Autor : Isidoro, Ricardo1, Debais, Marcelo2, Vilas, Gerardo3
1 Pulmonology specialist. Chief of the Bronchoscopy Service of the Hospital E. TornĂş. Buenos Aires 2 Pulmonology specialist. Bronchoscopy specialist of the Hospital TornĂş. 3Pulmonology specialist. Bronchoscopy specialist of the Hospital TornĂş
https://doi.org/10.56538/ramr.OKGR9772
Correspondencia : Ricardo Isidoro. E-mail: ricardoisidorodieÂguez@gmail.com
ABSTRACT
Three tracheal stents were removed
after 10, 16, and 22 years, followed by healing of tracheal stenosis.
Two new cases of benign tracheal
stenosis are reported, treated with silicone prosÂtheses, which presented for
follow-up after very long absences: 16 years in one case and 22 years in the
other. They add to a previously published case that was healed 10 years after
the stent was implanted, which also had a wide and stable tracheal lumen after
removal. The endoscopic findings are described, and reflections are included on
the healing of the observed stenosis in all cases and its probable relationship
with the prolonged indwelling of the prostheses. The physical properties of the
stents are invesÂtigated after such a long period since implantation, and they
are compared with a new device. A proposal is put forward that could lead to
the healing of tracheal stenosis with endoscopic treatment and prolonged
indwelling of the stent.
Key words: Tracheal stenosis, Tracheal stent, Tracheal prosthesis, Indwelling time of tracheal stent, Healing of benign
tracheal stenosis
RESUMEN
Tres
stents traqueales fueron removidos
luego de 10, 16 y 22 años, a lo que le siguió la correspondiente curación de la
estenosis traqueal.
Se
reportan dos nuevos casos de estenosis traqueal benigna, tratados con prĂłtesis
de silicona, que se presentaron a control luego de muy largas ausencias: 16
años en uno y 22 en otro. Se suman a un caso anteriormente publicado y curado
luego de 10 años de permanencia del stent, que
también presentó una amplia y estable luz traqueal luego la remoción. Se
describen los hallazgos endoscĂłpicos, y se incluyen reflexiones sobre la
curaciĂłn de la estenosis observada en todos ellos y su probable relaciĂłn con el
largo tiempo de permanencia de las prĂłtesis. Se investigan las propiedades
fĂsicas de los stents, luego de tan prolongado lapso
de implante y se las compara con un dispositivo nuevo. Se emite una propuesta
que podrĂa conducir a la curaciĂłn de las estenosis traqueales con tratamiento
endoscĂłpico y stent por tiempo prolongado.
Palabras
clave: Estenosis
traqueal, Stent traqueal, PrĂłtesis traqueal, Tiempo
de permanencia de un stent traqueal, CuraciĂłn de la
estenosis traqueal benigna
Received: 04/02/2023
Accepted: 08/02/2023
INTRODUCTION
This publication can be considered
a continuation of a previous one,1 published in 2016 by the same author and
titled “Tracheal Prosthesis. Prolonged Implant: 10 Years”.
Such publication provides a
“definition of traÂcheal stenosis” and another one of the “healing of
stenosis”. Finally, there is a table that organizes clinical criteria,
symptoms, and their relationship with the anatomical dimension of the tracheal
luÂmen after endoscopic treatment, along with the timing of appearance or
absence of recurrence.2
All of this allows the physician
to have a guide for understanding and determining healing of stenosis or
treatment failure.
The circumstances in which
healing can be esÂtablished are also explained, even if the tracheal lumen has
not regained its original diameter.
Healing criteria1
Tracheal stenosis, defined as a
“symptomatic reÂduction of the airway” requires a healing criterion that
involves at least the reversal of the aspects indicated by its definition. Therefore,
healing deÂmands the disappearance of the symptoms caused by this obstruction,
as well as the recovery of the airway lumen.
Once again, these two seemingly
fixed concepts –symptoms and airway lumen– are highly variable and will be
considered separately. Symptoms that are absent at rest might appear during
physical activity. Additionally, a complete recovery of the tracheal lumen,
determined by its diameter or useful section, is not necessary for the symptom
of stridor to disappear, even during exercise (Table 1).
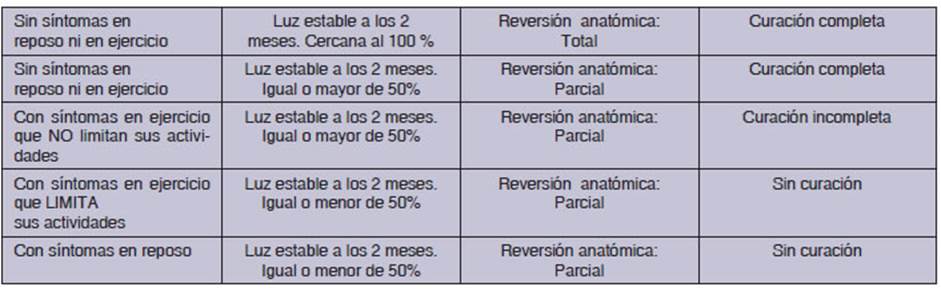
With a tracheal lumen diameter of
8 mm or more, there will be no stridor at rest when the stenosis is simple and
its length does not exceed 20 mm.
After analyzing all the elements
that define the framework of symptomatic airway stenosis, patients who remain
asymptomatic two months after completing their treatment, maintaining a fixed
tracheal lumen that is sufficient for the performance of their activities, are
considered healed. This is possible when, in anatomical terms, the tracheal
lumen is equal to or greater than 50% of the healthy trachea lumen in the same
patient.
We will refer to this as
“complete” healing, even though it is anatomically partial.
The following considerations will
complete the previous ones: the healing criterion must encomÂpass and include
asymptomatic cases, with a fixed or stable tracheal lumen that isn’t sufficient
for the performance of all the patient’s activities, thereby allowing them to
carry out their daily tasks with limitations.
We will refer to this
anatomically partial healing as “incomplete”.
Given the fact that the case
described in the previous publication was successfully healed without
complications, when the silicone stent was removed after 10 years, temptation
arose to support a line of reasoning suggesting that a longer indwelling time
of the stent could be associated with a higher likelihood of stabilizing the
tracheal wall and healing. It is observed that in other cliniÂcal situations,
this process occurs naturally.1 AdÂditionally, in other medical specialties, treatments
involving long-term stents or supports increase the
probability of success, and these are implanted with the intention of never
being removed.
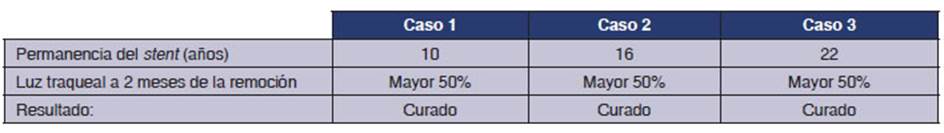
To the case described
with 10-year stent indwellÂing, two more cases are added, where the stents also
remained implanted without medical control for 16 and 22 years.
Thus, their
description can be outlined as folÂlows:
Case 0:
characteristics of a new and unused stent
Case 1: stent that
remains in the trachea for 10 years
Case 2: tracheal
stent with an indwelling time of 16 years
Case 3: tracheal
stent with an indwelling time of 22 years
Type of study
In
vitro/in vivo observational study.
MATERIALS AND METHODS
One new
silicone stent. Another
identical stent, implanted and removed after 10 years of
biological use. One stent implanted during 16 years and the other one during
22. All the stents were made using the same process and raw material: silicone
for use in human patients.
The study was based
on
– the
comparison of the hardness and elasticity of the stents extracted from the
patients with respect to the correspondÂing values of a new stent.
– the
analysis of the results of the treatment of benign tracheal stenosis in the
three patients.
Clinical case zero
Represented
by the control stent. New, unused. ManufacÂtured with silicone
for medicinal purposes.
Characteristics of
the new stent
Aspect: Translucid (Image A)
*Shore A Hardness Scale**: 78
*Expansion of rupture
(Mpa***): 5.3
Presence of
secretions or inlays: Not applicable
Proximal or distal
granulomas: Not applicable
*Determined at the
National Industrial Technology Institute (INTI, for its acronym in Spanish).
Argentina.
** Measurement of
elastic modulus. Preferred for rubÂber. It measures
the rebound height or penetration of a pyramidal cone.
***It is the maximum
stress before fracturing by cross-sectional area. Measurement in Newton/square
meter Ă— 10 raised to 6a (mega Pascal).
Case 1
60-year-old female
patient presented with stridor caused by central tracheal stenosis located 3
centimeters next to the vocal cords. The treatment involved endoscopic
resection of the stenosis, followed by the implantation of a silicone stent.
The stent model used was designed for tracheal steÂnosis, with a diameter of 14
mm at the ends, 12 mm in the central area, and a length of 40 millimeters.
There were no
immediate complications.
We lost contact with
the patient, and ten years later, she spontaneously returned to the endoscopic
center without experiencing any symptoms.
A flexible
respiratory endoscopy was performed, revealÂing that the stent was in the
correct position and fully permeable. No inlays or secretions were observed.
(Figure 2)


The stent was removed
and sent to the National InÂdustrial Technology Institute for physical
examination. (Figure 3)

Characteristics of the stent
removed 10 years after implantation
Aspect: Ochre-translucid
Shore scale hardness: It was
reduced from 78 to 71 Shore A units
Expansion of rupture: It was
reduced 0.3 Mpa
(average
of three measurements)
Presence of secretions or inlays
NO
Proximal or distal granulomas NO
After the removal of the
prosthesis, the trachea mainÂtained a wide diameter similar to that of the
removed stent, without deformations or localized malacia.
Endoscopic conÂtrol was carried out every 10 days, showing a slight, slow, and
progressive reduction in the diameter of the lumen in the stenosis area. This
retractile phenomenon stops, and the lumen stabilizes at the sixth week after
the prosthesis was removed, with a diameter exceeding 50% of what corÂresponds
to a healthy trachea. (Figure 4).

With a lumen diameter of more than
50% of the original, after two months, it was considered healed.1
Case 2
66-year-old male
patient who was treated 16 years ago for stridor caused by postintubation
benign tracheal stenosis. The patient
underwent endoscopic treatment involving resection and dilatation, along with
the implantation of a silicone stent identical to the model of the previous
case: a diameter of 14 mm at the ends and 12 mm in the central area, with a
length of 40 millimeters.
Sixteen years later, the patient
requested a follow-up appointment, reporting shortness of breath on exertion.
An endoscopy revealed partial
obstruction of the lumen distal to the stent with tissue that had the
macroscopic features of granulomas. (Figure 5)

A rigid bronchoscopy was
performed, and the prosthesis was removed. (Figure 6)

The extracted device was sent to
the National Industrial Technology Institute for physical examination.
After 8 weeks, the tracheal lumen
was wide and exceeded 50% (Figure 7). The patient was asymptomatic.

With a wide lumen, whose diameter
was similar to that of the normal trachea, stable after two months, the patient
is considered healed1.
Characteristics of the stent removed
16 years after implantation
Aspect: Opaque. Ochre color.
Shore scale hardness: 70 (8 units
lower than a new stent)
Expansion of rupture: 4.5 Mpa (0.8 Mpa lower than a new
stent)
Presence of secretions or inlays
NO
Distal granulomas YES
Note: these deviations from the
physical parameters with reference to those of a new stent are not considered
sigÂnificant.
Case 3
45-year-old male patient who
suffered from postintubation benign tracheal stenosis
located very close to the vocal cords. After being admitted due to an episode
of obstructive ventilatory difficulty, endoscopic
recovery of the tracheal lumen was performed, along with the implantation of a
classic straight silicone stent, with an external diameter of 16.25 mm and a
length of 40 mm. Then, the ventilatory function was
immediately stabilized.
All of this happened 22 years
ago.
The patient did not attend the
follow-up appointments until he felt compelled to do so due to the appearance
of late symptoms consistent with noisy breathing and isolated episodes of blood
expectoration, so he attended the hospital service, 22 years later.
The endoscopic examination
revealed the presence of a dark-looking stent at 2 cm from the vocal cords,
with secreÂtions inside that were insufficient to obstruct the airflow,
particularly in a stent of such a large caliber. However, the tracheal lumen
was greatly constricted at the end of the prosthesis, with the appearance of a
linear groove, due to the presence of two large contact granulomas positioned
laterally at 9 and 3 o’clock. (Figure 8)

A rigid bronchoscopy was
performed and the endoprosÂthesis was removed.
(Figure 9)

Two weeks later, the patient was
breathing normally and the aspect of the trachea was very satisfactory.
Following the same criteria1,
after two months with a lumen 50% larger than the original, the patient is considÂered
healed. (Figure
10)

Characteristics of the stent
removed 22 years after implantation
Aspect: Opaque. Dark brown
Shore A
Hardness Scale: N/A*
Expansion of rupture: N/A*
Presence of secretions or inlays
NO
Distal granulomas YES
*Device lost in the laboratory
DISCUSSION
The following considerations on the
matter that is being studied, while not definitive or conclusive, will organize
the knowledge on the subject.
In all cases, the stents were
removed. The reaÂsons can be found in the lack of understanding with regard to
the necessary period or at least the preferred duration for the implant to
produce a cure, as well as in the limited availability of studies that clarify
doubts on this matter. Periods of 10, 16, and 22 years turned out to be
empirically very long. The decision to remove the stents, initially intuitive,
was later based on the acceptable reason for extracting a product after such a
prolonged presence.
Regarding the mechanical
viability of the device, no further explanations will be added because, as we
already mentioned before, these are scarce or nonexistent, and the present
study aspires to additionally provide detailed knowledge on this point, which
can be found in Annex I at the end of the text.
Absence of complications after
implantation or silent course complications can be suspected in all cases,
since it was only in this way that patients were able to avoid clinical
monitoring.
On the other hand, the experience
strongly suggests that if these complications do not apÂpear within the first 6
months, they will not ocÂcur.1 However, in
contrast, Verma and colleagues believed and published
that stents weren’t well tolerated over long periods.5
In order to leave behind the
unappealing quesÂtion about how long a silicone stent “is able” to fulÂfill its
supporting function in the airway, it seems reasonable to say that very
extended periods far exceeding the usage time estimated by manufacÂturers do
not appear to be a problem, since it has been observed that the hardness and
elasticity of silicone change very little after 10 years in vitro and in the
patient.1
Other justifications can be found
in exceptional experiences like those presented here, which didn’t show any
defects in the supporting function of the prosthesis after so many years.
Physical and dynamic studies of the materials that make up the stents are
scarce or nonexistent.1 Other reasons, though empirical in nature,
can provide reassurÂance, such as the absence of problems in treated, referred,
or published cases as a consequence of defects in the implanted stent over long
periods.
Finally, from a technical
standpoint, the study presented in Annex I show that the stent mainÂtains its
primary function during prolonged periÂods of implantation.
Now, if we replace “is able” with
how long a stent “should” remain implanted in order to heal stenosis, an
uncomfortable question arises. The same question that
students always ask, and for which they receive unconvincing answers, even
after more than three decades of experience with the use of prostheses in the
airway.
The review of publications
reveals that initially the prostheses remained implanted for short peÂriods,
from 6 to 18 months2-4, as recommended by F. DumĂłn
in the beginning, although later he considered that probably there were fewer
recurÂrences in patients who had stents for a longer time.6
Publications or recommendations about the indwelling time of a stent are very
difficult to find.
Long indwelling periods occur
occasionally and have been reported.5-6
We had a tendency to keep the
stents for longer periods,7 with the
conviction that the passing of time can contribute to a firm healing of the
tracheÂal wall, as it happens in diseases of other organs.
Gathering statistically robust
information on the results of endoscopic treatment of benign stenosis can also
be difficult because of its limited availability.7
So, in our series of 198 cases,
the stents reÂmained implanted between 13 and 36 months, with an average of
28.6. The healing that was achieved combining the methods of thermal or mechanical
endoscopic resection, with or without dilatation, was 42%. It’s the same as
admitting that for 42% of those patients, the treatment has been very good, and
for the rest, it was very bad.
Now, these results
show that almost one every two patients will relapse and return to the starting
point of their tracheal disease to restart the long path of decisions and
therapies, with a discourageÂment that is difficult to hide.
CONCLUSION AND RESULTS
All three cases of occasional
indwelling of a traÂcheal stent for 10, 16, and 22 years were healed after
stent removal.
This cannot lead to
any conclusions; however, there is a feeling of astonishment that all three
patients healed immediately, along with the inÂevitable regret that there
wasn’t a larger number of cases.
This striking
circumstance invites us to wonder and discover if, through a statistical
analysis, the healing of tracheal stenosis around the prosthesis is necessarily
related to the prolonged indwelling time of the stent, and if much longer
periods than those used so far are required.
Conversely, medium
and short periods of imÂplantation could be the cause of poor results.
It must be made very
clear that only patients who do not show immediate complications or
complications during the first year of stent implanÂtation, such as the
formation of bacterial plaque inlays,7 excessive secretions, the
development of granulomas, or other, would be candidates to participate in a
study with extended periods of stent implantation. Experience has shown that if
patients don’t show these complications in the first year, they don’t tend to
ever show them.1
Finally, since the
short periods were insufficient and those of 28 months on average only healed
42% of the cases, it is inevitable to propose a longer indwelling time of the
stents for benign stenosis.
And these
considerations lead to the unavoidÂable question: how long should the
indwelling period be?
Before hastily
proposing the controversial peÂriod of 10 years, in order to obtain better
adaptaÂtion to change, we can reflect on the matter.
We can begin by
admitting, in the first place, that the stent indwelling times already
established or used so far are insufficient. Secondly, we still don’t know
which should be the sufficient times, and the little information we have about
this (three cases with 10, 16, and 22 years) is invalid or barely worthy of
consideration from the statistical or almost any other point of view.
Still, given the need
to improve the results of a treatment that has been administered for almost
three decades, we could propose an initial period of 10 years, as it
corresponds to the case we have presented with the shortest indwelling time and
the best result.
Thus, a study that
allows us to know the perÂcentage of healing after ten years would enable the
examination of a new series in the following study, with a shorter indwelling
period, thus repeating the trial until the appearance of an increase in the
recurrence rate allows the determination of the best period in years for stent
indwelling time; that is to say, the shortest period that produces the highest
healing rate, which, based on the inÂformation presented on the topic, falls
between 28 months and 10 years.
ANNEX I
DETERMINING THE LIFE OF TRACHEOBRONCHIAL STENT FAMILY IMPLANTS
Jorge Gallo, Engineer
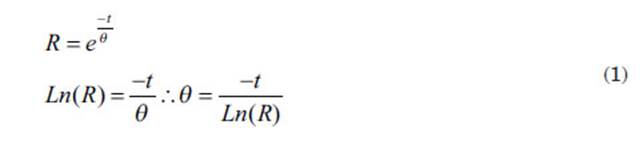
1. Theoretical introduction
In order to determine
the shelf life of this family of implants, we use the mathematical model of ExponenÂtial
Distribution, which is the one that best fits for analyzing the durability of
implants. This is derived from the general expression of the Weibull distribution, whose mathematical expression is as
follows:

Where:
R(t): the probability at a given moment for a medical
device to still have the potential to fulfill its intended use; abbreviated as
reliability. Reliability is a variable that decreases over time (t) due to the
negative factor in the exponential expression (1).
q: a statistical value referred to as characteristic
life, the meaning of which will be analyzed further in this report.
e: the base of natural logarithms.
b: another statistical value of the distribution, which
is different for the Weibull distribution comÂpared
to the Exponential Distribution, where it equals one.
So, the expression
(1) for b = 1 becomes:
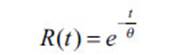
which is the one we have used in our work and allows for
the following graphical representation
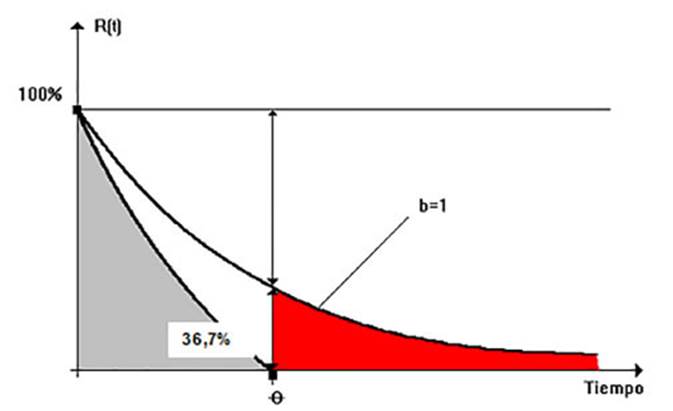
If we analyze this chart
we can see that mathematically speaking, the characteristic life “q” is the
time it takes for the “no defects” probability (reliability) to decrease to
approximately 37%, which is its mathematical definition.
In our work, we
adopted the distribution that defines the shaded area in the previous chart,
thus ignoring the asymptotic nature of the original mathematical model.
However, this conservative simÂplification allows us to establish the second,
more practical definition of “q” which is the one we use in this study
considering it as the end of the device’s shelf life. This is also known
as the predictable durability of the stent.
For these
distributions, we work with data obtained from implants that fail after being
placed. Since there are no defective implants in our sample, we must use an
attributive method to graphically deterÂmine the value of “R” and then
that of “q”, for a confidence level of C = 95%.
Description of the
applied methodology
2. Input and output data
In our case, we have
a sample of implants that have worked properly up to the date of this analysis
(January 31, 2019). These data are presented in the table of Annex II.
Based on the data
summarized in this table, we obtain the following input data for our analysis:
• Sample size N =
18
• Average aging time
of the sample (implantation) was t = 618 days (we do not use the average
because the distribution of this variable is not Gaussian).
• Number of items
whose performance goes according to specifications (number of OKs in the
sample) 18
With this data, we
need to determine the characteristic life “q” as the output data of the
calculation process.
2.2. Calculation process used
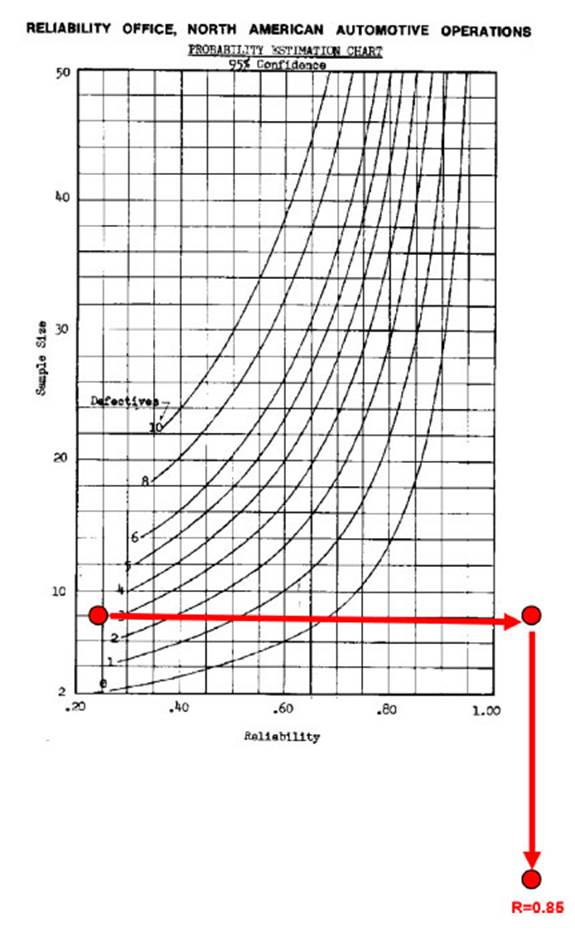
We need to determine the
q value. To do this, we use the attribute-graph that was created basing on a
confidence level of C = 95% using the curve for zero defects in the
sample, entering horizontally with the value of “n” and extracting the
corresponding value of “R(t)” from the chart.
Once we knew this
value of R(t), we used the mathematical
expression of the exponential distribuÂtion to obtain the value of the
characteristic life q as follows:
3. Case resolution
3.1. Input data
With the data
available in the Annex of this report, we have the following input data for the
calculation:
• Sample size: 18
• Median time of
aging with no defects (the average was not used because the time column is
not a Gaussian distribution): 618 days
• Number of items
meeting the intended use: all of them (there wasn’t any “Not OK” in the
sample)
3.2. Output data
Using the input data
and the chart of Annex II, we obtained:
R = 0.85 (see
graphical solution on the next page).
Then, by applying the
expressions (1), we obtained the following output data from our work:
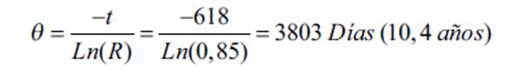
The predictable or inferred
durability of a stent manufactured by the company is 10.4 years.
Conflict of interest
The costs of
physical/dynamic examinations of the stents were covered by Stening
SRL. The stents used in the patients, extracted and analyzed were manufactured
by Stening SRL, Argentina. The author Ricardo Isidoro is partner and general manager of Stening SRL.
REFERENCES
1. Isidoro R. Prótesis traqueal implante prolongado: 10 años. Rev Am Med Resp. 2016;16:250-7.
2. Bolliger CT, Mathuer PN, Beamis JF, et al. ERS/ATS statement on interventional
pulmonology. Eur Respir J
2002;19:356-73.
https://doi.org/10.1183/09031936.02.002 04602
3. DumĂłn JF, Cavaliere S,
Diaz-Jiménez JP, et al. Seven-year experience with the Dumón
prosthesis. J Bronchol. 1996;3:6-10. https://doi.org/10.1097/00128594-199601000-00003
4. Ernst A, Silvestri GA, Johnstone D;
American College of Chest Physicians. Interventional pulmonary procedures:
Guidelines from the American College of Chest PhysiÂcians. Chest.
2003;123:1693-717.
https://doi.org/10.1378/chest.123.5.1693
5. Verma A, Um SW, Koh WJ, et al.
Long-term tolerance of airway silicone stent in patients with post-tuberculosis
tracheobronchial stenosis. ASAIO J. 2012;58:530-4.
https://doi.org/10.1097/MAT.0b013e318263c76f
6. Saito Y. Long-term
Wear and Tear of a Silicone Stent. J Bronchol. 2008;15:290-1. https://doi.org/10.1097/LBR.0b013e318187a2a6
7. Debais M, Boccia
CM, Isidoro R, et al. RepermeabilizaciĂłn de la vĂa
aérea con prótesis traqueobronquiales: 300 casos. Rev Am Med Resp. 2012;2:38-43.