Basing on that
information, it is time to estabÂlish in Ecuador the necessary measures to
allow a better diagnostic/therapeutic approach for lung interstitial diseases
and with that, the knowledge of the epidemiological impact they represent; to
that end we propose a national record of patients with DILD and in turn, the
creation of multidisÂciplinary committees for the purpose of directing
treatment access in the long run.
CONCLUSION
We have reported the
largest cohort of IPF patients in Ecuador. Our results have identified similar
popÂulations with other study groups where the HRCT and multidisciplinary
analysis are the most used methods for the diagnosis. Comorbidities, such as
pulmonary hypertension and emphysema show a reduction in survival time. Barely
29% of the population under evaluation received antifibrotic
treatment, so, apart from providing information on the characterization, we are
able to observe the natural course of the disease.
It is indispensable
to have well-organized and unified records of IPF patients so as to obtain
better results.
Conflicts of interest
The authors of this
work declare there isn’t any conflict of interest in relation to this
publication.
REFERENCES
1. Raghu G, Collard
H, Egan J, et al. An Official ATS/ERS/ JRS/ALAT Statement: Idiopathic Pulmonary
Fibrosis: Evidence-based Guidelines for Diagnosis and Management. Am J Respir Crit Care Med. 2011;183:788-824. https://doi.org/10.1164/rccm.2009-040GL
2. Raghu G, Rochwerg B, Zhang Y, et al. American Thoracic Society;
European Respiratory society; Japanese RespiratoÂry Society; Latin American
Thoracic Association. An official ATS/ERS/JRS/ALAT clinical practice guideline:
treatment of idiopathic pulmonary fibrosis. An update of the
2011 clinical practice guideline. Am J Respir Crit Care Med 2015;192:e3-e19.
https://doi.org/10.1164/rccm.1925erratum
3. Raghu G, Remy-Jardin M, Myers JL, Richeldi L,
Ryerson CJ, Lederer DJ, et al.; American Thoracic
Society, European Respiratory Society, Japanese Respiratory Society, and Latin
American Thoracic Society. Diagnosis of idiopathic pulmonary fibrosis: an
official ATS/ERS/JRS/ ALAT clinical practice guideline. Am J Respir Crit
Care Med 2018;198: e44-e68.
4. Caro F, Buendía-Roldan I, Noriega-Aguirre L, et al, Latin
American Registry of Idiopathic Pulmonary Fibrosis (REFIPI):Clinical
Characteristics, Evolution and TreatÂment. Arch Bronconeumol. 2022:S0300-2896(22)00329-5.
5. Cottin V, Spagnolo P, Bonniaud P, et al. Mortality and Respiratory-Related
Hospitalizations in Idiopathic PulÂmonary Fibrosis Not Treated With Antifibrotics. Front Med (Lausanne). 2021;8:802989.
https://doi.org/10.3389/ fmed.2021.802989
6. Charlson M, Carrozzinob D, Guidib J, Patierno C, CharlÂson Comorbidity Index: A Critical Review of Clinimetric Properties Psychother
Psychosom 2022;91:8-35. https://doi.org/10.1159/000521288
7. Gao Jing, Kalafatis D, Carlson L, et al.
Baseline
characterisÂtics and survival of patients of idiopathic pulmonary fbrosis: a longitudinal analysis of the Swedish IPF
Registry. Respir Res. 2021;22:40.
https://doi.org/10.1186/s12931-021-01634-x
8. Fisher J, Kolb M, Algamdi, et al. Baseline characteristics and comorbidities
in the CAnadian Registry for Pulmonary Fibrosis. BMC Pulm Med.
2019;19(1):223. https://doi.org/10.1186/s12890-019-0986-4
9. Moon S, Kim S,
Chung M, et al. Longitudinal Changes in Clinical Features, Management, and
Outcomes of IdioÂpathic Pulmonary Fibrosis. A Nationwide
Cohort Study. Ann Am Thorac Soc. 2021;18:780-7. https://doi.org/10.1513/ AnnalsATS.202005-451OC
10. Wuyts W, Dahlqvist C, Slabbynck H, et al. Baseline clinical characteristics,
comorbidities and prescribed medication in a real-world population of patients
with idiopathic pulmonary fibrosis: the PROOF registry. BMJ Open Respir Res 2018; 5:e000331. https://doi.org/10.1136/bmjresp-2018-000331
11. Raghu G, Anstrom KJ, King TE Jr, et al.
Prednisone, AzaÂthioprine, and N-Acetylcysteine for
Pulmonary Fibrosis. N Engl J Med. 2012;366:1968-77. https://doi.org/10.1056/ NEJMoa1113354
12. Richeldi L, du Bois RM, Raghu G, Azuma A, Brown KK, Costabel U, et al.; INPULSIS Trial Investigators. Efficacy and safety of nintedanib in
idiopathic pulmonary fibrosis. N Engl J Med
2014;370:2071-82. https://doi.org/10.1056/
NEJMoa1402584
13. King T, Bradford
W, Castro-Bernardini S, et al. A
phase 3 trial of pirfenidone in patients with
idiopathic pulmonary fibrosis. N Engl J Med.
2014;370:2083-92. https://doi.
org/10.1056/NEJMoa1402582
14. Behr J, Kreuter M, Hoeper MM, et al.
Management of paÂtients with idiopathic pulmonary fibrosis in clinical
practice: the INSIGHTS-IPF registry. Eur Respir J 2015;46:186-96.
https://doi.org/10.1183/09031936.00217614
15. Mejía M, Carrillo G, Rojas J, et
al. Idiopathic Pulmonary Fibrosis and
Emphysema: Decreased Survival Associated With Severe Pulmonary Arterial
Hypertension. Chest. 2009;136:1-2.
https://doi.org/10.1378/chest.08-2306