Autor : Oliva Virginia1, Prato Franco1, Mainero Flavia1, Sastre Ignacio2 , Bustos Mario2, España Manuel2, Carranza MartĂn3
1Diagnostic Imaging Service, Hospital Privado Universitario de CĂłrdoba, City of CĂłrdoba 2Thoracic Surgery Service, Hospital Privado Universitario de CĂłrdoba, City of CĂłrdoba 3Hospital RaĂşl A. Ferreyra, City of CĂłrdoba
http://orcid.org/0000-0001-6268-4055
http://orcid.org/0000-0001-6268-4055
https://orcid.org/0000-0002-0844-9238
Correspondencia : Virginia Oliva. DirecciĂłn: Av Naciones Unidas 346, CĂłrdoba Capital, Argentina E-mail: viroliva230992@gmail.com
ABSTRACT
Exogenous lipoid pneumonia (ELP)
is an unusual disease, with an incidence of 1 to 2.5%, caused by aspiration and
accumulation of exogenous lipids in the pulmonary alveoli. When the aspirated
agent has an oily composition, a pulmonary inflammatory reaction called lipoid
pneumonia is triggered, which over time can lead to irreversible parenchymal
fibrosis. Sometimes it can appear as nodular lesions that require a broad
differential diagnosis, in which case imaging studies have a fundamental role.
HistoÂpathological confirmation is required for definitive diagnosis1 .
We present a clinical case of
lipoid pneumonia which appeared as a lung mass acÂcompanied by bilateral
pulmonary infiltrates.
Key words: Lipoid pneumonia, Vaseline, Lung mass, Intra-alveolar lipophages
RESUMEN
La neumonía lipoidea exógena (NLE) es una
patología inusual, que tiene una inciÂdencia del 1% al 2,5%, y tiene su
causa en la aspiración y la acumulación de lípidos de
origen exógeno dentro de los alvéolos pulmonares. Cuando el
agente aspirado es de composición oleosa, se desencadena una
reacción inflamatoria pulmonar denomiÂnada neumonía lipoidea, que
con el tiempo puede conducir a una fibrosis parenquiÂmatosa irreversible. En
ocasiones, se puede presentar en forma de lesiones nodulaÂres, que obligan a un
amplio diagnóstico diferencial, en el que desempeñan un papel
fundamental los estudios por imágenes. Para el diagnóstico
definitivo, se requiere confirmación histopatológica1 .
Presentamos un caso clínico de neumonía lipoidea que se
presentó como masa pulmonar acompañada de infiltrados pulmonares
bilaterales.
Palabras claves: Neumonía lipoidea, Vaselina, Masa pulmonar, Lipofagos
intraalveolares
Recibido: 08/10/2020
Aceptado: 01/04/2021
INTRODUCTION
Lipoid pneumonia is a rare
disease that results from the aspiration of mineral, animal or vegetaÂble oils
into the lungs. Once the oil is inhaled, it is phagocytized by the macrophages
that fill the alveoli and loosen the alveolar walls, causing acute, chronic
pneumonitis. Over time, the macrophages carry the oils from the alveoli to the
interlobular septa, resulting in localized granulomas and pulÂmonary fibrosis2 .
Predisposing factors include neuÂromuscular disorders and esophageal anomalies2 .
We present the case of a male
patient diagnosed with lipoid pneumonia. This case is of great inÂterest
because the patient didn’t have swallowing disorders and showed an
atypical-particular radioÂlogical image, a spiculated lung mass with ground
glass infiltrates and bilateral interlobular septal lines.
CASE REPORT
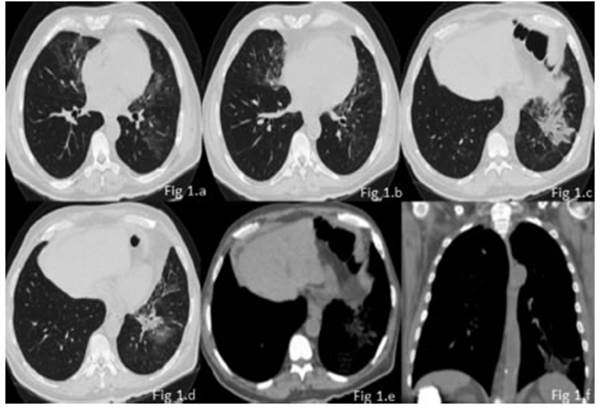
64-year-old male patient, university teacher, with history of insulin-dependent type I diabetes and chronic constiÂpation, and without history of smoking. The patient was admitted to our institution with fever associated with asthenia, myalgia and arthralgia of 10 days of evolution. Subsequently, he had generalized cephalea and chronic cough. Given the current epidemiological context, the patient was tested for COVID-19 on two occasions, with negative results. Physical examination: BP 140/80; HR 85 lpm, BR 28 rpm, SatO2 94% aa, temperature 37.5 °C. He showed good ventilatory mechanics, and the auscultation identified fine crepitant rales in the left pulmonary base. Lab tests, cultures and specific serology were requested: hemoglobin, 8.9 mg-dl, PCR 27.8, negative hemocultures, negative urine cultures, negative sputum, negative galacÂtomannan. A chest radiography was performed initially, showing a left basal consolidation; so, the patient began antibiotic treatment with azithromycin-ceftriaxone for 5 days, and then the regimen was modified and the patient continued with piperacillin-tazobactam because he had persistent fever. Due to persistent fever and lack of clinical response to treatment, a high-resolution chest tomography was performed, and it showed a spiculated, heterogenous lung mass with fibro-retractable bands and intralesional foci with negative density (fat density), located in the anÂterior and lateral segment of the left lower lobe. The mass was associated with patchy areas with increased interstitial-alveolar density, in ground glass opacity with geographic borders, with mild interlobular septal thickening (crazy paving pattern), in middle lobe, lingula and left lower lobe, with fine cylindrical bronchiectasis in the lingula.
Absence of adenopathies and pleural effusion (Figure 1).
Due to radiological findings, a
bronchoscopy with bronchoalveolar lavage (BAL) was performed: no germ
development, negative BAAR (acid-alcohol-resistant baciÂllus), no yeast-like
elements detected. From the clinical and radiological point of view, we were considering
a differential diagnosis between lipoid pneumonia and lung neoplasm, so we
decided to perform a biopsy for histopathological confirmation. First, a
transbronchial biopsy was taken, in which we could observe small fragments of
pulmonary parenchyma with moderate mononuclear, focal and diffuse inflammatory
infiltrate. Also, groups of lipophages were recognized. Since the diagnosis
wasn’t clear, a transthoÂracic puncture was carried out: its
anatomopathological report showed lung tissue with alveolar spaces covered by
pneumocytes without atypia, deposits of intraalveolar and interstitial
lipophages, and interstitial adipocytes. Epithelial malignancy was discarded,
and it was reported that morphological findings suggest the diagnosis of lipoid
pneumonia.
DISCUSSION
The radiological presentation of
our case is of great relevance, since it showed a lesion with heterogeÂneous
density, with an evident lipid component in the mediastinal window (lipid
range), simulating a mass of irregular borders which, together with the
consumption of liquid vaseline, suggested the diagnosis of exogenous lipoid
pneumonia without the fibrosing component.
It was produced as a consequence
of the aspiraÂtion of oils of vegetable, animal or mineral origin, and it can
present itself in an acute form, due to the accidental aspiration of a large
volume in a short time, or in a chronic form, with recurring intake of the
compound through the airways for a long period. The degree of inflammation and
lung fibrosis is related to oil aspiration: it depends on the amount of free
fatty acids present. In geneÂral, animal fat produces more inflammation and
fibrosis than vegetable or mineral fat, because it is hydrolyzed by pulmonary
lipases and releases free fatty acids3.
Regarding the clinical
presentation, it may be asymptomatic and show casual radiographic alteÂrations
or, there may be non-specific symptoms such as chronic cough, sometimes
productive cough, dyspnea or intermittent fever3, 5. Other less common symptoms are:
chest pain, hemoptysis, and weight loss.
The radiographic aspect is
non-specific, and can be described as consolidations or interstitial opacities,
or as a noteworthy mass suspicious for pulmonary neoplasm5.
Tomographic findings in exogenous
lipoid pneuÂmonia include a sequence of radiological events, with initial
predominance of ground glass opacities with centrilobular distribution, with
low attenuaÂtion value (-25 and -75 Hounsfield units). After one week, the
density of the aspirated segment increaÂses until it forms a clear
consolidation, increasing the value of the segment’s HUs.
After two weeks, the density is
reduced and returns mainly to ground glass opacities; during this period, the
crazy paving pattern appears (due to the migration of macrophages and inflammatory
cells to the interstitial lymphatic vessels). These opacities can be completely
resolved, leaving resiÂdual thickening of the interlobular septa. If that
doesn’t happen, as opacities increase, fibrosis will appear with up to
approximately 50% volume loss of the affected segment, with vascular
clustering, traction bronchiectasis and fissure displacement5.
Within the forms of radiologic
presentation, we found that consolidation is the most frequent finding in 90%
of the cases, with fat attenuation in 80%.
Then comes the form of irregular
mass in 66% of the cases.
Ground glass opacities were found
in 50% of isolated patients or associated with previously described findings,
just like the crazy paving patÂtern in 33%.
In cases of acute aspiration, we
don’t see any sign of volume loss, which does occur in the chronic forms of the
disease, in 80% of the patiens5.
Distribution is dependent on
severity: the posteÂrior segments of upper lobes and apical segments of lower
lobes being the most affected, in supine position, and basal segments in
standing position5.
Regarding the resolution, acute
aspiration usually improves in up to 80% of the patients, but very rarely
disappears completely. But chronic aspiration normally remains stable over time5 .
Diagnosing lipoid pneumonia is
usually difficult because it is not routinely suspected when it first appears.
Often, the cases are treated as commuÂnity-acquired pneumonia, and an
alternative diagnosis is considered only if the patient doesn’t respond to
treatment, as in our case. So, a detailed medical record has to be written,
emphasizing preÂvious exposure to fatty substances. Once the ELP is suspected,
it is necessary to detect intraalveolar lipids and lipid-laden macrophages in
respiratory samples. The samples may be taken from sputum, BAL, transthoracic
puncture-aspiration cytology or surgical lung biopsy. With regard to the
sputum, it is available but many patients can’t produce it, and so it may be
difficult to obtain a representaÂtive sample. It also has questionable
reliability, and lipid-laden macrophages have been found in the sputum in the
absence of lipoid pneumonia6.
The BAL is widely available nowadays, and its usefulness has been proven. It
may show a turbid or off-white liquid with visible drops of fat on the surface.
Transthoracic puncture is also a minimaÂlly invasive procedure of diagnostic
usefulness, though false negatives can be obtained due to the size of the
sample. Thus, in some cases, a transbronchial lung biopsy or even a surgical
biopsy may be necessary. Most reports have used lipid-laden macrophages as
diagnostic markers of lipoid pneumonia; however, some authors have questioned
their specificity6.
So, the diagnosis of exogenous lipoid pneumonia must be based on the
conjunction of the patient’s history of mineral oil intake, compatible
radiologic findings, and the presence of intraalveolar lipids or macrophages
with lipid content6.
Some possible complications are:
over infection by atypical mycobacteria, which should be suspecÂted in the
presence of cavitary nodules, and also the occasional appearance of epidermoid
carcinoma in chronic aspiration3,
5.
With regard to treatment, there
aren’t any studies that define the best therapeutic option, though the first measure
that should be taken is to identify and suspend the use of the causative agent,
which should generally be enough, mostly if the patient is asymptomatic4 . Some reports
suggest the use of corticosteroids to reduce inflammation. This treatment is
reserved for acute cases with severe lung damage. Another option is the use of
whole-lung lavage as it is used in alveolar proteiÂnosis. Surgical treatment is
reserved for patients that don’t respond to these last options and for
esophageal alterations1,
5.
Conflict of interest
The authors declare that there is
no conflict of interest.
BIBLIOGRAFÍA
1. Aliaga F, Chernilo S, Fernandez C, Valenzuela H,
Rodriguez JCs. Neumonía lipoidea exógena: Una inhabitual de
nódulos pulmonares. Casos clínicos. Rev Med Chil.
2017;145:1495-9. https://doi.org/10.4067/s0034-98872017001101495
2. Gaerte SC, Meyer CA, Winer-Muram HT, Tarver RD, ConcÂes
DJ. Fat-Containing Lesion of the Chest. RadioGraphics. 2002;22:S61-S78.
https://doi.org/10.1148/radiographics.22.suppl_1.g02oc08s61
3. Martin M, Torres R, Hernandorena M, Lopez Moraz J,
Rossi S, Codinardo C. Neumonía lipoidea exógena fibrosante en
paciente con enfermedad de parkinson. Rev Am Med Resp. 2020; 20: 189-94.
4. Alvarez-Cordoves MM, Mirpuri-Mirpuri PG, Rocha Cabrera
P, Pérez-Monje A. Neumonía lipoidea. A propósito de un
caso. Elsevier España, S.L. y SEMERGN. 2013; 39: 110-2.
5. Winer-Muran, Rosado-De-Christenson, Mohammed, AbÂbott,
Huller-Maier. Especialidades en Imagen TCAR de Pulmón. Edición
especial. Madrid, España: Marban. 2013; 3: 142-7.
6. Hadda, V., & Khilnani, G.
C. Lipoid pneumonia: an overview. Exp Rev Resp Med 2010;4:799–807.
https://doi.org/10.1586/ers.10.74176