Autor : AgustĂn Buero1, Silvia Quadrelli1, Domingo Chimondeguy2, Alejandro Lotti3, Bettiana Torterolo4
1Thoracic Oncology Center. British Hospital of Buenos Aires 2Department of Thoracic surgery. British Hospital of Buenos Aires 3Department of Pathology. British Hospital of Buenos Aires 4Department of Diagnostic Imaging. British Hospital of Buenos Aires
Correspondencia : E-mail: a_buero@hotmail.com
Abstract
Mucoepidermoid tumors of the trachea and bronchi are uncommon neoplasms, and represent less than 5% of all pulmonary neoplasms. We present a 29-year-old patientwho was referred to our hospital with complaints of cough with expectoration together with intermittent fever during 8 months without weight loss or hemoptysis. The CT scan of the chest revealed left upper lobe atelectasis and a polypoid mass in the left main bronchus with a diameter of about 16 mm. Bronchoscopy revealed a polypoidendobronchial tumor at 18 mm from tracheal bifurcation. The patient underwent a sleeve resection with bronchial anastomosis. The hystopathological analysis of post-operative material confirmed the diagnosis of a low grade, well-differentiated mucoepidermoid carcinoma. There were no complications during the post-operative period and the patient was discharged from hospital on the fifth day after surgery.
Key words: Bronchial tumor; Mucoepidermoid carcinoma; Surgery; Sleeve resection.
Introduction
Mucoepidermoid lung tumors of the trachea and bronchi are uncommon neoplasms, previously included under the term bronchial adenoma. They are morphologically and clinically similar to mucoepidermoid tumors of the salivary glands1 and represent less than 5% of all pulmonary neoplasms2. Histologically, MEC is characterized by a combination of mucus-secreting, squamous, and intermediate cell types.
Case report
A 29-year-old man was referred to our hospital with complaints of cough with expectoration along with on and off fever for last 8 months. He did not reported weight loss or hemoptysis. His past medical history was unremarkable.
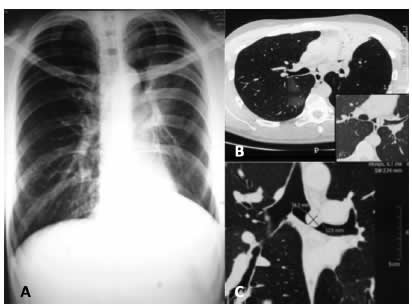
General physical examination revealed decreased breath sounds and decreased vocal resonance and wheezing on the left side. The examination of other systems was unremarkable. A chest radiograph was suggestive of volume loss in the left hemithorax (Figure 1A). Further evaluation with CT scan of the chest revealed left upper lobe atelectasis and a polypoid mass in the left main bronchus with a diameter of about 16 mm (Figure 1B-C).
Bronchoscopy was performed, revealing a polypoid endobronchial tumor, localized in the left main bronchus (18 mm from tracheal bifurcation), completely occluding its lumen (Figure 2A). The suspected diagnosis was a carcinoid tumor and because of the perspective of a surgical treatment, the risk of bleeding was not considered cost-effective and the tumor was not biopsied.
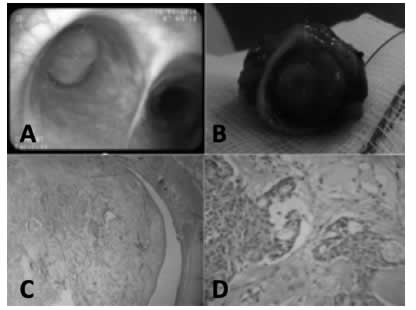
The patient was transferred to thoracic surgery ward for surgical treatment. He underwent a sleeve resection with bronchial anastomosis. The hystopathological analysis of post-operative material confirmed the diagnosis of a low grade, well-differentiated mucoepidermoid carcinoma (Figure 2B-C-D). The remaining bronchial stump did not contain microscopic disease.
Immunohistochemical results showed that the tumor was strongly stained with monoclonal antibodies anticytokeratins AE1 and AE3. It showed Ki67 antigen staining of 3% and CEA: (+). Tumor also stained for p53. There were no complications during post-operative period and the patient was discharged from hospital on the fifth day after surgery.
Discusion
When mucoepidermoid tumors occur in the bronchus they have been described as well circumscribed, covered by normal bronchial mucosa and characterized by local invasion with only a few instances of distant metastases3. In the World Health Organization’s histological classification of lung tumors, MECs belong in the main group of malignant epithelial tumors and the subgroup of salivary gland tumors4. Mucoepidermoid carcinoma of high-grade malignancy should be differentiated from adenosquamous carcinoma and from low-grade mucoepidermoid carcinoma, which has a better prognosis. MEC arise from bronchial glands, low-grade mucoepidermoid carcinoma are centrally located and show histologic features identical to their salivary gland counterpart, with mixture of mucinous glands, intermediate or squamoid cells, with no or mild atypia. High-grade mucoepidermoid carcinoma is more difficult to differentiate from adenosquamous carcinoma. Keratinization, a feature of adenosquamous carcinoma, is absent in high-grade MEC. Another difference is that the surface epithelium of MEC rarely shows in situ carcinoma.
Radical surgery based on lung cancer treatment is performed for MEC, and in recent years this operation has been frequently performed using VATS5. MECs of the lung are often treated by lobectomy, sleeve resection, local resection, segmental resection, or even endoscopic removal. Sleeve lobectomy should be considered when the primary bronchus is invaded, and pneumonectomy is the last choice6.
Regional lymphatic node metastases have been seen in less than 5% of these tumors. In high-grade tumors, the prognosis is variable. Although, high-grade MECs are thought to have a better prognosis than non-small cell lung carcinomas, they also should be treated by radical surgical treatment7.
Most patients with this disease have a favorable outcome after a complete resection. However, the disease may recur in distant organs in a small subset of the patients during long-term follow-up periods. Higher FDG uptake is associated with nodal disease in patients with primary salivary gland-type tumors of the lung but is not predictive of survival, whereas CT features suggestive of advanced disease correlate with worse outcome8.
Yousem and Hochholzer9 proposed that the prognosis of older patients and those with hilar lymph node metastasis is worse. In the series reported by Vadasz and Egervary10, only high-grade tumors develop lymph node metastasis and in the 21 patients reported by Xi et al, univariate analysis showed that age and TNM stage were correlated with OS and PFS. However, multivariate regression analysis revealed that lymph node metastasis was the only independent prognostic factor11.
Metastases in MECs occur by lymphatic or hematogenous ways. They are more frequent in the regional lymphatic nodes (48%), bone (25%), distant lymphatic nodes (18%), and the adrenal gland, cerebral, and skin (14%)12.
Postoperative radiation therapy or chemotherapy is unnecessary in the low-grade variant of these tumors.6 High-grade mucoepidermoid carcinoma carries a worse prognosis, and it must be treated as a non-small cell lung cancer with more radical surgical resection, even if this lesion is known to have a better prognosis than bronchogenic carcinoma13. Radiotherapy and chemotherapy should be added in patients whose surgical margins remained positive and whose tumors cannot be re-resected, or in inoperable patients who already are metastatic at the time of diagnosis. There is effective treatment for high-grade tumors and those patients usually have a poor prognosis14. Cisplatin, docetaxel, gemcitabine, adriamycin, and pemetrexed have been reported as potential chemotherapy combinations.
Given that the epidermal growth factor receptor (EGFR) is frequently overexpressed in MECs of salivary gland origin, bronchial MECs have been tested for EGFR. Evidence is inconclusive. There are several reports on the efficacy of the tyrosine kinase inhibitor gefitinib in patients with epidermal growth factor receptor (EGFR) gene mutations15 and it has been suggested that this molecularly targeted therapy is likely to improve the prognosis of cases with progressive high grade and recurrent MEC. However, in spite of some case reports, the role of TKI therapy in metastatic MECs remains unclear. It must be taken into account the finding that no activating EGFR mutations were detected in the tumors of patients who reportedly responded to the TKI therapy16 reported in a review of the literature, that 48 pulmonary MEC tumors were tested for EGFR mutations, and nine tumors (19%) tested positive for mutations. Of note, all the EGFR mutations were detected in the Asian population. Whether treatment with TKIs improves outcome in these patients remains unclear.
Conclusion
Primary pulmonary MEC represents a very infrequent type of lung cancer. Patients with low-grade MECs, like the present patient, usually have a good prognosis after primary surgical resection. Adjuvant treatment is not indicated for these patients. However, in cases of high-grade malignant neoplasm as in small cell lung cancer, surgery results in a significantly worse prognosis. The role of targeted therapy directed against EGFR is yet to be determined.
Conflict of interest: SQ is a consultant in the research study “Safety of pirfenidone in IPF” sponsored by DOSA.