Autor : Rojas Mendiola, Ramiro Horacio1, Smurra, Marcela Viviana1
1 Center for Respiratory Failure and Sleep Laboratory, Pulmonology Division, Hospital General de Agudos Enrique TornĂș, Buenos Aires, Argentina
https://doi.org./10.56538/ramr.XREG8277
Correspondencia :Ramiro H. Rojas Mendiola, email: rhrojasmd@gmail.com
ABSTRACT
Introduction: Treatment with positive airway pressure is one of the cornerstones in
managing obstructive sleep apnea (OSA). However, access to the equipment and adÂherence
to their use are not easy to achieve. Objective: to evaluate the adherence of
patients from the public health system who receive continuous pressure devices
free of charge for the treatment of OSA.
Materials and methods: Patients diagnosed with OSA who received continuous posiÂtive airway
pressure (CPAP) devices between 2013 and 2018 through PAMI (Programa
de AtenciĂłn MĂ©dica
Integral, Medical Services Program) , Incluir Salud, and Cobertura Porteña de Salud were retrospectively evaluated.
Results: Patients from PAMI were older and had a lower score in the Epworth
scale. The delay between the consultation and the diagnosis was 1.4 ± 2.4
months. The time from the diagnosis until the equipment was provided was 10.2 ±
9.9 months. Patients from PAMI received the equipment faster (2.7 ± 2.5 months)
and were more adherent to follow-up visits. Adherence
to clinical follow-up visits in the first year was 46 %. Older patients with a
lower Epworth score and those using AutoCPAP had a
non-significant trend favoring this adherence. The objective adherence measured
by memory card or telemonitoring was 40 %. The higher
body mass index (BMI) was the only factor favorÂing objective adherence.
Conclusions: Overcoming the economic limitation to access the equipment does not
change the attitude towards adherence and follow-up.
Key words: Sleep Apnea; Obstructive, Continuous Positive Airway Pressure, Patient
Compliance
RESUMEN
IntroducciĂłn:
El
tratamiento con presiĂłn positiva es uno de los pilares del manejo de las apneas
obstructivas del sueño, sin embargo, el acceso a los equipos y la adherencia a
su uso no son fĂĄciles de lograr.
Objetivo:
Evaluar
la adherencia de los pacientes del sistema pĂșblico de salud que reÂciben
equipos de presiĂłn continua de forma gratuita para el
tratamiento de las apneas obstructivas del sueño.
Material
y métodos: Se
evaluĂł retrospectivamente a los pacientes con diagnĂłstico de apnea obstructiva
del sueño que recibieron equipos de CPAP entre 2013 y 2018 a través de PAMI,
Incluir Salud y Cobertura Porteña de Salud.
Resultados:
Los
pacientes de PAMI fueron de mayor edad y tenĂan un Epworth
mås bajo. La demora entre consulta y diagnóstico fue de 1,4 ± 2,4 meses. El
tiempo de diagnóstico a provisión del equipo fue de 10,2 ± 9,9 meses. Los
pacientes de PAMI recibieron los equipos mås råpido (2,7 ± 2,5 meses) y fueron
mĂĄs adherentes a las visitas de control. La adherencia a los controles clĂnicos
el primer año fue del 46 %. Los pacientes de mayor edad, con Epworth mĂĄs bajo y que usan auto-CPAP tenĂan una tendencia
no significativa a favorecer esta adherencia. La adherencia objetiva medida por
tarjeta de memoria o telemonitoreo fue del 40 %. El
mayor IMC fue el Ășnico factor que la favorecĂa.
Conclusiones:
Superando
la limitaciĂłn econĂłmica al acceso a los equipos, no cambia la actitud hacia la
adherencia y control.
Palabras
clave: Apneas
del sueño; PresiĂłn positiva continua en la vĂa aĂ©rea; Adherencia
Received :11/08/2022
Accepte:11/24/2023
INTRODUCTION
Obstructive sleep apnea (OSA) is
defined by the presence of recurrent episodes of apneas or hyÂpopneas secondary
to pharyngeal collapse during sleep, leading to desaturations and
micro-arousals. When these events are associated with a set of signs and
symptoms, they constitute the obstrucÂtive sleep apnea-hypopnea syndrome
(OSAHS). The traditionally accepted prevalence of OSAHS in the general
population is 3.1 to 7.5 % in men and 1.2 to 4.5 % in pre-menopausal women.
However, recent epidemiological studies describe an even higher prevalence. 1
Taking into account the population
data in Argentina, in 2010, there were 40,117,096 inhabÂitants, 91 % of whom lived in urban areas, with a male/female ratio of
0.95/1. Approximately 65 % of the population is concentrated in the Central
region, especially in the province of Buenos Aires, which accounts for 38.9 %
of the countryâs populaÂtion, particularly in the Autonomous City of BueÂnos
Aires (CABA) and its surroundings.
The Argentinian Healthcare System
is made up of national and provincial ministries, as well as a network of
public hospitals and health centers that provide free care to anyone in need,
particularly those in the lowest income quintiles, without social security or
without the capacity to pay for health services. In the city of Buenos Aires,
the population that has public health coverage, without resources or through
the Cobertura Porteña
de Salud (CPS, Buenos Aires Health Coverage)
provided by the Government of CABA, represented 18.7 % during the year 2017.
The population with social health insurance (Obra
Social) was 46.1 %, prepaid health care plan, 28 %, and coverage from other
systems 7.2 %.3 Additionally,
the National Institute of SoÂcial Services for Retirees and Pensioners
(INSSJP), through the Medical Services Program (PAMI), provides coverage to
retirees of the national welÂfare system and their families, reaching 20 % of
the population, with an expenditure that accounts for 0.75 % of the GDP.4
Individuals with pension benefits
or disability pension receive coverage from the National GovÂernment (formerly
PRO.FE, currently Incluir Salud) and also seek diagnosis and follow-up care at
hospitals in CABA.
At the Hospital Enrique TornĂș, an average of 235,500 patients consulted the
Diagnostic Services per year, from 2013 to 2018. The Sleep and ReÂspiratory
Failure Laboratory receives 600 annual consultations from patients without
coverage, members of PAMI, and those with social health insurance coverage.
Our objective is to describe the
hospitalâs situÂation regarding patients with state coverage that addresses
economic limitations, a key aspect of access to treatment.
MATERIALS AND METHODS
This is a descriptive
retrospective study of patients with coverage from PAMI, Incluir
Salud, and CPS who were diagnosed with OSAHS
between 2013 and 2018 and were able to access treatment with continuous airway
pressure (CAP) devices, either CPAP, Auto CPAP, or BiPAP
(bilevel positive airway pressure). Patients who
purchased their own devices and those with social health insurance were
excluded.
Data were obtained from the
medical records of patients older than 18 years who first consulted during this
period and were diagnosed with OSA either through polygraphy
or polysomnography, and initiated treatment with PAP
devices. As it is a referral center, some patients come to the consultation
with the study already performed. Data were collected on sex, age, Body Mass
Index (BMI), neck circumference (NC), and daytime sleepiness using the Epworth
Sleepiness Scale (ESS).
Polygraphy studies were conducted using two different devices. The first is a Resmed Apnea LinkÂź
device that records airflow signals through a nasal pressure
cannuÂla, snoring derived from a nasal cannula, oximetry,
and pulse frequency. The signal analysis is performed using ApneaLink
software version 8 with automatic analysis and subsequent manual review. The
second device is an Embla Embletta
GoldÂź model that records airflow signals through a nasal pressure
cannula, snoring derived from a nasal canÂnula, thoracic and abdominal movement
using XactTraceÂź RIP (Respiratory
Inductance Plethysmography) belts, pulse oximetry, and body position. The signals are evaluated
using RemLogic-E software version 1.3 with automatic
analysis and manual review of events. For polysomnography
studies, an ATI Praxis18 AMP18P - Lermed S.R.L.
device is used. In each study, three EEG (electroencephalogram) channels were
recorded: 3, C4, and O1 with references on the mastoids (A1 and A2), two EOG (electrooculogram) channels (right and left), three EMG
(electromyogram) channels, ECG (electrocardiogram), airflow measurement through
thermistor and nasal pressure cannula, piezoelecÂtric thoracic and abdominal
bands for effort, body position sensor, pulse oximetry,
and a microphone. The records are manually analyzed using DelphosDB
software version 1.75.32.4 (Lermed S.R.L.) according
to the standards of the American Association of Sleep Medicine (AASM).7
The calibration procedure is
performed with polysomnoÂgraphic control or during 3
nights at home in order to reduce equipment ordering times. The devices used
for calibration are: REMstar auto with Aflex (Philips-Respironics) and
S9 (Resmed). Once the calibrations are completed, an
effective treatment pressure is established by the deviceâs software, as
effective pressure (P) during 90 or 95 % of the approÂpriate device usage time,
with system leaks of less than 24 liters/minute. Finally, the type of device is
noted, whether it has fixed pressure (CPAP), automatic variable pressure (AutoCPAP), or bilevel pressure (BiPAP).
The next step is the equipment
request. For patients without coverage, a form is completed that evaluates the
clinical and social situation to qualify for a request as Medical aid. Under
this designation, a request number is generated, categorized as âHospital
Supplyâ in the FinanÂcial Management and Administration Integrated System of
the Ministry of Health of the Government of CABA, where the resource provided
by the Ministry is directly available. Based on the availability of funds, a
bidding process is initiated with the submission of proposals from equipment
suppliers. Technical support is provided by the sleep laboÂratory doctors
according to each patientâs requirements. Upon confirmation of the final
amount, the equipment purchase is made, and the device is delivered to the patient
from 2 months on. In cases of urgent equipment provision, the administrative
resource of Emergency Purchase can be used, resulting in equipment acquisition
within one month. This administrative model has been in operation since 2016.
Between 2013 and 2016, a similar procedure was followed, but there were some
variations in supply times due to administrative issues beyond our control.
For PAMI patients, a specific
supply form is completed; it must then be renewed every 6 months. The bidding
process of the equipment is carried out for each patient, in every INSSJP
agency, depending on the patientâs address.
After the equipment is delivered,
a sleep laboratory doctor explains the basic care aspects of the equipment, he/she tests the mask, and checks the proper
functioning of the equipment. Follow-up visits are scheduled according to
national guidelines, one month after the beginning of treatment, at 3 months,
and then every 6 months. A contact phone number is provided for difficulties
that could arise between scheduled consultations.
The mean times that were
evaluated include: from consultation to diagnosis, from previous studies until
conÂsultation, from equipment request until provision, from equipment provision
until the first follow-up visit, and follow-up in the last 12 months. Adherence
to treatment was also evaluated basing on the presence or absence of a
follow-up visit one year after equipment delivery, the subjective use of
devices without memory, the objective use of devices with compliance memory
card, and the use in patients undergoing telemedicine.
Differences were analyzed between
adherents and non-adherents to follow-up visits, regardless of their equipment
provision method. In the subgroup of patients monitored with memory card or
telemedicine, differences were sought between those with more than 70 %
adherence and those without.
Patients who do not attend
scheduled follow-up visits during the last year are contacted to assess the use
of their equipment.
Statistical analysis
The data were collected in Excel
spreadsheets and processed using the EPI Info 7 program. The data are described
with measures of central tendency and dispersion according to the type of variable.
Differences between categorical variables were compared using the chi-square
test,2 and
continuous variables were analyzed using the Studentâs t-test. A p-value of
less than 0.05 was considered significant.
RESULTS
The data of 148 patients were
evaluated. A first group of 84 patients received the equipment from the
Government of the City of Buenos Aires and the National Government, referred to
as the Hospital Group (HG); and a second group of 64 patients with health
coverage received the equipment through the Social Services System for Retirees
and Pensioners and were called the PAMI group.
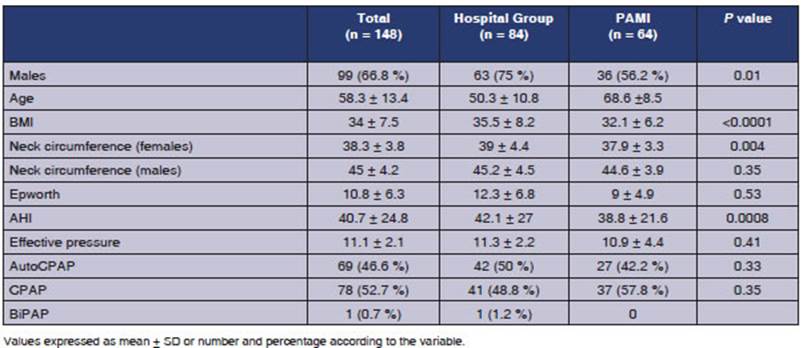
The characteristics of the
patients are presented in Table 1. The waiting times for diagnosis,
treatÂment, and follow-up are presented in Table 2.
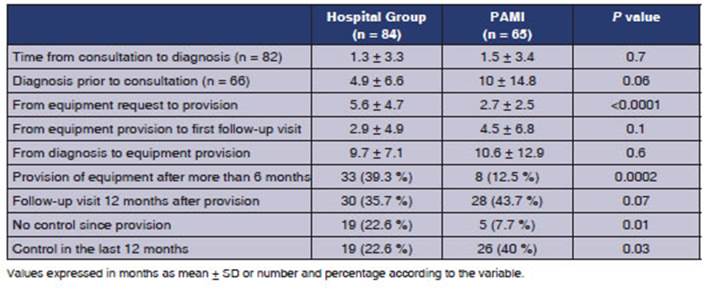
Values expressed in months as
mean ± SD or number and percentage according to the variable
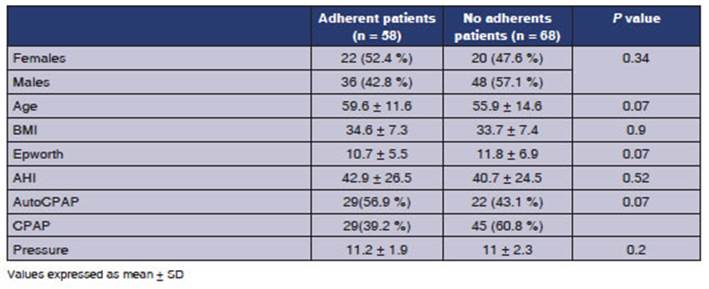
In a sub-analysis, patients who
had not yet completed 1 year of treatment by the statistical cutoff date were
excluded. Those who attended follow-up visits during the first year were
grouped as adherents. This group was compared with the remaining patients in order
to identify factors favoring adherence. Results are presented in Table 3.
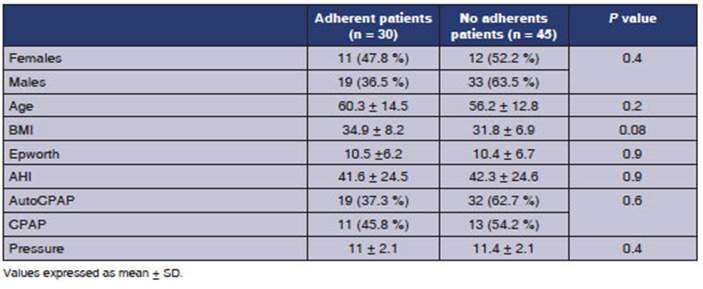
The objective adherence in
patients who had memory cards or were monitored through the cloud, defined as more
than 70 % of use for more than 4 nights per week, was only 40 %, with no
statistically significant differences between adherÂent and non-adherent
patients in the analyzed variables. Table 4.
91 patients who hadnât attended
any follow-up visit in the last year were contacted: 51.6 % reÂported that they
were still using the CPAP; 6.6 % had returned the device due to intolerance;
3.3 % had the device but werenât using it; and 38.5 % of patients couldnât be
located.
DISCUSSION
Our study found that
patients from the Hospital Group (HG) are younger but have a higher BMI and
higher levels of daytime sleepiness according to the Epworth Sleepiness Scale.
The age differÂences between groups are due to the fact that patients from the
PAMI group are mostly retired individuals, while the HG group consists of
middle-aged patients. Lee et al observed that the BMI does not correlate with
the apnea/hypopnea index (AHI) in patients older than 70 years.11 AdditionÂally, the Sleep Health Heart Study showed that
correlation and also demonstrated that sleepiness is less prevalent in elderly
patients compared to middle-aged individuals.12
In our study, the
delays in the access to the diagÂnostic study were 1.4 months. Access to
diagnostic procedures is deficient worldwide. A review on this topic in 2004
found significant variability among the analyzed countries, with Belgium having
the shortest waiting time, with average delays ranging from 2 weeks to 2
months. In the United States, significant differences are observed between cenÂters
and hospitals, with average waiting times ranging from 2 weeks to 9 months. In
other counÂtries, such as the United Kingdom, the average is 4 months; in Australia,
5 months, and in Canada, 24 months. It is important to note that there are
differences within each country, with Ontario, for example, having a waiting
time of only 2 months.13
The use of continuous airway
pressure devices is considered the standard treatment for patients with
moderate to severe OSAHS. UnderstandÂing the obstacles and difficulties in
accepting and adhering to CPAP is crucial for an effective treatment and the
development of an adherence protocol.
Access to the
equipment is the first barrier to treatment. A recent study in six Latin
American countries showed that 28.7 % of the patients who could not initiate
CPAP treatment lacked economic resources to purchase the equipment.14
In Mexico, Torre B. et al observed that 45 % of patients with a CPAP
prescription failed to acquire the equipÂment, considering the economic aspect
an essential causal factor.15 Through economic incentives for
patients with low socioeconomic status, CPAP acceptance rates of 70 % were
achieved.16 The Argentinian public healthcare system enables all
patients diagnosed with OSAHS to access the equipment. However, in our study,
treatment adherence during the first year was only 39 %, similar to the
findings by Tarasiuk et al (35 to 39 %).16 Another study in Belgium demonstrated that CPAP acceptance
was higher when there was economic reimbursement from social security, but
found no differences with regard to adherence and compliance after more than 2
years of follow-up.17
There are few studies
about delays in treatment initiation. A cohort study in Ontario with 216,514
patients who started CPAP treatment between 2006 and 2013 showed a mean delay
of 138 +/- 202 to 196 +/- 238 days since the diagnosis in hospital sleep
laboratories versus 119 +/- 167 to 150 +/- 202 days in community sleep
laboratories, with 33.6 % of patients taking more than 6 months to receive the
equipment.18 Our study has a much smaller sample size, but we
obtained provision times of 130.4 +/- 130.9 days, with shorter times in the
PAMI system and only 12.2 % of patients taking more than 6 months to receive
the equipment.
In a systematic
literature review from 1994 to 2015 about CPAP adherence, an average usage rate
of 36.3 % was observed with a mean use of 4.6 hours per night that did not
improve over time.19 Baratta et al found
that adherence to the use of CPAP for more than 4 hours per night and more than
5 days per week was 41.4 %, with an average follow-up of 74.8 months.20
This value is similar to what was found in our group of patients with objective
CPAP adherence. In contrast, a study conducted in Denmark with 695 patients who
received a free AutoCPAP under a strict follow-up
protocol achieved compliance rates of 77.7 %, with an average follow-up of 3
years, showing higher adherence in severe patients. Furthermore, they found
that the severity of the OSAHS, daytime sleepiness, and smoking are independent
factors for treatment adherence.21 Kohler et al evaluated long-term
follow-up at the Oxford Centre for Respiratory Medicine, and found 81 % adherence
at 5 years, and 70 % at 10 years, with an mean use of 6.2 hours per night, with
the desaturation index being the only factor favoring long-term adherence in
the multivariate analysis.22 In the study by Santin
et al, it was observed that 60.5 % of patients continued using CPAP at an
average of 12.3 months of follow-up, with age, Epworth Scale score, and AHI
being the factors favoring long-term adherence.23 Torre B. et al
reported an 80 % adherence to CPAP at 34 months post-prescription, which was related
to a higher respiratory distress index (RDI).15 Our study found that
age, the EpÂworth Scale score, and the use of AutoCPAP
over the CPAP had a non-significant trend in favor of adherence to follow-ups,
while the increased BMI was the only factor showing a non-significant trend
toward improving objective adherence. These findÂings lack statistical
significance, probably due to the smaller number of patients.
There should be an
initial consultation with a specialist before the start of treatment, followed
by frequent visits to a specialist nurse in the field of sleep disorders for
adjustments in the CPAP combination, the mask type, and the use of huÂmidification
(if deemed necessary), until patient tolerance is achieved. Subsequently, there
should be follow-up visits at least once a year.21
The decision of
patients to sleep in another room has been shown to be a predictor CPAP
treatment acceptance.24 This suggests that
eduÂcating the patientâs partner and family environment is important to maintain
good adherence. In a systematic review by Cochrane, low-quality evidence was
found regarding individual support interventions (frequent consultations, phone
calls, telemedicine, home visits, and group meetÂings for patients) and
behavioral therapy (face-to-face or online motivational interviews) to improve
the use of CPAP; and there is moderate-quality evidence for in-person or
distance educational interventions.25
CPAP equipment
providers can play a crucial role in the treatment of sleep apnea by helping
patients to select the most suitable devices and masks and providing training
on proper usage. In a study conducted in Germany, the equipment provider
company evaluated the use of a patient support tool. This tool provided
personalized eduÂcation on the use of the mask,
the humidifier and overall device usage. Additionally, the company offered
usage tips and encouraging messages, all tailored to
the device usage data. These intervenÂtions resulted in improvements in the
number of hours of use, reduced leakage, and lower rates of treatment
withdrawal.26
CONCLUSIONS
With the data obtained in our
analysis, we found significant delays in accessing the diagnosis of OSA and
treatment with CPAP. These delays are longer in patients without medical coverage
compared to those with PAMI coverage. Adherence to CPAP use is still low even
after overcoming economic limitations in the access to treatment equipment.
Age, the baseline Epworth score, and the use of auto-adjustable deÂvices would
favor treatment adherence. More interventions from various healthcare system
stakeholders are needed to achieve optimal use of CPAP equipment and obtain all
the benefits of treatment.
Conflict of interest
Authors have no conflict of
interest to declare in relation to the topic of this manuscript. This work
was carried out without funding.
REFERENCES
1. Nogueira FB, Cambursano H, Smurra M, et al. GuĂas prĂĄcticas de diagnĂłstico y
tratamiento del sĂndrome de apneas e hipopneas
obstructivas del sueño: Actualización 2019. Rev Am Med Resp. 2019;19:31.
2. Jonas DE, Amick HR, Feltner C, et al.
Screening for Obstructive Sleep Apnea in Adults: Evidence Report and Systematic
Review for the US Preventive Services Task Force. JAMA.
2017;317:415-33. https://doi.org/10.1001/jama.2016.19635
3. Peppard PE, Young T, Barnet JH, et al. Increased prevalence
of sleep-disordered breathing in adults. Am J EpideÂmiol. 2013;177:1006-14.
https://doi.org/10.1093/aje/kws342
4. Redline S, Sotres-Ălvarez D, Loredo J, et
al. Sleep-disordered breathing in Hispanic/Latino individuals of diverse
backgrounds. The Hispanic Community Health Study/ Study of
Latinos. Am J Respir Crit Care Med, 2014:189:335- 644.
https://doi.org/10.1164/rccm.201309-1735OC
5. Simpson L, Hillman
DR, Cooper MN, et al. High prevalence of undiagnosed obstructive sleep apnoea in the general population and methods for screening
for repreÂsentative controls. Sleep Breath. 2013;17:967-73.
https:// doi.org/10.1007/s11325-012-0785-0
6. Arnardottir ES, Bjornsdottir E, Olafsdottir KA, et al. Obstructive sleep apnoea in the general population: highly prevalent but
minimal symptoms. Eur Respir
J. 2016;47:194-202.
https://doi.org/10.1183/13993003.01148- 2015
7. Shahar E, Redline S, Young T, et al. Hormone replacement
therapy and sleep-disordered breathing. Am J Respir Crit Care Med. 2003;167:1186-92.
https://doi.org/10.1164/rccm.200210-1238OC
8. Argentina, INdEyCR. Censo 2010. 2010;
Available from:
https://www.indec.gob.ar/nivel4_default.asp?id_
tema_1=2&id_tema_2=41&id_tema_3=135.
9. Arce HE. OrganizaciĂłn y financiamiento del sistema de salud en
la Argentina [The Argentine
Health System: organization and financial features]. Medicina (B Aires). 2012;72:414-8.
10. (Argentina), MdS. El acceso a la
salud en Argentina: III encuesta de utilizaciĂłn y gasto en servicios de salud
2010. 2010; Available from:
http://www.msal.gob.ar/fesp/images/stories/recursos-de-comunicacion/publicaciones/estudio_carga_enfermedad.pdf.
11. Lee YG, Lee YJ, Jeong DU. Differential Effects of Obesity on Obstructive
Sleep Apnea Syndrome according to Age. Psychiatry Investig. 2017;14:656-61.
https://doi.org/10.4306/pi.2017.14.5.656
12. Young T, Shahar E, Nieto FJ, et al. Predictors of sleep-disordered
breathing in community-dwelling adults: the Sleep Heart Health Study. Arch
Intern Med. 2002;162:893- 900.
https://doi.org/10.1001/archinte.162.8.893
13. Flemons WW, Douglas NJ, Kuna ST, et al. Access to diagnoÂsis
and treatment of patients with suspected sleep apnea. Am J Respir Crit Care Med. 2004;169:668-72.
https://doi.org/10.1164/rccm.200308-1124PP
14. Nogueira JF, Poyares D, Simonelli G, et al., Accessibility and adherence to
positive airway pressure treatment in patients with obstructive sleep apnea: a
multicenter study in Latin America. Sleep Breath. 2020;24:455-64.
https://doi.org/10.1007/s11325-019-01881-9
15. Torre Bouscoulet L, LĂłpez EscĂĄrcega
E, Castorena MalÂdonado A, VĂĄzquez GarcĂa JC, Meza Vargas MS, PĂ©rez- Padilla R.
Uso de CPAP en adultos con sĂndrome de apneas obstructivas durante el sueño
despuĂ©s de prescripciĂłn en un hospital pĂșblico de referencia de la Ciudad de
MĂ©xico [Continuous positive airway
pressure used by adults with
obstructive sleep apneas after prescription in a public referral hospital in Mexico City]. Arch Bronconeumol. 2007;43:16-21. https://doi.org/10.1157/13096996
16. Torre Bouscoulet L, LĂłpez EscĂĄrcega
E, Castorena MalÂdonado A, VĂĄzquez GarcĂa JC, Meza Vargas MS, PĂ©rez- Padilla R.
Uso de CPAP en adultos con sĂndrome de apneas obstructivas durante el sueño
despuĂ©s de prescripciĂłn en un hospital pĂșblico de referencia de la Ciudad de
MĂ©xico [Continuous positive airway
pressure used by adults with
obstructive sleep apneas after prescription in a public referral hospital in Mexico City]. Arch Bronconeumol. 2007;43:16-21.
https://doi.org/10.1157/13096996
17. Leemans J, Rodenstein D, Bousata J, Mwenge GB. Impact of
purchasing the CPAP device on acceptance and long-term adherence: a Belgian
model. Acta Clin Belg. 2018;73:34-9. https://doi.org/10.1080/17843286.2017.1336294
18. Rotenberg B, George
C, Sullivan K, Wong E. Wait times for sleep apnea care
in Ontario: a multidisciplinary assessment. Can Respir
J. 2010;17:170-4. https://doi.org/10.1155/2010/420275
19. Rotenberg BW, Murariu D, Pang KP. Trends in CPAP adÂherence over twenty
years of data collection: a flattened curve. J Otolaryngol
Head Neck Surg. 2016;45:43.
https://doi.org/10.1186/s40463-016-0156-0
20. Baratta F, Pastori D, Bucci T, Fabiani M, Fabiani V, Brunori M, et al.
Long-term prediction of adherence to continuous positive air pressure therapy
for the treatment of moderate/severe obstructive sleep apnea syndrome. Sleep
Med. 2018;43:66-70.
https://doi.org/10.1016/j.sleep.2017.09.032
21. Jacobsen AR, Eriksen F, Hansen RW, et al. Determinants for adherence to
continuous positive airway pressure therapy in obstructive sleep apnea. PLoS One.
2017;12:e0189614.
https://doi.org/10.1371/journal.pone.0189614
22. Kohler M, Smith
D, Tippett V, Stradling JR.
Predictors of long-term compliance with continuous positive airway pressure. Thorax. 2010;65:829-32.
https://doi.org/10.1136/thx.2010.135848
23. SantĂn M J, Jorquera A J, JordĂĄn J,
et al. Uso de CPAP nasal en el largo plazo en sĂndrome de apnea-hipopnea del sueño [Long-term continuous positive airway presÂsure (CPAP) use in obstructive
sleep apnea]. Rev Med Chil. 2007;135:855-61.
https://doi.org/10.4067/S0034-98872007000700005
24. Kiely JL, McNicholas WT. Bed partnersâassessment of nasal continuous positive airway
pressure therapy in obstructive sleep apnea. Chest.
1997;111:1261-5. https://doi.org/10.1378/chest.111.5.1261
25. Wozniak DR, Lasserson TJ, Smith I. Educational, supportive and behavioural interventions to improve usage of continuous
positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst
Rev. 2014:CD007736. https://doi.org/10.1002/14651858.CD007736.pub2
26. Woehrle
H, Arzt M, Graml A, et al.
Effect of a patient engagement tool on positive airway pressure adherÂence:
analysis of a German healthcare provider dataÂbase. Sleep Med. 2018;41:20-6.
https://doi.org/10.1016/j.sleep.2017.07.026