1 ATS (American Thoracic Society)
2025, May 16 to 21
2 panish Society of Pulmonology
and Thoracic Surgery (SEPAR, by its Spanish acronym; Sociedad Española
de Neumología y Cirugía Torácica) 2025, June 12 to 14
ATS 2025 CONGRESS ON INTERSTITIAL LUNG DISEASES
Significant advances were
presented at the ATS 2025 Congress with regard to interstitial lung diseases.
Below are three of the most relevant studies, with additional updates to be
shared in future educational activities of the AAMR:
1. New treatment for pulmonary
fibrosis: For the first time in 11 years, a new drug for pulmoÂnary fibrosis
has been approved: NerandomiÂlast. In the Fibroneer IPF and Fibroneer ILD
studies (DOI: 10.1056/NEJMoa2414108 and DOI: 10.1056/NEJMoa2503643), this drug
was shown to reduce the rate of decline in forced vital capacity (FVC) in
patients with progresÂsive pulmonary fibrosis, both with and without
concomitant antifibrotic treatment. Although patients without concomitant
treatment showed a slower decline in FVC, these results should be interpreted
with caution, as differences in disease severity and duration between groups
probably exist. In addition, a reduction in morÂtality was observed in patients
treated with Nerandomilast in the Fibroneer ILD study.
2. First-line treatment in
pulmonary sarcoidosis: The PREMETH Study (DOI: 10.1056/NEJÂMoa2501443) compared
methotrexate and prednisone as initial treatment for pulmonary sarcoidosis. At
24 weeks, both treatments produced similar improvements in FVC, and
methotrexate was found to be non-inferior to prednisone. Although side effects
were comparable between the groups, prednisone was asÂsociated with greater
weight gain, insomnia, and increased appetite, while methotrexate caused more
nausea, fatigue, and liver abnormalities. These findings suggest that
methotrexate could be considered a first-line option, particularly in patients
concerned about steroid-related side effects.
3. Evaluation and management of
interstitial abÂnormalities: According to the ATS Clinical StateÂments (DOI:
10.1164/rccm.202505-1054ST), interstitial lung abnormalities are defined as
bilateral changes on computed tomography (such as ground-glass opacities,
reticulations, and honeycombing) affecting more than 5% of a lung area. The
updated definition no longer exÂcludes high-risk populations. Screening for
ILA/ ILD (interstitial lung abnormalities/interstitial lung disease) is
recommended in lung cancer imaging studies, in adults with connective tissue
diseases, and relatives of patients with familial pulmonary fibrosis. In
addition, it is essential to assess baseline symptoms and lung function, and to
follow up every 2-3 years.
This summary was prepared by the
Interstitial Lung Disease Section of the AAMR.
PARTICIPATION REPORT
58TH CONGRESS OF THE SPANISH SOCIETY OF PULMONOLOGY AND THORACIC SURGERY
(SEPAR)
Bilbao, Spain – June 2025
Santiago Larrateguy,
Physiotherapist– Specialist in
Respiratory RehaÂbilitation, Active member, AAMR
Speakers: Dr. Ane Arbillaga and Dr. Javier Gascón
Chronic dyspnea continues to be
one of the most complex symptoms in the management of respiÂratory diseases. In
this session, recent advances in the understanding of dyspnea were discussed
from a neuroscientific perspective, recognizing its central processing as a key
component, beyond the traditional peripheral approach.
Main concepts addressed:
• Role of pulmonary
rehabilitation: Recognized as one of the most effective interventions to
relieve dyspnea, although its exact mechanisms are still unknown. Current hypotheses
include:
o Optimization of respiratory and
peripheral muscle function.
o Reduction of ventilatory
demand.
o Cognitive and affective
improvements that modulate symptom perception.
• Breathing-Thinking-Functioning
(BTF) Model:
This clinical framework was
proposed to underÂstand the interaction between anxious thoughts, respiratory
alterations, and functional decline. This cycle perpetuates dyspnea even in the
absence of objective structural impairment.
• Nociplastic dyspnea:
An analogy with chronic pain was
used to deÂscribe situations where dyspnea persists without an evident
functional equivalent, suggesting central sensitization mechanisms.
• Clinical decoupling:
The low correlation between
dyspnea and tradiÂtional parameters such as FEV1 or the mMRC scale was
highlighted. The need to assess dysÂpnea as a multifactorial subjective
experience was emphasized.
• Current gaps:
o Lack of knowledge regarding the
degree of participation of chemoreceptors.
o Unclear interactions between
psychological factors and the perception of dyspnea.
Important references:
• Herigstad M, et al. Respir Med.
2011.
• Parshall MB, et al. Am J Respir
Crit Care Med. 2012.
• Pavlovic M, O’Daly O. Semin
Respir Crit Care Med. 2022.
• Booth S, et al. Prim Care
Respir J. 2013.
2. Teaching workshop: Motivational
interÂviewing (MI) in patients with chronic respiÂratory disease
A practical activity was
conducted focusing on the application of motivational interviewing as a
clinical tool to improve adherence and facilitate behavior change in the
context of rehabilitation.
Key areas addressed:
• Importance of MI in respiratory
rehabilitation:
o Effective approach to
ambivalence toward change.
o Strengthening the therapeutic
alliance through empathy, active listening, and afÂfirming language.
o Particularly useful in patients
with fear of dyspnea or frequent relapses.
• Techniques covered:
o OARS: use of open-ended
questions, affirmaÂtions, reflections, and summaries.
o Strategies for eliciting
motivation and colÂlaborative planning.
o Respectful, patient-centered
feedback.
It was emphasized that MI should
not be conÂsidered merely a communication technique, but rather an intervention
with strong evidence to induce sustainable changes in health behaviors.
3. Talk: Physical Activity
Interventions in Patients with Exacerbations
Speaker: Dr. Marian Ramon – Vall d’Hebron, Barcelona
The lecture focused on the
negative impact of respiratory exacerbations on physical activity and
functionality, and the need for early intervention in the recovery process.
Main points:
• Exacerbations significantly
reduce functional caÂpacity, muscle strength, and emotional well-being.105
• A significant gap was
identified between the intention to remain active and actual behavior after
hospital discharge.
• Factors such as depression,
fear, an unfavorable environment, and comorbidities contribute to inactivity.
Proposed interventions:
• Consider the exacerbation as a
key moment to initiate structured interventions.
• Integrate programs that
include:
o Motivational interviewing
o Individualized goals
o Identification of barriers and
facilitators
o Systematic follow-up of
progress
Clinical conclusion:
The implementation of
individualized strategies during the post-exacerbation stages can prevent
functional decline, improve quality of life, and optimize long-term prognosis.
Cited references:
• Pitta F. Chest. 2006
• Ramon MA. Eur Respir J. 2018
• Valeiro B. ERJ Open Res. 2025
• Feil K. Br J Sports Med. 2023
4. Institutional meetings and
collaboration opportunities
During the congress, informal
meetings were held with directors of the Respiratory Physiotherapy Area of
SEPAR, where a strong interest was expressed in establishing collaborative
links with the Respiratory Rehabilitation Section of the AAMR.
Below are some possible joint
actions:
• Invitation to virtual lectures:
Dr. Ane Arbillaga expressed her willingness to deliver the talk on dyspnea in a
virtual format for professionals in Argentina.
• Intersocietal research
projects: the possibility of generating multicenter research involving both
societies was discussed.
• Strengthening the academic
connection: plans were made to continue institutional dialogue to coordinate
future educational and scientific actions in a collaborative manner.
These initiatives represent a
strategic opporÂtunity to enhance the development of respiraÂtory
rehabilitation in the region, facilitating the exchange of knowledge and
experiences among Spanish-speaking professionals.
Acknowledgement
I sincerely thank the authorities
of the ArgenÂtine Association of Respiratory Medicine (AAMR) for their support
and the opportunity to participate in this international event. The possibility
of repÂresenting the institution in a high-level academic setting such as the
SEPAR Congress not only alÂlowed for rigorous scientific updating but also the
development of strategic connections that could lead to future
inter-institutional collaborations.
PRE-CONGRESS COURSE ON BRONCHIECTASIA IN THE FRAMEWORK OF THE 58TH SEPAR
CONGRESS IN THE CITY OF BILBAO, SPAIN, PRE-CONGRESS COURSE ON BRONCHIECTASIA
Bilbao, España - Junio 2025
Dra. Eugenia Alais
Pneumonology Department Hospital
Alemán
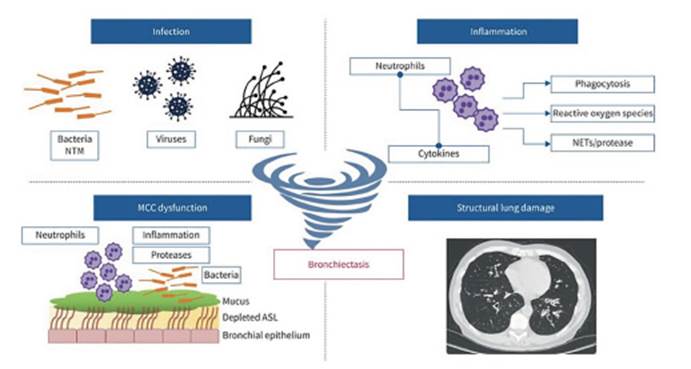
In the introduction, the
diagnostic algorithm from the SEPAR guideline published in 2018 was reviewed,
with its update expected by the end of 2025. The physiopathology was also
addressed, replacing the traditional model of inflammation, infection, and
structural damage with four key factors in disease development and progression:
infection, inflammation, impaired mucociliary clearance, and structural damage.
Instead of being represented as a circle, the new model is depicted as a
whirlwind or twister, where each component can independently affect the others.
Causes to consider include
disorders related to CFTR (cystic fibrosis transmembrane conductance regulator)
when cystic fibrosis (CF) has been ruled out. Suspicion should arise if the
patient presents with specific clinical features (phenotypes), after excluding
CF, or if there is evidence of partially functional CFTR protein with activity
levels below the threshold for CF. The most frequent forms of clinical presentation
are: bilateral bronchiectasis, ABPA (allergic bronchopulmonary aspergillosis),
chronic rhinosinusitis, recurrent acute or chronic pancreatitis, primary
sclerosing cholangitis, and absence of the vas deferens.
Another major causal group is related
to rheuÂmatologic diseases. The prevalence of bronchiecÂtasis in rheumatoid
arthritis (RA) is 3-30%, and it is associated with advanced arthropathy and
greater morbidity and mortality. Risk factors include advanced age, longer RA
duration, and genetic variants. In primary Sjögren’s syndrome, the
prevalence is 7-54%, usually cylindrical in type, predominantly affecting the
lower lobes (70%), and is associated with older age, hiatal hernia (50%), and
positive anti-SMAs (smooth muscle antibodies). In systemic lupus, prevaÂlence
ranges from 13 to 21%, though it remains unclear whether this is due to the
disease itself or a consequence of recurrent infections. Those associated with
vasculitis occur more frequently in women and with positive ANCA (antineutroÂphil
cytoplasmic antibody).
The diagnostic criteria for ABPA
(allergic bronÂchopulmonary aspergillosis) were reviewed, noting a lack of
consensus among societies, as criteria vary depending on the underlying
disease, and active screening is not routinely performed. For example, in
corticosteroid-dependent asthma, the prevalence is 2-5%; in CF, 8-9%; in COPD
(chronic obstructive pulmonary disease), 1-2.9%; and in bronchiectasis, 6%.
Currently, four phenotypes of ABPA are considered, but treatment remains similar,
with the objectives of controlling the imÂmune response, reducing fungal load,
improving symptoms, and preventing exacerbations and progression of
bronchiectasis.
When to suspect primary ciliary
dyskinesia? Symptoms include: persistent productive cough, situs inversus,
chronic rhinitis/rhinosinusitis, conÂgenital heart disease, otitis
media/hearing loss, and frequent respiratory infections. For diagnosis,
high-speed video analysis has a sensitivity of 95-100% and a specificity of
93-95%, evaluating coordination, amplitude, and pattern of ciliary movement.
Among immunological causes, the
most frequent is common variable immunodeficiency (CVID), with a bronchiectasis
prevalence of 34-68%, and it should be suspected in patients with frequent
respiratory infections, pneumonias, severe sinus disease, and otitis. CVID is
also associated with meningitis, endocarditis, abscesses, osteomyelitis, and
sepsis. Within the bronchiectasis algorithm, all patients should have IgA, IgG,
IgM, IgE, and C3/C4 levels measured. In selected cases, IgG subclasses and B,
T, NK phenotyping should also be performed.
Bronchiectasis and digestive
disorders: the lung–gut axis has a common origin, a specialized epithelium,
physical barriers (mucus, ciliated or secretory cells), mucosa-associated
lymphoid tissue (MALT), shared microbiota, and similar immunoÂlogical
responses. Reflux is associated with NTM (nontuberculous mycobacteria) and
bronchiectasis (BQ), but reflux itself was not found to be a causal factor of
BQ. Similarly, inflammatory diseases of the colon may have a positive genetic
correlation with BQ but do not have a direct causal effect.
Other causes of BQ include
accessory tracheal bronchus, tracheobronchomalacia, tracheal or bronchial
stenosis, bronchogenic cyst, pulmonary sequestration, William-Campbell
syndrome, yelÂlow nail syndrome, Mounier-Kuhn syndrome, Young’s syndrome, and
alpha-1 antitrypsin deÂficiency.
Finally, different causal
pathologies of BQ were reviewed, which we must keep in mind in our daily
practice and not settle for idiopathic causes without investigating their
origin.