Autor : Aranda Castro, Ricard1,2, Picos, Erica1, JoaquĂn, Javier MoisĂ©s1,3, Castro, Ignacio1,4, Staffolani, Pablo1,5, Fradin, BĂĄrbara1, Dutto, EstefanĂa1,4, Frankenberger, Gabriel1,6, De Sousa, Paula1, Fiorentini, Victoria1, CortĂ©s, JeremĂas1,7, Ălvarez, Sabrina1
1 Hospital Central, Mendoza, Argentina 2Hospital Dr. RamĂłn Carrillo, Mendoza, Argentina 3Hospital Sociedad Española, Mendoza, Argentina 4Hospital Privado, Mendoza, Argentina 5Hospital Español, Mendoza, Argentina 6ClĂnica de Cuyo, Mendoza, Argentina 7Hospital Diego Paroissien, Mendoza, Argentina
https://doi.org/10.56538/ramr.RCCH6240
Correspondencia :Ricard Aranda Castro E-mail: ricardaranda@proÂton.me
ABSTRACT
Introduction: During the SARS-CoV-2 pandemic, the high-flow nasal cannula (HFNC) was
used as support while waiting for the Intensive Care Unit (ICU) or as an
alternative to invasive ventilation.
Objectives: Primary: to determine if the high-flow nasal cannula prevents orotracheal intubation. Secondary: to analyze predictors of
success at the start of the high-flow nasal cannula treatment and descriptive
analysis of the sample.
Materials and methods: retrospective descriptive observational study. We included patients over
16 years of age positive for SARS-CoV-2, treated in the emergency departÂment
and Intensive Care Unit. The patients used the high-flow nasal cannula between
October 2020 and March 2021. Data was collected in individual forms, which were
then analyzed by an external professional.
Results: The study included 72 patients (16 to 88 years old), 20 women and 52
men. 50 % of the sample avoided orotracheal
intubation. Initial IROX, âsuccessâ group vs. âfailureâ group p = 0.006.
Comparison of IROX at 12hr, âsuccessâ group vs. âfailureâ
group p < 0.001. Comparison of âTime from admission to start
of high-flow nasal cannula treatmentâ, âsuccessâ group vs. âfailureâ group p
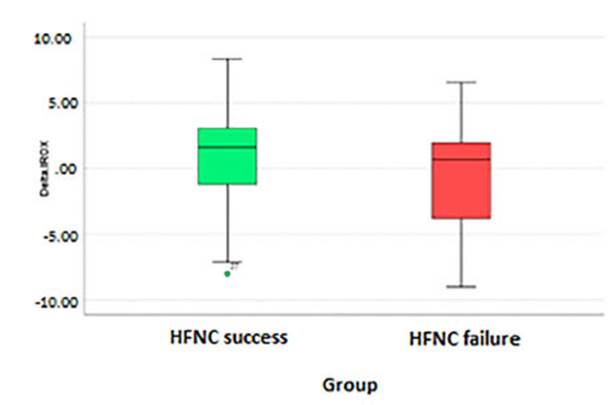
= 0.133 Comparison of âDelta IROXâ, âsuccessâ group vs. âfailureâ group p
= 0.092.
Conclusion: Orotracheal intubation was avoided in 50 % of the cases. The initial IROX and the
IROX 12 hours after the use of the high-flow nasal cannula were statistically
significant, which is a good predictor of success in this population. The date of
sympÂtom onset and the use of the HFNC and Delta IROX during the first 12 hours
were not statistically significant for the success of the treatment. These data
are a useful tool for generating patient selection protocols for this disease.
Key words: High-flow nasal cannula, High-flow oxygen therapy, Respiratory failure,
SARS-CoV-2 infection
RESUMEN
IntroducciĂłn:
Durante
la pandemia por SARS-CoV-2, la cĂĄnula nasal de alto flujo (CNAF) se usĂł como
soporte en espera de Unidad de terapia intensiva (UTI) o como alternativa a la
ventilaciĂłn invasiva.
Objetivos:
Primario:
Determinar si la cĂĄnula nasal de alto flujo evita la intubaciĂłn oroÂtraqueal. Secundarios: Analizar predictores de Ă©xito al
inicio de la cĂĄnula nasal de alto flujo y anĂĄlisis descriptivo de la muestra.
Materiales
y métodos: Estudio
observacional descriptivo retrospectivo. Se incluyeron pacientes mayores de 16
años positivos para SARS-CoV-2, atendidos en guardia y unidad de terapia intensiva,
que utilizaron cĂĄnula nasal de alto flujo entre octubre de 2020 y marzo 2021.
Se recolectaron datos en planillas individuales, analizadas por un profesional
externo.
Resultados:
Se
incluyeron en el trabajo 72 pacientes (de 16 a 88 años), 20 mujeres y 52
hombres. El 50 % de la muestra evitĂł la intubaciĂłn orotraqueal.
El IROX inicio grupo âĂ©xitoâ vs. grupo âfracasoâ, p
= 0,006. ComparaciĂłn Irox 12 h grupo âĂ©xitoâ vs. grupo âfracasoâ p < 0,001. ComparaciĂłn âtiempo
desde ingreso a inicio de cĂĄnula nasal de alto flujoâ grupo âĂ©xitoâ vs. grupo âfracasoâ, p = 0,133. ComparaciĂłn âDelta IROXâ
grupo âĂ©xitoâ vs grupo âfracasoâ p = 0,092.
ConclusiĂłn:
Se
evitĂł la intubaciĂłn orotraqueal en el 50 % de los
casos. El IROX de inicio y el IROX a las 12 h del uso de cĂĄnula nasal de alto
flujo fue estadĂsticamente significativo, lo que es un
buen predictor del Ă©xito en esta poblaciĂłn. La fecha de inicio de sĂntomas y el
uso de cĂĄnula nasal de alto flujo y el delta del IROX durante las priÂmeras 12
h no fue estadĂsticamente significativo para el Ă©xito
de la terapia. Estos datos son una herramienta Ăștil con el objeto de generar
protocolos de selecciĂłn de pacientes para esta patologĂa.
Palabras
claves: CĂĄnula
nasal de alto flujo, Oxigenoterapia de alto-flujo, Insuficiencia respiraÂtoria,
InfecciĂłn por SARS-CoV-2
Received : 15/11/2023
Accepted : 09/27/2023
INTRODUCTION
The use of the high-flow nasal
cannula (HFNC) increased during the COVID-19 pandemic due to the high demand
from patients with acute respiraÂtory failure (ARF).
The use of high-flow oxygen
therapy was a point of controversy among major critical care medical societies
worldwide during the COVID-19 panÂdemic, especially due to concerns regarding the
safety of the healthcare personnel and the delay in starting therapy.1
Therefore, the therapeutic
measures traditionÂally implemented to counteract COVID-19-related hypoxemia have
included conventional oxygen therapy and invasive mechanical ventilation.
The use of oxygen (O2)
through a conventional oxygen therapy mask has long been the first-line therapy
for patients with acute respiratory failure (ARF).
However, this strategy is far
from ideal because conventional oxygen therapy does not reduce respiratory
effort or improve alveolar ventilation.
On the other hand, the gas
delivered by convenÂtional devices is dry and cold, which can irritate the
airways, disrupt mucociliary clearance, and cause
discomfort to the patient.2
The use of the HFNC allows for
improved oxyÂgenation through various mechanisms, such as a reduction in the
dilution of the oxygen administered with ambient air,3, 4 a decrease in
dead space,4,
5 an
inÂcrease in circulating volume,5,
6 and
the generation of positive airway pressure (CPAP),6-8 resulting in a reduction of respiratory effort
and respiratory rate.6-10
The use of the HFNC allows for
the delivery of a gas flow of up to 60 L/min through silicone nasal cannulas,
with the supplied gas conditioned to ideal temperature and humidity levels
(37°C and 100 % relative humidity).
Several studies have demonstrated
that usÂing flow rates between 35 and 60 L/min results in mean expiratory
pressures at the pharyngeal level of 2-3 cmH2O with the mouth open
and 5-7 cmH2O with the mouth closed.11-12 Furthermore, it has been shown that the use of
the HFNC inÂcreases lung impedance at the end of expiration,5, 6 a parameter
correlated with lung volume. Alveolar recruitment is optimized,13 due to
increased airway pressures.
Considering the positive outcomes
observed with the early application of the HFNC in patients with moderate to
severe COVID-19 pneumonia,14,15 and using the IROX index16,17 as a predictor of sucÂcess, this retrospective
observational study aims to establish an objective relationship between
treatment success and failure with the analyzed variables, offering a robust
tool for managing the disease.
Faced with the high mortality
observed during the first wave of the pandemic, there arose a need for more
efficient approaches to treat hypoxemia in COVID-19 patients.18,19
The primary objective of this
study is to deterÂmine whether the HFNC avoids orotracheal
intuÂbation. As secondary objectives, the study aims to analyze whether the
initial IROX, the IROX at 12 hours, the Delta IROX during the first 12 hours,
and the start of HFNC treatment from the onset of symptoms serve as predictors
of treatment success.
MATERIALS AND METHODS
Designs
This is a retrospective and
descriptive study of patients attended at the Hospital Central, a regional
hospital in the region of Cuyo, Argentina, who were
admitted to the Emergency Department and Covid
Intensive Care Unit.
The ARF is the inability of the
respiratory system to fulfill its basic function, which is the gaseous exchange
of oxygen and carbon dioxide between ambient air and circulating blood; with
the presence of arterial hypoxemia (PaO2
below 60 mmHg), at rest, at sea level, and breathing ambient air,
with or without hypercapnia (PaCO2
above 45 mmHg). We will refer to hypoxemia only in cases where
the PaO2 is between 60
and 80 mmHg. With pulse oximetry, oxygen saturation
values of 90 % to 95 % can be considered equivalent to a PaO2
of 60 to 80 mmHg (hypoxemia), and if they are 90 %, they are
equivalent to a PaO2 of 60 mmHg
(respiratory failure).21
The HFNC is a non-invasive
respiratory support deÂsigned to deliver flows between 30-60 L/min. It works by
mixing air and oxygen, humidified and heated through a nasal cannula
specifically designed for these therapeutics.2
The IROX is a variable used to
evaluate the success or failure of a high-flow nasal cannula for respiratory
failure; it is the ROX index (IROX) that combines oxygenation (SpO2/ FiO2) and
respiratory work (RR). Its validity in COVID-19 pneumonia has a high
sensitivity for predicting therapy failure and is associated with high
mortality (45.4 %).16,
17
The diagnosis of Covid-19 was
made by nasopharynÂgeal swabbing by the on-call laboratory staff and referred
to the molecular biology service of the Hospital Central, where the sample was
analyzed by PCR (polymerase chain reaction through viral RNA) with the Schep SARS-CoV-2 Multi-FAST Kit.
Sample
In the period between
October 2020 and March 2021, with confirmed Covid 19
and suspicious symptoms. The sample included
patients older than 15 years, and collaborators who tolerate the device and
follow the operatorâs indicaÂtions within their psychophysical limitations. The
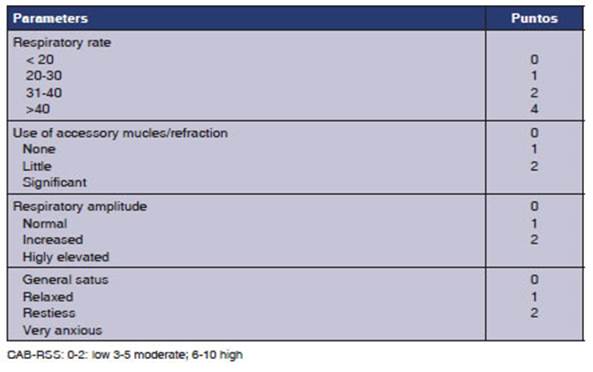
Cabrini Respiratory Strain Scale (CAB-RSS) (Annex 1) was used as a guide for orotracheal intubation criteria with a CAB-RSS score of 3
to 5; patients without orotracheal intubaÂtion
criteria, with poor clinical prognosis for intubation and confirmed diagnosis
of COVID-19 by rapid test or nasopharyngeal swab. Patients with criteria of
imminent need for OTI (orotracheal intubation) and
CAB-RSS scale of less than 2 or greater than 6 were excluded.
Variables
In patients who met the inclusion
criteria, the following variables were analyzed during the first 24 hours: age,
sex, comorbidities, initial IROX, and IROX at 1, 2, 4, 6, 12 hours after
starting treatment with HFNC, success or failure of treatment in relation to
the days elapsed between the date of symptom onset and the start of treatment
with the high-flow nasal cannula.
The data were collected in
individual patient spreadÂsheets and shared by means of a drive between on-call
kinesiologists in each area from Monday to Sunday,
and then analyzed using the Access program.
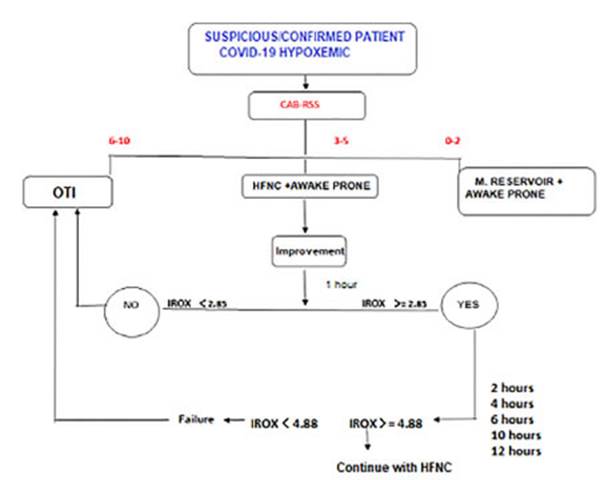
On admission, the patient was
clinically evaluated with the CAB-RSS scale; if he/she showed signs of
hypoxemia and a score of up to 2 on this scale, conventional oxygen therapy was
continued with eventual prone decubitus positioning. If the CAB-RSS score was
between 3 and 5, the HFNC was placed and the patient was put in prone decubitus
position. After the placement of the HFNC and eventual change of decubitus,
clinical signs were evaluated thoroughly during the first 12 hours with IROX. If
the IROX was equal to or lower than 2.85 in the first place, it suggested OTI;
if the IROX was equal to or higher than 3.85, treatment was continued and
evaluations were performed in the following hours. If IROX was lower than 4.88
at 6 hours after initiaÂtion, it was considered as treatment failure; and if it
was higher, treatment was continued (Figure 1).
Monitoring HFNC placement in patients
was performed through the ROX index (IROX), which is defined as the ratio
between pulse oximetry/ fraction of inspired oxygen
(SpO2 /FiO2) and
respiratory rate (RR). Roca et al20
identiÂfied patients at high risk of HFNC failure when this index
was < 4.88 at 12 hours. The cutoff values were different, as were the cutoff
times for predicting failure. A recent meta-analysis was able to evidence in
the subgroup using an IROX > 5 greater discriminatory accuracy in predicting
failures compared to a cutoff value ≤ 5. 17
HFNC treatment was started with
high flows of 50-60 L/min, adjusting the FiO2
to maintain the SpO2 between 92
%-96 %. The temperature was automatically regulated by the equipment. Patients
were put in prone decubitus position from the beginning, and were alternated
with lateral decubitus positions depending on their tolerance. Patients were
monitored by noninvasive measurement of heart rate and blood pressure, oxygen
saturation and respiratory rate. The FiO2
was gradually reduced while maintaining the target SpO2. The
flow was also decreased gradually depending on patient tolerance and
respiratory rate reduction.
The failure of the HFNC is
defined as the escalation to invasive mechanical ventilation (IMV) or death.
Standard indications for orotracheal intubation (OTI)
included the following: respiratory rate (RR) of more than 35 breaths/ min,
obvious activity of accessory respiratory muscles or paradoxical abdominal
breathing, progressively increase of PaCO2, hemodynamic instability, and inability
to protect the airways or inability to obtain saturation above 93 % with a FiO2 of more than
80 %.
For the implementation of the
HFNC, a patient interface was used, which consisted of a flexible nasal cannula
insÂtead of face masks, allowing the patient to be independent in functions
such as eating, drinking, talking and sleeping easily without interrupting
therapy, and is available in several sizes adapted according to the patientâs
anatomy (AquaNaseE); high flow and precise O2 system
allowing to deliver a flow between 0 to 60 L/min and FIO2
from 21 % to 100 % (Neumovent tecme TS, Leistung Luft 3, R203P14, R219P86), humidifierheater
system with or without tempeÂrature control (Fisher&paykel,
AquaVENT AMHH2600A), non-condensing tubing (Armstrong
Medical AquaVent).
Statistical analysis
For the statistical analysis we
had the IBM SPSS software platform, which was used by a professional external
to the study. The results are presented for categorical variables such as count
and their proportion within the category. Numerical variables, whether they are
continuous or discrete, are observed as appropriate to their distribution, such
as mean and standard deviation or median and interÂquartile range.
To compare the association
between categorical variaÂbles, we used the Studentâs t-test or Mann-Whitney U
test for numerical variables depending on their distribution. For
non-parametric variables, we used the Kolmogorov- Smirnov test. The chi-squared
test was used for comparing qualitative variables. A value of p < 0.05 in
two-tailed tests was considered to be statistically significant.
RESULTS
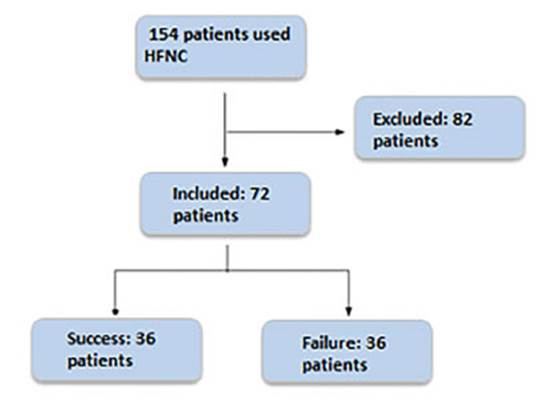
A total of 154 patients were
reviewed, and a sample of 72 patients who had been consecutively selected and had
completed the data collection form was included. 82 patients were excluded due
to missÂing data (Figure 2). 50 % of the patients avoided orotracheal
intubation. The populationâs characÂteristics are presented in Table 1.
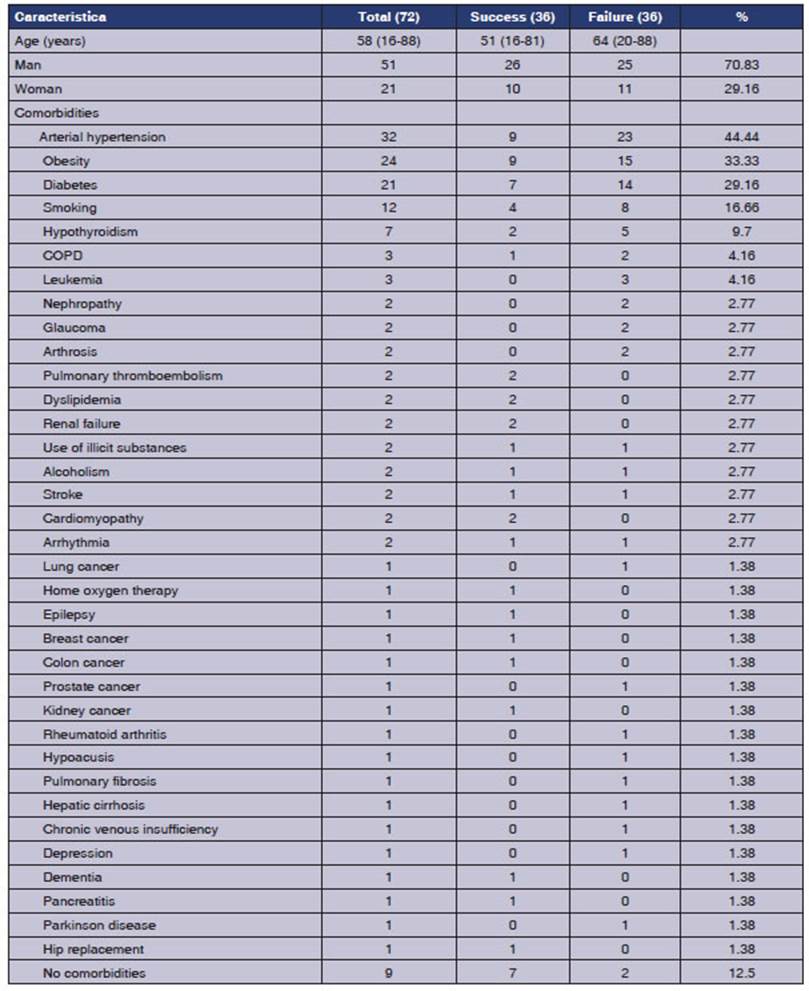
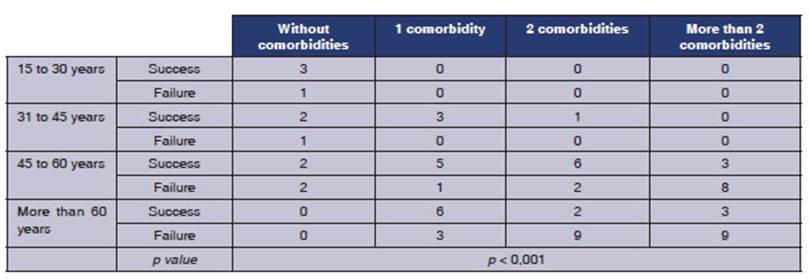
It was observed in the group of
patients that those who experienced failure were older adults with two or more
comorbidities, with a significant p-value of p < 0.001 (Table
2).
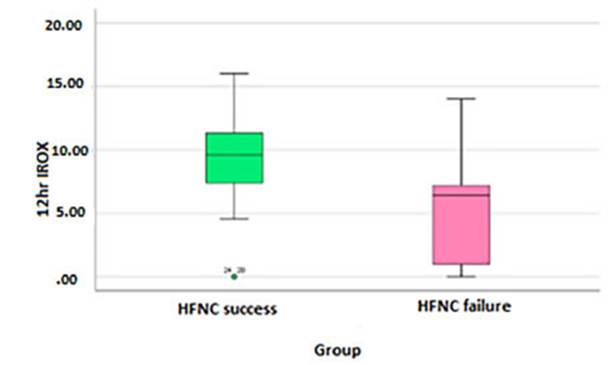
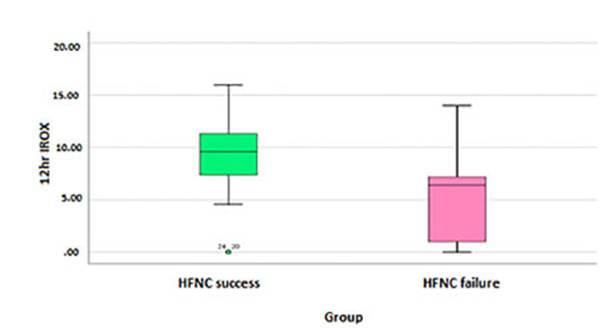
The initial IROX is significantly
different beÂtween both groups, with a mean of 7.10 (95 % CI 6.41-7.79), a
median of 6.78, and a standard deviaÂtion of 2.94. The comparison of the
initial IROX between the success group and the failure group yielded a mean ±
of 6.24 ± 2.32, with a p-value of 0.006 (Figure 3).
The IROX score at 12hr is
significantly different between both groups, with a mean of 7.26 (95 % CI
6.25-8.27), a median of 7.18, and a standard deviation of 4.29 with a p <
0.001 (Figure 4).
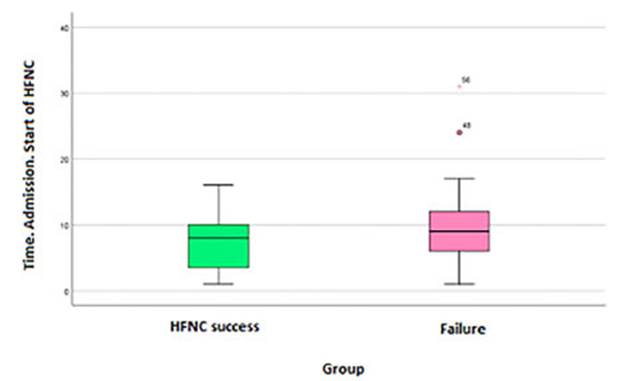
The time elapsed between symptom
onset (SO) and the start of the HFNC doesnât have a statisÂtically significant
relationship with a p-value of 0.133, mean of 8.76 (95 % CI 7.47-10.05),
a median of 8 and a standard deviation of 5.254. (Graph 3).
The Delta IROX (initial IROX/IROX
at 12hr) wasnât statistically significant with a p-value of 0.092, mean value
of 0.16 (95 % CI 0.76-1.07), a median of 1.19 and a standard deviation of 3.9
(Figure 5).
DISCUSSION
After several months of the
pandemic, a high mortality rate was observed in patients who were under
invasive ventilation; early intubation in COVID-19 is not correlated with a
favorable progÂnosis, as noted by Plotnikow et al18 and Farkas et al.19 The use of
the HFNC reduces the need for early intubation in adult patients with acute
respiratory failure. This helps to prevent the asÂsociated risks of invasive
mechanical ventilation, such as delirium, cognitive decline, ICU-acquired
weakness, and secondary infections.
High-flow oxygen therapy through
the HFNC is an innovative technique that combines O2
and compressed air, allowing the delivery of high conÂcentrations
of O2 at flow rates
exceeding the peak inspiratory flow in patients with high ventilatory
demands.
This oxygenation strategy is
particularly comÂfortable for the patient due to the nasal cannula that
provides humidified and warm gas, similar to physiological conditions. It also
allows functional independence for activities like oral feeding, comÂmunicating,
sitting up, and changing decubitus position without complications, as noted by MelÂlado-Artigas et al.21
The IROX has been suggested as a
tool to predict the outcome of the HFNC in patients with ARF. In the initial
phase (within the first hour of HFNC treatment), we have demonstrated that the
IROX is capable of distinguishing between the success and failure of HFNC
treatment in COVID-19 patients, but not with the threshold value sugÂgested by
Roca et al,9 since we have
shown better prediction accuracy with a higher threshold value.
The time elapsed between the SO
and the start of the HFNC treatment was not found to be sigÂnificant. This data
may reflect a direct relationÂship with a lower severity index at the beginning
of treatment. The average IROX in patients who started HFNC
treatment late (after 10 days). The success or failure of treatment
could be related to the initial level of hypoxemia and respiratory mechanics involvement,
regardless of the number of days since symptom onset.
Older adults, defined as those
aged 60 years or older with two or more comorbidities, accounted for half of
the total failures. This information is useful for hospital management, so that
HFNC can be used with critical care units or units nearby for older patients,
and in regular wards or peripheral hospitals in the case of the other group of
patients.
Limitations
In the first place, this is a
retrospective analysis, but it was based on prospectively collected data. Due
to the retrospective nature, the standardÂization of intubation was not decided
a priori. Furthermore, itâs a single-center study, which means we cannot
compare different population characteristics in the same region. Additionally,
these results cannot be extrapolated to other non- SARS-CoV-2-related
conditions that also cause acute respiratory failure due to a lack of evidence.
CONCLUSION
Our work demonstrates that the
HFNC is a valuÂable tool for avoiding orotracheal
intubation in patients with ARF caused by SARS-CoV-2 pneuÂmonia.
The initial IROX and the IROX at
12 hours are predictors of the therapyâs success.
It would be interesting to
investigate the value of this method in other etiologies of ARF.
Conflict of interest
Authors have no conflicts of
interest to declare.
Acknowledgement
Thanks to Dr. Pablo Ferrada for his collaboration in data analysis and Dr.
Carlos Widerhold for the review.
REFERENCES
1. Agarwal
A, Basmaji J, Muttalib F,
et al.High-flow nasal cannula for acute hypoxemic
respiratory failure in paÂtients with COVID-19: systematic reviews of
effectiveness and its risks of aerosolization,
dispersion, and infection transmission Can J Anaesth 2020;67:1217-48. https://doi. org/10.1007/s12630-020-01740-2
2.
Alfonso NC, Sayat MC. CĂĄnula Nasal Alto-Flujo (CNAF):
Puesta al dĂa. Arch Med. 2009;15:1-8.
3. Shelly MP. Inspired
gas conditioning. Respir Care. 1992;37:1070-80.
4. Wettstein RB, Shelledy DC, Peters
JI. Delivered oxygen concentrations
using low-flow and high-flow nasal canÂnulas. Respir
Care. 2005;50:604-9.
5. Dysart K, Miller TL, Wolfson MR, Shaffer TH. ReÂsearch in high flow therapy:
Mechanisms of action. Respir Med. 2009;103:1400-5. https://doi.org/10.1016/j.rmed.2009.04.007
6. Ricard
JD. High flow nasal oxygen in acute respiratory failure.
Minerva Anestesiol. 2012;78:836-41.
7. Riera
J, Pérez P, Cortés J, Roca O, Masclans JR, Rello J. Effect of high-flow nasal cannula and body
position on end-expiratory lung volume: A cohort study using electrical
impedance tomography. Respir Care. 2013;58:589-96. https://doi.org/10.4187/respcare.02086
8. Parke R, McGuinness
S, Eccleston M. Nasal high-flow therapy delivers low
level positive airway pressure. Br J Anaesth. 2009;103:886-90. https://doi.org/10.1093/bja/aep280
9.
Roca O, Riera J, Torres F, Masclans JR. High-flow oxyÂgen therapy in acute respiratory
failure. Respir
Care. 2010;55:408-13.
10. Parke RL, McGuinness SP, Eccleston ML. A preliminary randomized controlled trial to assess effectiveness of
nasal high-flow oxygen in intensive care patients. Respir
Care. 2011;56:265-70.
https://doi.org/10.4187/respcare.00801
11. Groves N, Tobin A. High flow
nasal oxygen generates positive airway pressure in adult volunteers. Aust Crit Care. 2007;20:126-31.
https://doi.org/10.1016/j.aucc.2007.08.001
12. Sztrymf
B, Messika J, Bertrand F, Hurel
D, Leon R, Dreyfuss D, et al. Beneficial effects of
humidified high flow nasal oxygen in critical care patients: A prospective
pilot study. Intensive Care Med. 2011;37:1780-6.
https://doi.org/10.1007/s00134-011-2354-6
13. Sztrymf
B, Messika J, Mayot T, Lenglet H, Dreyfuss D, Ricard JD. Impact of high-flow nasal cannula oxygen therapy
on intensive care unit patients with acute reÂspiratory failure: A prospective
observational study. J Crit Care.
2012;27:324.e9-13.
https://doi.org/10.1016/j.jcrc.2011.07.075
14. Vega ML, Montiel
G, Colaianni N, et al. Resultados
preliminares de una unidad de soporte ventilatorio no invasivo en
SARS-COV-2 Preliminary results of a non-invasive ventilaÂtory
support unit in SARS-COVID-2. Medicina (B Aires). 2020;80 Suppl 6:1-8.
15. Patel M, Gangemi
A, Marron R, et al. Retrospective analysis of high
flow nasal therapy in COVID-19- related moderate-to-severe hypoxaemic
respiratory failure. BMJ Open Respir Res. 2020;7:e000650. https://doi.org/10.1136/ bmjresp-2020-000650
16. Chandel
A, Patolia S, Brown AW, et al. High-flow nasal
cannula in COVID-19:Outcomes of application and examiÂnation
of the ROX index to predict success. Respir Care.
2020;66:909â19. https://doi.org/10.4187/respcare.08631
17. Prakash
J, Bhattacharya PK, Yadav AK, Kumar A, Tudu LC, Prasad K. ROX index as a good predictor of high
flow nasal cannula failure in COVID-19 patients with acute hypoxemic
respiratory failure: A systematic review and meta-analysis. J
Crit Care. 2021;66:102-8.
https://doi.org/10.1016/j.jcrc.2021.08.012
18. Plotnikow
GA, Matesa A, Nadur JM, et
al. Characteristics and outcomes of patients infected with CoV19 requiring
invasive mechanical ventilation in Argentina. CaracterĂstiÂcas y resultados de los
pacientes infectados con nCoV 19 con requerimiento de
ventilaciĂłn mecĂĄnica invasiva en la Argentina. Rev Bras Ter Intensiva. 2020;32:348-53.
https://doi.org/10.5935/0103-507X.20200062
19.
Farkas J, Spiegel R, et al.
Rethinking the early intubaÂtion paradigm of COVID-19:
time to change gears? Clin Exp Emerg Med. 2020;7:78-80.
https://doi.org/10.15441/ceem.20.043
20.
Roca O, Masclans JR, PĂ©rez-TerĂĄn P. Papel de la oxigÂenoterapia
de alto flujo en la insuficiencia respiratoria aguda. Medicina Intensiva. 2015;39:505-15. https://doi.org/10.1016/j.medin.2015.05.009
21.
Mellado-Artigas R, Ferreyro BL, Angriman
F, et al. OxĂgeno nasal de alto flujo en pacientes con insuficiencia respiraÂtoria
aguda asociada a COVID-19. Crit Care. 2021;25:58. https://doi.org/10.1186/s13054-021-03469-w
ANNEX