Autor : Cafaro, Mario A.1, Benavidez Rodrigo A.2, Yaryura Montero José G.3, Navarro Ricardo4
1Staff Surgeon of the Thoracic Surgery Service. Sanatorio Allende, CĂłrdoba city, capital of the Province of CĂłrdoba, Argentina. 2Chief of the Thoracic Surgery Service. Sanatorio Allende, CĂłrdoba city, capital of the Province of CĂłrdoba, Argentina. 32nd year Resident of the Thoracic Surgery Service. Sanatorio Allende, CĂłrdoba city, capital of the Province of CĂłrdoba, Argentina. 4Consultant Surgeon of the Thoracic Surgery Service. Sanatorio Allende, CĂłrdoba city, capital of the Province of CĂłrdoba, Argentina.
https://doi.org/10.56538/ramr.YZBD4253
Correspondencia :Mario Cafaro E-mail: mariocafaro.t@gmail.com
ABSTRACT
Introduction: The disease caused by SARS-CoV-2 has become a significant public health
issue. 5 % of the patients required endotracheal intubation due to acute hypoxÂemic
respiratory failure, leading to an increased number of consultations for
tracheal stenosis. This work was done with the aim of presenting the results of
tracheal resection in patients with post-COVID-19 stenosis.
Material and methods: Analytical, prospective, observational study. 11 patients were included.
The preoperative and postoperative evaluation was the same for all patients.
Post-surgical ventilation and phonation were assessed up to 30 days. The Clavien and Dindo classification
was used to grade post-surgical complications, with follow-up extended up to 60
post-surgical days. Statistical analysis: the Wilcoxon test was used to compare
the results.
Results: 27.2 % of the patients had postoperative complications. The comparison
of pre- and postoperative ventilation (p < 0.05) was statistically
significant, with improveÂment in the postoperative period. When comparing pre-
and postoperative fiberoptic bronchoscopy (tracheal
lumen diameter), the result was also statistically significant (p < 0.05).
Conclusion: The results obtained are similar to those expressed in the literature.
TraÂcheal resection is a safe and effective procedure and should be considered
as first-line treatment for tracheal stenosis.
Key words: Coronavirus, Tracheal stenosis, Intubation, Intratracheal,
Thoracic surgery
RESUMEN
IntroducciĂłn:
La
enfermedad por SARS-CoV-2 se convirtiĂł en un importante problema de salud
pĂșblica. El 5 % de los pacientes requiriĂł intubaciĂłn endotraqueal
por insuficienÂcia respiratoria aguda hipoxĂ©mica, y
se generĂł un aumento de consulta por estenosis traqueal. Se realizĂł el trabajo
con el objetivo de expresar los resultados de la cirugĂa de resecciĂłn traqueal
en pacientes con estenosis post COVID 19.
Material
y métodos: Estudio
prospectivo, observacional, analĂtico. Se incluyeron 11 pacientes. La
evaluaciĂłn prequirĂșrgica y postquirĂșrgica fue la
misma en todos los pacientes. Se valorĂł en el postquirĂșrgico la ventilaciĂłn y
la fonaciĂłn hasta los 30 dĂas. Se utilizĂł la clasificaciĂłn de Clavien y Dindo para calificar a
las complicaciones posÂtquirĂșrgicas, con seguimiento hasta los 60 dĂas
postquirĂșrgicos. AnĂĄlisis estadĂstico: se aplicĂł prueba de Wilcoxon
para comparar los resultados.
Resultados:
El
27.2 % de los pacientes tuvieron complicaciones postquirĂșrgicas. Fue
estadĂsticamente significativa la comparaciĂłn de la ventilaciĂłn entre el prequirĂșrgico y el postquirĂșrgico (p<0.05) con mejorĂa
en el postquirĂșrgico. Al comparar la fibrobronÂcoscopĂa
prequirĂșrgica con la postquirĂșrgica (diĂĄmetro de la
luz traqueal) tambiĂ©n el resultado fue estadĂsticamente significativo (p
<0.05).
ConclusiĂłn:
Los
resultados obtenidos son similares a los expresados en la literatura. La
cirugĂa de resecciĂłn traqueal es un procedimiento seguro y efectivo y debe ser
considerada como tratamiento de primera lĂnea para la estenosis traqueal.
Palabras
claves: Coronavirus,
Estenosis Traqueal, IntubaciĂłn, Intratraqueal,
CirugĂa TorĂĄcica
Received: 07/07/2023
Accepted: 12/02/2023
INTRODUCTION
The disease caused by SARS-CoV-2
(COVID-19) spread rapidly worldwide and has become a sigÂnificant public health
issue. The first case was reported in 2019. This led to an unprecedented
increase in the number of patients requiring proÂlonged stays in the Intensive
Care Unit (ICU) due to respiratory complications caused by COVID-19. 5 % of
these patients required endotracheal inÂtubation and mechanical ventilation for
acute hypoxemic respiratory failure.1, 2
While orotracheal
intubation (OTI) is an esÂsential tool for the management of patients in the
intensive care unit, one of the complications it can generate is tracheal
stenosis. Although the incidence is low at present, thanks to applied new
technologies, it still exists. These advances began to be used after research
conducted by Grillo and Cooper in 1966,3 where they
determined the physiopathology of tracheal stenosis. The rate of laryngotracheal stenosis postintubation
(LSPI) in non-COVID-19 patients is between 10 and 22 %.4, 5 Although the rate of LSPI related to COVID-19
is still unknown, it is believed that this complicaÂtion is even more common.6 This could
possibly be due to the debate regarding the timing of the tracheostomy that
took place at the beginning of the pandemic (due to the risk of virus aerosolizaÂtion), leading to many cases being performed
late.7
We present the experience in
managing a series of consecutive patients who underwent surgical treatment.
OBJECTIVES
Primary
To assess the results
of the surgery in relation to ventilation and phonation.
Secondary
1. To determine surgery-related
morbidity and mortality according to the Clavien Dindo scale.
2. To compare our results with
those of the series of patients (with and without COVID-19) menÂtioned in the
literature.
MATERIALS AND METHODS
An analytical, prospective,
observational study was conÂducted. A database was created, including the
patients who underwent tracheal resection with primary anastomosis at the Sanatorio Allende, New CĂłrdoba and Cerro branches (CĂłrdoba
city, capital of the Province of CĂłrdoba, Argentina) between August 2021 and
September 2022.
All patients signed an informed
consent prior to surgery.
The study was reviewed and
approved by the Ethics Committee of the Sanatorio
Allende.
Inclusion criteria
âą Patients of both sexes, aged 16
and older, diagnosed with complex central airway stenosis following prolonged
intubation with mechanical respiratory support as a treatment for COVID-19.
Exclusion criteria
âą Patients with tracheal stenosis
greater than 5 centimeÂters and/or with general contraindications for surgical
treatment.
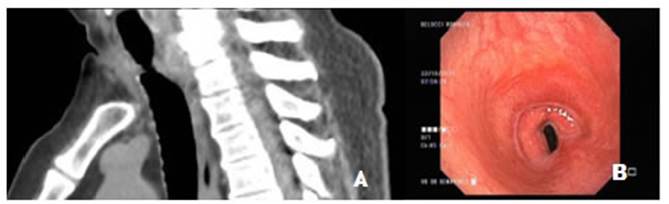
All the patients had a standard evaluation.
They unÂderwent axial, coronal and sagittal computed tomography scans (CT) and
flexible fiberoptic bronchoscopy (FFB). With the CT
and FFB results, both the length and location of the stenosis were determined.
A complex tracheal stenosis is considered
to be one exceÂeding 1 cm in length and with involvement of the tracheal wall.
Cases were classified according to the Myer-Cotton classification.8
In patients where the stenosis
affected the cricoid cartiÂlage, laryngotracheal
resection was considered.
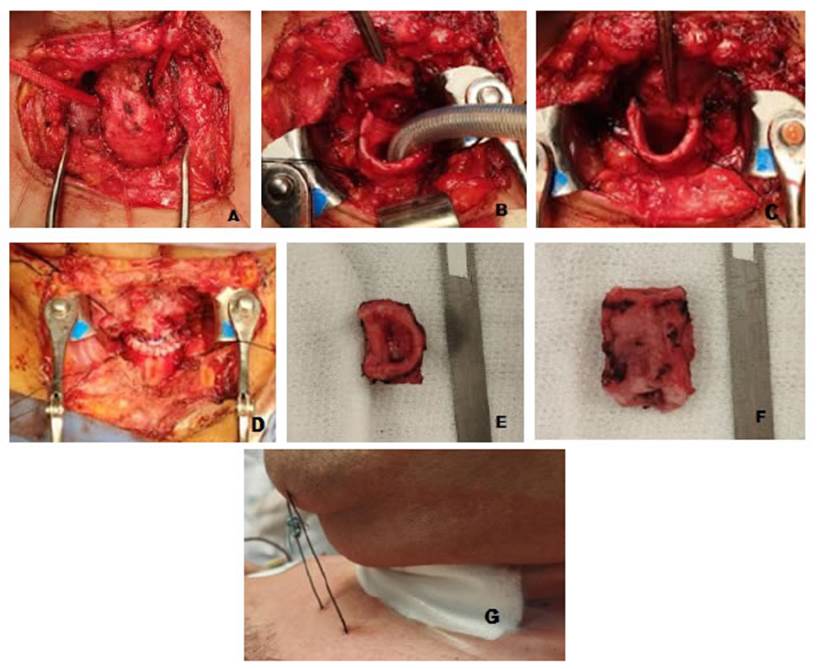
The surgical technique is similar
to that described by Mathisen9 with a few
modifications.
To the patient with tracheoesophageal fistula, closure of the opening on the
anterior face of the esophagus was perÂformed using 3.0 silk sutures on the mucosa
and muscular layers separately. Regarding anesthesia, all patients receiÂved
either inhalation gas or total intravenous anesthesia. In patients with severe
tracheal stenosis, tracheal dilation was performed prior to the placement of
the orotracheal tube. At the end of the surgery, the
patients were extubated.
To assess ventilation and
phonation, patients were evaÂluated at 7 days, 15 days, and 30 days
post-surgery.
Ventilation was assessed basing
on the presence or abÂsence of stridor in the postoperative period.
Phonation was assessed basing on
the presence or absÂence of dysphonia in the postoperative period.
The Clavien
and Dindo classification was used to grade
postoperative complications, with follow-up extended up to 60 days.
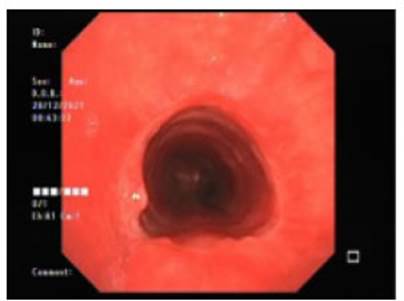
A new FFB was conducted on all
patients after 30 days to evaluate the status of the anastomosis.
Statistical analysis
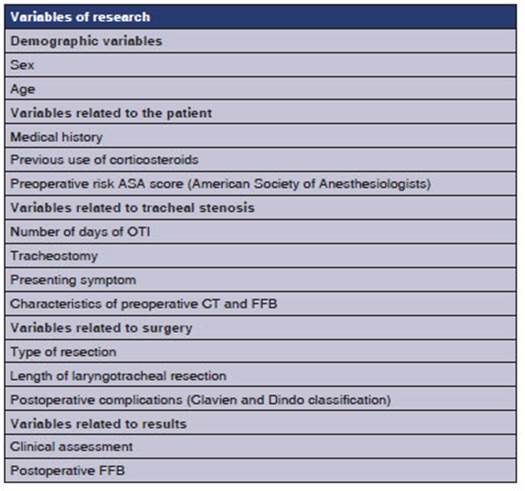
All the variables in research
were expressed in percentages, maximum, minimum, and median.
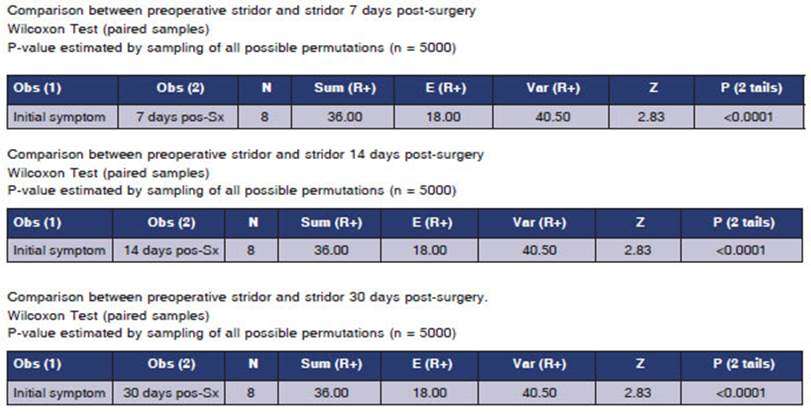
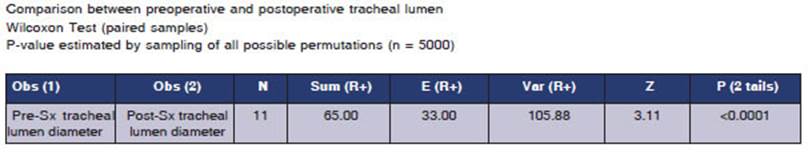
The Wilcoxon test was used to
compare the presence or absence of stridor on days 7, 14, and 30 after surgery
in patients who presented stridor as initial symptom, consiÂdering a p-value
< 0.05 as statistically significant.
The Wilcoxon test was also
applied to compare preoperaÂtive and postoperative fiberoptic
bronchoscopy, taking into account whether the postoperative fiberoptic
bronchoscopy showed a preserved tracheal lumen diameter or not; the
statistically significant value was p < 0.05.
RESULTS
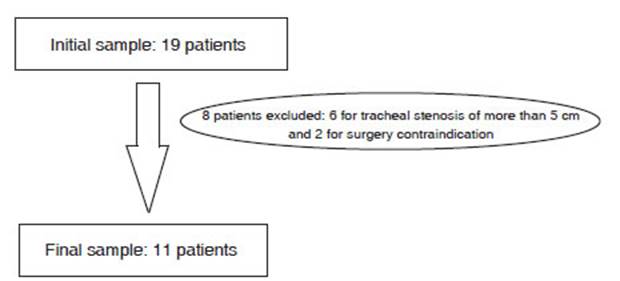
Out of the 19 initially evaluated
patients, 8 were excluded, resulting in a final sample size of 11 participants.
(Figure 1)
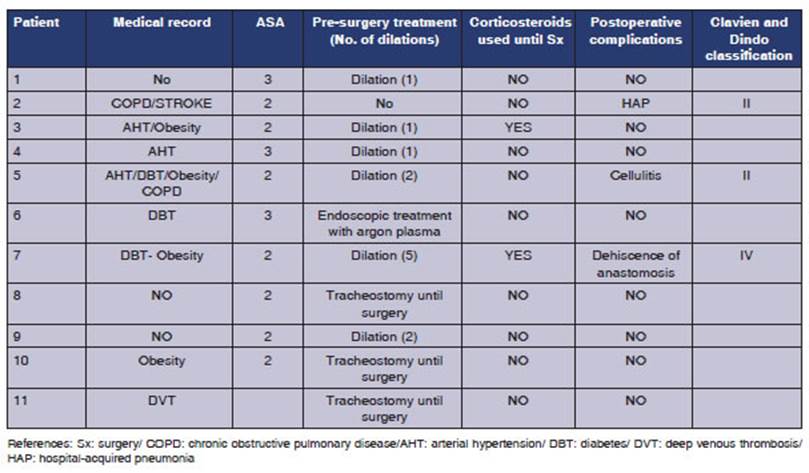
Of the included patients, 9 (81.8
%) were male, with a mean age of 52 years (MAX: 72 MIN: 32 MEDIAN: 47). Table 2
shows the medical record, surgical risk (ASA score), pre-surgery treatment,
history of corticosteroid use, and postoperative complications (Clavien Dindo classification).
27.2 % of the patients had postoperative complications.
Only one patient was
diagnosed with COVID-19 in the year 2020; the rest were diagnosed in 2021.
All the patients had
OTI, with an average of 13 days (MAX: 21 MIN: 8 MEDIAN: 12). 5 patients (45.4
%) underwent a tracheostomy. The average of days between the OTI and the
tracheostomy was 13 (MAX: 20 MIN: 9); and 3 patients (27.2 %) remained with the
tracheostomy until surgery; 2 of them due to total laryngotracheal
occlusion and the rest due to tracheoesophageal
fistula.
The presenting
symptoms and reasons for consultation were as follows: stridor and dyspnea
(36.3 %), stridor only (27.2 %), aphasia (18.1 %), stridor, dyspnea, and
dysphonia (9 %), and bronÂchoaspiration (9 %). The
results observed in the neck CT and FFB are detailed in Table 3.
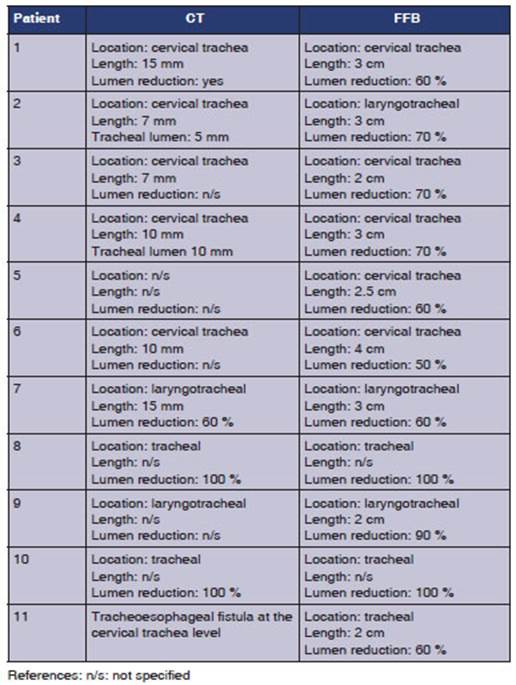

References: n/s: not
specified
According to the
Myer-Cotton classification, 8 patients were grade 2; 2 patients were grade 4,
and 1 patient was grade 3.
The average number of
months between the diagnosis of COVID-19 and tracheal resection surgery was 7
(MAX: 25 MIN: 2).
54.4 % of the
patients required at least one tracheal dilation prior
to surgery. One of the patients underwent endoscopic treatment using argon
plasma without the expected results before surgery.
Laryngotracheal resection was performed on 36.3 % of the patients,
and tracheal resection on 63.6 %.
The average duration
of surgery, measured in minutes, was 191 (MAX: 240 MIN: 120). The averÂage
hospital stay was 6 days (MAX: 7 MIN: 5). Onlyone patient required surgical reintervention
due to dehiscence of the anastomotic suture 47 days after surgery.
The average resection length
(measured in cm) was 2.9 (MIN: 1.5 MAX: 5).
There was no mortality at 60
days.
In the assessments at 7 and 14
days post-surÂgery, 5 patients showed dysphonia.
At the 30-day assessment, 4
patients experiÂenced dysphonia.
In the postoperative period,
endoscopic treatÂment with argon plasma was performed in only 1 patient for
granulomas at the anastomotic level.
Statistical analysis
Regarding the assessment of preoperative
stridor compared to the control at 7 days, no patients showed stridor; and the
same was observed at 14 days. Only one patient exhibited stridor at 30 days. In
this comparison, 8 patients were included, as 3 patients maintained the tracheÂostomy
until surgery, making the symptom unassessable.
The result of the comparison
between preoperaÂtive stridor and the assessment of the presence of this
symptom at 7, 14, and 30 days was statistically significant in all cases (p
< 0.05) (Table 4).
In the comparison between the
initial FFB and that of 30 days post-surgery, only one patient exÂhibited a
decrease in the diameter of the tracheal lumen. The result was statistically
significant (p > 0.05) (Table 5).
DISCUSSION
The approach to treat benign
tracheal stenosis is very complex, so it should be carried out in highly
experienced centers. It requires a trained team to do a proper evaluation and
determine the best treatment option, with tracheal resection and priÂmary anastomosis
being one of the choices.
There are very few studies in the
literature that show the results of tracheal surgery for benign stenosis, and
if we specifically focus on tracheal or laryngotracheal
resection for stenosis secondary to intubation from COVID-19, we find only two
studies, with the rest being case reports.
Regarding our results, the most
prevalent sympÂtom in the postoperative period was dysphonia, but it was mild
in all the cases, and it didnât prevent the patients from carrying out their
daily activities normally. Only one patient required endoscopic treatment
related to dysphonia, specifically due to granulomas on the vocal cords.
27.7 % of the
patients showed postoperative complications, with two being classified as mild
(Clavien Dindo II) and one
more severe: dehiscence of the anastomotic suture (Clavien
Dindo IV), which required emergency tracheostomy and
was a late complication, occurring 47 days post-surgery. This case was the
patient whose FFB showed a deÂcrease in the tracheal lumen 30 days
post-surgery. Upon analyzing the complications, it is observed that all three
patients were classified as ASA 3, and the patient with the most severe
complication continued using corticosteroids until the surgery and had
undergone 5 previous dilations. These are known risk factors for tracheal
resection surgery.10
The most common
presenting symptom was stridor, which was taken into account when assessÂing
ventilation in the postoperative period. When comparing the preoperative period
with control at days 7, 14, and 30 after surgery, the difference in the absence
of stridor was always statistically significant (p < 0.05), indicating the
positive outÂcomes of the surgery. The same trend was observed when comparing
the preoperative FFB with the one performed 30 days after surgery. The result
was also statistically significant (p < 0.05) for the preserved tracheal
lumen diameter in the postoperative period, which correlates with the absence
of stridor and underscores the success of the surgical treatment.
Piazzaâs work11 is the
only one in the literature showing the results of a case series involving
tracheal or laryngotracheal resection secondary to
tracheal stenosis caused by COVID-19. The number of patients treated in that
study is 14, very similar to our experience. The mean
age of the patients and the male-to-female ratio are also similar. In their
study, the mean duration of the OTI was 15.2 days, and a tracheostomy was
performed on 10 patients. In our work, the mean duration of the OTI was 13 days,
and a tracheosÂtomy was performed on 5 patients. Just like in our work, 3
patients arrived to the surgery with a tracheostomy.
With regard to the
location, in both studies, the most frequent location was the cervical trachea.
The most commonly performed procedure on patients before surgery was tracheal
dilation. In Piazzaâs work,11 the mean time
of hospitalization was 12.1 days, compared to 6 days in our study. They
documented a case of restenosis, whereas we had none in our study.
Another study that
shows results of tracheal surgery in patients with stenosis secondary to
prolonged intubation is the one from Palacios12. However, it
includes various tracheal procedures (tracheal resection, Montgomery T-tube
placeÂment, endoscopic treatment), and in the descripÂtion of the results, it
does not specify the technique that was used. The most frequently affected site
was the cervical trachea. According to the Myer- Cotton grading system, the
majority of the cases were grade III; in our work, the majority
were grade II.
The remaining
articles are related to tracheal surgery for tracheal stenosis but not
specifically associated with COVID-19.
Wrightâs work,10 evaluates the results of 392 patients
operated on at the Massachusetts General Hospital from 1993 to 2017. The mean
number of tracheal resections performed per year is 16.3; this figure aligns
with the significant number of patients included in our study. The study states
that the most common presenting symptoms are stridor, dyspnea, cough, and
dysphonia, very simiÂlar to those observed in our patients. In Wrightâs study,
92 % of patients received some form of treatment before surgery, compared to
63.6 % in our patient series. The mean length of tracheal resection was very
similar, with 3 cm in Wrightâs work and 2.9 cm in ours. The best outcomes were
obtained in patients without prior treatment for tracheal stenosis and without
prior use of corticoÂsteroids. That is why it is very important not to delay
the diagnosis.13
The overall morbidity
rate was 33 % in Wrightâs study versus 27.7 % in our work. There was dehisÂcence
of anastomosis in 4 % of Wrightâs patients compared to 9 % (1 patient) in our
series. Similar to our findings, in Wrightâs study there were no significant
differences between pure tracheal reÂsection and laryngotracheal
resection.
The study by Natuta14
reveals the results of 43 patients who underwent tracheal resection between
2007 and 2018, with a mean follow-up of 58 months. Similar to our findings, the
study did not report any deaths within the first 30 days. Dyspnea was measured
using the visual analogue scale for dyspnea, showing a noticeable improveÂment
in the postoperative period with statistically significant results. Regarding
voice assessment, it was determined that 30 patients experienced mild
deterioration.
The results presented
in the series of patients who underwent tracheal or laryngotracheal
resecÂtion for benign stenosis unrelated to COVID are
similar to those obtained in our study. This sugÂgests that this condition
should not significantly alter the treatment approach.
As for the
limitations of the study, it should be noted that the number of cases does not
allow for statistical analysis to relate variables studied in our work and
compare them with the results of non-COVID-19 patients.
CONCLUSION
The COVID-19 pandemic
posed a significant chalÂlenge for healthcare professionals worldwide. There
was a substantial increase in patient admissions to critical care units with the
need for OTI. Initially, due to concerns about virus aerosolization,
changes in guidelines were implemented, leading to delays in performing
tracheostomies. These factors conÂtributed to an increased rate of tracheal
stenosis.
For complex tracheal
stenosis, it is crucial to have a team with experience in tracheal surgery.
With appropriate indications, tracheal resection with primary anastomosis
should be considered the first option. In the hands of experienced surgeons, it
is a safe and effective procedure.
The postoperative
results in this series of paÂtients are similar to those with benign tracheal
stenosis unrelated to COVID-19.
A multicenter study
should be conducted to increase the number of cases and obtain more significant
results.
Conflict of interest
The authors declared
no conflict of interest
REFERENCES
1.
Guan WJ, Ni ZY, Hu Y, et
al. Clinical
characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708-20.
https://doi.org/10.1056/NEJMoa2002032
2. Wu Z, McGoogan
JM. Characteristics of and important lessons from the coronavirus disease 2019
(COVID-19) outbreak in China: summary of a report of 72314 cases from the
Chinese Center for Disease Control and PrevenÂtion. JAMA 2020;323:1239-42.
https://doi.org/10.1001/jama.2020.2648
3. Cooper J.D, Grillo H.C. The evolution of tracheal inÂjury due to ventilatory assistance through cuffed tubes: a pathologic
study. Ann Surg 1969;169:334-48.
https://doi.org/10.1097/00000658-196903000-00007
4. Cooper J. Tracheal Injuries
Complicating Prolonged IntubaÂtion and Tracheostomy. Thorac
Surg Clin 2018;28:139-44. https://doi.org/10.1016/j.thorsurg.2018.01.001
5. Nouraei
SA, Ma E, Patel A, et al. Estimating the population incidence of adult
post-intubation laryngotracheal stenosis. Clin Otolaryngol 2007;5:411-2. https://doi.org/10.1111/j.1749-4486.2007.01484.x
6. Alturk
A, Bara A, Darwish B. Post-intubation tracheal
stenosis after severe COVID-19 infection: A report of two cases. Ann Med Surg 2021;67:102468.
https://doi.org/10.1016/j.amsu.2021.102468
7. Piazza C, Filauro
M, Dikkers FG, et al. Long-term intubaÂtion and high
rate of tracheostomy in COVID-19 patients might determine an unprecedented
increase of airway stenoses: a call to action from
the European Laryngological Society. Eur Arch Otorhinolaryngol 2021;278:1-7.
https://doi.org/10.1007/s00405-020-06112-6
8. Miller R, Murgu
S. Evaluation and Classifications of Laryngotracheal
Stenosis. Rev Am Med Resp. 2014; 4:344-57.
9. Mathisen
D. Tracheal Resection and Reconstruction: How I Teach It. Ann Thorac Surg 2017;103:1043-8.
https://doi.org/10.1016/j.athoracsur.2016.12.057
10. Wright CD, Li S, Geller AD,
et al. Postintubation Tracheal Stenosis: Management
and Results 1993 to 2017. Ann Thorac Surg
2019;108:1471-7. https://doi.org/10.1016/j.athoracsur.2019.05.050
11.
Piazza C, Lancini D, Filauro
M, et al. Post-COVID-19 airway stenosis treated by tracheal
resection and anastoÂmosis: a bicentric experience. Acta Otorhinolaryngol Ital 2022;42:99-105. https://doi.org/10.14639/0392-100X-N1952
12.
Palacios JM, Bellido DA, Valdivia FB, et al. Tracheal stenoÂsis as a complication of prolonged intubation in
coronavirus disease 2019 (COVID-19) patients: a Peruvian cohort. J Thorac Dis 2022;14:995-1008.
https://doi.org/10.21037/jtd-21-1721
13. Ramalingam
H, Sharma A, Pathak V, et al. Delayed Diagnosis of Postintubation Tracheal Stenosis due to the Coronavirus
Disease 2019 Pandemic: A Case ReÂport. A Pract 2020;14:e01269. https://doi.org/10.1213/XAA.0000000000001269
14.
Nauta A, Mitilian D, Hanna
A, et al. Long-term Results and Functional Outcomes After Surgical Repair of Benign LaÂryngotracheal
Stenosis. Ann
Thorac Surg 2021;111:1834- 41.
https://doi.org/10.1016/j.athoracsur.2020.07.046