Autor : Sánchez Soto, Carlos Alberto1 , Orea Tejeda, Arturo2 , González-Islas, Dulce2 , MartÃnez Vázquez, Valeria2, Sánchez Santillán, RocÃo2 , MartÃnez-Reyna, Oscar Ubaldo2
1 Thoracic Surgery Resident, Instituto Nacional de Enfermedades Respiratorias Ismael CosÃo Villegas, City of Mexico, Mexico. 2 Heart Failure and Respiratory Distress Clinic, Cardiology Department, Instituto Nacional de Enfermedades Respiratorias Ismael CosÃo Villegas, City of Mexico, Mexico
https://doi.org/10.56538/ramr.BPGS1496
Correspondencia : RocÃo Nayeli Sánchez SanÂtillán E-mail: rnsanchezs@gmail.com
ABSTRACT
Hemoptysis is defined as the
expectoration of blood from the tracheobronchial tree, typically originating
from bronchial arteries. Once the presence and bleeding site are confirmed, one
must choose among different methods for managing hemoptysis, each with its own
benefits and limitations. Bronchial artery embolization is a minimally invaÂsive
endovascular technique. It has become the method of choice for treating massive
and recurrent hemoptysis. Its success rate in the first episode is over 80%.
The recurÂrence rate after the procedure ranges from 10% to 55%, in which
surgery may play an important role.
Objectives: To describe the demographic and clinical characteristics, the
etiological diagnosis and treatment of patients with hemoptysis at a tertiary
care level hospital in the City of Mexico.
Materials and methods: Retrospective study of patients diagnosed with hemoptysis during the
period from January 2014 to December 2016. The data were obtained from the
clinical records.
Results: A total of 34 patients with a mean age of 52 years were studied, with a
preÂdominance of males (52.9%). The etiology of hemoptysis was tuberculosis
(45.5%), neoplasms (20.6%), bronchiectases (15.2%),
and arteriovenous malformation (6.1%). The most
frequent embolization site was the right upper bronchial artery (56.6%),
followed by the left lower bronchial artery (23.3%); and a group of 6 patients
(18.7%) required a second embolization procedure due to recurrence of bleeding.
Conclusion: The management of hemoptysis should be comprehensive. The main objective
is to maintain airway permeability and evaluate each patient for optimal manÂagement
based on the type and etiology of the hemoptysis.
Key words: Hemoptysis, Embolization, Treatment, Surgery
RESUMEN
La
hemoptisis se define como la expectoración de sangre del árbol traqueobronquial, por lo general se origina en las arterias
bronquiales. Una vez confirmada la presencia y el sitio de sangrado se debe elegir
entre los diferentes métodos de manejo de la hemoptisis, cada uno con sus
beneficios y limitaciones. La embolización de
arterias bronquiales es una técnica endovascular
mÃnimamente invasiva. Se ha convertido en el método de elección para tratar
hemoptisis masiva y recurrente. Tiene una tasa de éxito en el primer episodio
superior al 80%. La tasa de recurrencia posterior al procedimiento va de un 10
% a un 55%, en el cual la cirugÃa llega a tener un papel de importancia.
Objetivos:
Describir
las caracterÃsticas demográficas, clÃnicas, diagnóstico etiológico y
tratamiento de pacientes con hemoptisis en un hospital de tercer nivel de la
Ciudad de México.
Material
y métodos: Estudio
retrospectivo de pacientes con diagnóstico de hemoptisis en el periodo comprendido
entre enero de 2014 a diciembre de 2016. Los datos fueron obtenidos del
expediente clÃnico.
Resultados:
Se
estudiaron 34 pacientes media de edad 52 años, con predominio en hombres
(52,9%). La etiologÃa de la hemoptisis fue tuberculosis (45,5%), neoplasias
(20,6%), bronquiectasias (15,2%), malformación arteriovenosa
(6,1%). El sitio de emboÂlización más frecuente fue
la arteria bronquial superior derecha (56,6%), seguido de la arteria bronquial
inferior izquierda (23,3%) y un grupo de 6 pacientes (18,7%) requirieron un
segundo evento de embolización por recurrencia del
sangrado.
Conclusión:
El
manejo de la hemoptisis debe de ser integral. El objetivo principal es mantener
una vÃa aérea permeable y evaluar cada paciente para un manejo óptimo de acuerdo
al tipo y etiologÃa de la hemoptisis.
Palabras
clave: Hemoptisis,
Embolización, Tratamiento, CirugÃa
Received: 10/13/2022
Aceptado: 08/09/2022
INTRODUCTION
Hemoptysis is defined as the expectoration
of blood from the tracheobronchial tree, typically originatÂing from bronchial
arteries.1-7
Its severity can vary and may
require urgent in-hospital management. The prevalence varies depending on the
region under study. When apÂproaching a patient with hemoptysis, the first step
is to confirm the presence of airway bleeding and then identify the precise
site in order to establish the etiology and determine the most appropriate
treatment.1
Approximately 95% of hemoptysis
cases are self-limiting, while the rest can be potentially fatal. AlÂthough
there is no international consensus for its classification, it is generally
accepted that massive hemoptysis is that which can lead to respiratory failure
and patient’s death. Regarding the volume of blood, it varies widely from 100
mL to 600 mL with no defined time frame.3, 5, 8, 9
During the initial assessment, a
chest X-ray is the first study to be performed.7 However,
the absence of visible abnormalities does not rule out the presence of a lesion,
neoplasm, or other pathology causing hemoptysis, as its sensitivity is only
50%.1, 5, 6
Therefore, it is recommended that
the evaluÂation should be complemented with a computed tomography (CT) scan,
and if possible, a multi-deÂtector computed tomography angiography (MDCT
angiography). The MDCT angiography provides comprehensive anatomical coverage
that reduces respiratory motion artifacts. It has almost 100% accuracy in
identifying bleeding from bronchial arteries and also shows vascular anatomy, which
is useful for therapeutic planning,1, 5, 9 whose primary objective is to control the
bleeding.10
There is controversy about the
use of the bronÂchoscopy in patients with bleeding. The rigid bronÂchoscopy
offers good visibility and the possibility to aspirate clots and secretions,
with the benefit of being able to ventilate the patient simultaneously.
However, various publications report only a 50% success rate in locating the
bleeding site.3,
11
Bronchial artery embolization
(BAE) is a miniÂmally invasive endovascular technique that has become the
method of choice for treating massive and recurrent hemoptysis. It has a
success rate of more than 80% in the first event.3, 5, 7 The recurÂrence rate
of hemoptysis post-embolization ranges from 10% to 55%, so surgery plays a
crucial role among therapeutic options through the resection of the affected
lung tissue.8,
12
The objective of this article is
to describe the demographic and diagnostic characteristics and the therapeutic
approaches used in patients with hemoptysis at a reference hospital.
MATERIALS AND METHODS
A retrospective study was
conducted at the Instituto NacioÂnal
de Enfermedades Respiratorias
Ismael CosÃo Villegas during the period from January 2014
to December 2016. The study included patients older than 18 years diagnosed
with hemoptysis who were treated in the Emergency DeÂpartment and admitted to
the hospital, and then underwent embolization at the Hemodynamics Service.
Patients with incomplete medical records were excluded.
The clinical data collected
included demographic information (age, gender), associated comorbidities (diaÂbetes,
hypertension, tuberculosis, smoking), etiology of hemoptysis, management of
hemoptysis, bleeding time, length of hospital stay, characteristics of embolizations, and surgeries.
The bleeding time was measured
from time of arrival in the Emergency Department until treatment. All patients
underwent computed tomography angiography and bronÂchoscopy to confirm the bleeding
and its etiology.
Ethical considerations
This study was conducted in
accordance with the guidelines of the Ethics Committee of the Instituto Nacional de EnÂfermedades Respiratorias
Ismael CosÃo Villegas, following the protocol with
the evaluation of medical records and in accordance with the Declaration of
Helsinki (1964).
Statistical analysis
Categorical variables are
presented as frequency and percentage. For quantitative variables, the Shapiro-Wilk test was conducted to determine the distribution of
each variable. Variables with normal distribution are presented with mean and
standard deviation, while variables without normal distribution are presented
with median and perÂcentiles (25th-75th). Statistical analysis was performed
using the STATA program, version 14 (Stata
Corporation, College Station, Texas, USA). A p-value of less than 0.05 was
considered statistically significant.
RESULTS
A total of 34 patients with
hemoptysis who unÂderwent embolization were included in the study. 52.9% were
men, with a mean age of 52.4 ± 14.5 years. The volume of bleeding was 225 mL
(ranging from 100 to 350 mL), and the mean evolution time before treatment was
3 days (Table 1).
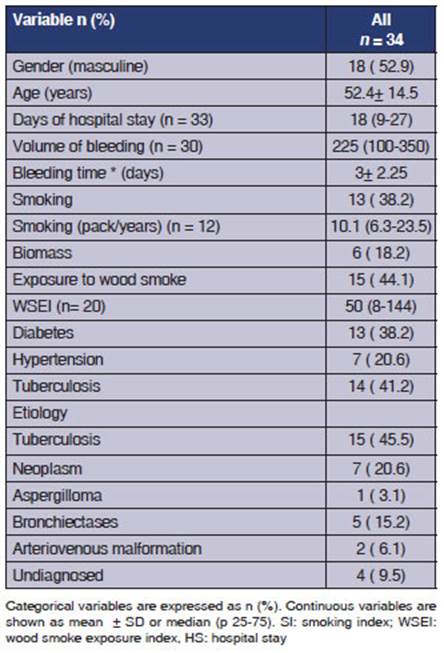
The following comorbidities were found:
diabeÂtes mellitus (DM) in 38.2% of cases, systemic arteÂrial hypertension
(SAHT) in 20.5%, and pulmonary tuberculosis (PTB) in 38.2% (Table 1). Regarding
the etiology of the bleeding, PTB was identified as the primary cause in 46.8%
of cases, followed by neoplasms in 31.2%, bronchiectases
in 15.6%, and arteriovenous malformation (AVM) in
6.2% After confirming the bleeding and its origin
through the CT angiography, the patients underwent embolizaÂtion at the
Hemodynamics Service (Table 1).
The bleeding was
successfully controlled in the first procedure for 81.2% of the patients, while
18.7% of the individuals required a second emboÂlization due to recurrence. In
93.7% of the cases, microspheres of alcohol were used, and 6.4% were treated
with coils. The most commonly embolized arteries were
bronchial arteries (n = 10), mamÂmary arteries (n = 8), and the phrenic artery
(n=3) (Table 2).
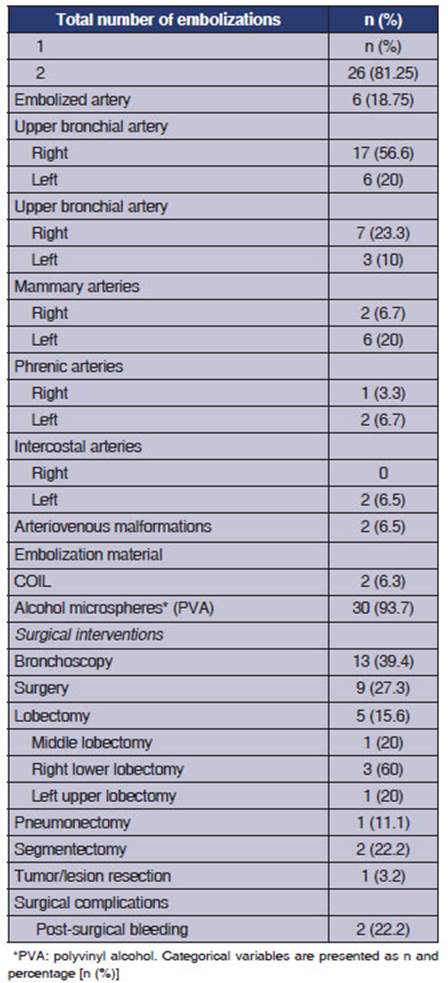
Surgery was necessary
for 9 patients, 5 of which required lobectomy: 3 in the right lower lobe, 1 in
the left upper lobe, and 1 in the middle lobe. One patient had bleeding from a
left cavitated lesion that required pneumonectomy due to extensive parenchymal damage, and one underwent non-anatomical pulmonary resection
of the bleeding-causing lesion (Table 2).
DISCUSSION
A total of 34
patients who underwent embolization due to hemoptysis were evaluated, and a 81.2% success rate was found in the first event. 7
patients underwent surgery as definitive treatment. Six patients required a
second embolization due to recurrent bleeding. Fructer
et al reported that BAE is highly effective for hemoptysis control and has
adequate long-term efficacy, except when the bleeding is secondary to lung
cancer or bronchiecÂtasis, where embolization is a temporary measure prior to
surgery.13
While most cases of
hemoptysis are self-limiting, the presence of massive bleeding can lead to a
mortality rate ranging from 10% to 60%.13 In
the same series by Furcher et al, the recurrence of
bleeding within the first 30 days after embolization was reported at 31.2%, and
22.9% for the period of more than 30 days after embolization. Long-term
recurrence following embolization ranges from 10% to 60% and is attributed to
occluded vessel recanalization or neovascularization when the etiology has not
been treated, such as in cases of aspergilloma and
cancer.13, 14 4 patients of our group experienced a new bleeding
episode within one month of the initial embolization and required
re-intervention, while in another patient, bleeding recurred at 93 days. Two
patients (33.3%) of the group who experienced hemoptysis recurrence eventually
underwent surgery as definitive treatÂment.
The most common embolization
agents are polyvinyl alcohol (PVA), ranging from 150 μm to 1200 μm (with 300 μm to 500 μm being the most common size). PVA is non-absorbable and has a permanent
occlusive effect. The use of microÂspheres of less than 300 μm is not recommended, as they could cross bronchopulmonary
anastomoses of 325 μm and cause microinfarctions.9, 15
In existing reports,
the predominant causes of hemoptysis are pulmonary tuberculosis, bronÂchiectases, mycetomas, and cancer.
Clearly, the source of the bleeding can be in the airway, the pulmonary
parenchyma, or even the large-caliber vessels. It is important to consider that
regardÂless of the cause, bleeding can occur in a volume significant enough to
obstruct the airway and impede gas exchange. In our review, we found that
nearly 45.5% of hemoptysis cases were caused by pulmonary tuberculosis, while
cancer accounted for 20.6%, followed by bronchiectasis with 15.2%. The etiology
of hemoptysis varies significantly according to the different reports due to
the timÂing of the study and sociodemographic
factors. Our data align with countries like China, Hong Kong, and India, where
tuberculosis is the leadÂing cause.1, 16, 17
None of the patients
we treated with embolizaÂtion experienced bleeding of more than 350 mL,
resulting in a stable evolution. Surgical resection is not recommended as the
initial treatment for heÂmoptysis, though surgery has proven to be useful,
particularly in cases of massive bleeding recurring within 72 hours or when an
endovascular techÂnique is not anatomically feasible. Surgery is also
considered for lesions such as tumors or cavitations
with a risk of rebleeding. Among patients who
underwent surgery, mortality rates ranging from 2% to 18% have been reported,
but in emergency surgeries, the mortality rate rises to 50%.1, 16, 18
Hemoptysis requires a
well-organized multidisÂciplinary approach. Its presence has been associÂated
with mortality rates between 25% and 50%. It can be classified based on its
origin, the volume of the bleeding, or the etiology inducing it.19
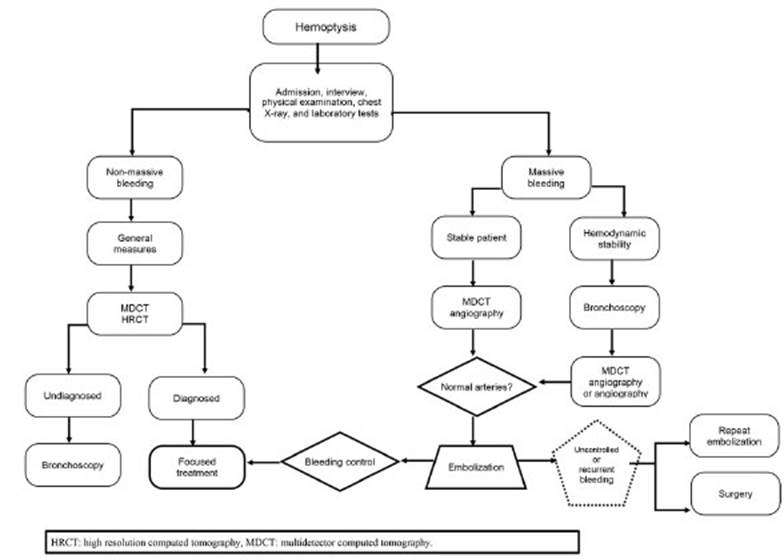
This study provides
an overview of the emboliÂzation treatment and offers insights into existing
literature. Finally, it shows the management opÂtion suggested by a tertiary
care institution. This study paves the way for a prospective evaluation to
implement a management and treatment protocol for patient evolution (Figure 1).
Limitations
The main limitation
of the study is the fact that the results are derived from a retrospective
analysis and a single center. We believe that the obtained results are adequate
for patients with hemoptysis undergoing embolization and are consistent with
the existing literature. We propose conducting a prospective study and setting
a unified care protoÂcol to achieve better control over patient outcomes and
evolution.
CONCLUSIONS
Patients with hemoptysis should
be evaluated in units equipped with both human and material resources specialized
in respiratory emergencies. Stabilizing a patient by securing the airway is of
utmost importance; subsequently, the bleeding site should be identified, and as
the first therapeutic option, embolization with polyvinyl alcohol microÂspheres
or coils should be performed, with surgery as a last resort.
Conflict of interest
The authors of this article have
no conflicts of interest among themselves or with any institution.
Funding
This research did not receive
funding from any source.
REFERENCES
1.
Cordovilla R, Bollo de Miguel E, Nunez
Ares A, Cosano Povedano FJ, Herráez Ortega I, Jiménez
Merchán R. Diagnosis and Treatment of Hemoptysis. Archivos de bronÂconeumologia. 2016;52:368-77.
https://doi.org/10.1016/j.arbr.2016.05.010
2. Bulut
D, Maier K, Bulut-Streich N, Borgel
J, Hanefeld C, Mugge A.
Circulating endothelial microparticles correlate
inversely with endothelial function in patients with ischÂemic left ventricular
dysfunction. J Card Fail. 2008;14:336- 40.
https://doi.org/10.1016/j.cardfail.2007.11.002
3. Ittrich
H, Bockhorn M, Klose H,
Simon M. The Diagnosis and Treatment of Hemoptysis. Dtsch Arztebl Int.2017;114:371- 81. https://doi.org/10.3238/arztebl.2017.0371
4. Ittrich
H, Bockhorn M, Klose H,
Simon M. DiagnosÂtik und Therapie
der Hämoptysen. Dtsch Arztebl
Int.. 2017;114:371-81.
5.
Larici AR, Franchi P, Occhipinti M, Contegiacomo A, del
Ciello A, Calandriello L,
et al. Diagnosis and
management of hemoptysis.Diagn
Interv Radiol 2014;20:299-309. https://doi.org/10.3238/arztebl.2017.0371
6. Ong ZY, Chai HZ, How CH, Koh J,
Low TB.A simplified approach to haemoptysis. Singapore Med J. 2016;57:415-8.
https://doi.org/10.11622/smedj.2016130
7. Kang MJ, Kim JH, Kim YK, Lee
HJ, Shin KM, Kim JI, et al. 2018 Korean Clinical Imaging Guideline for
Hemoptysis. Korean J Radiol.
2018;19:866-71.
https://doi.org/10.3348/kjr.2018.19.5.866
8. Radchenko
C, Alraiyes AH, Shojaee S. A systematic apÂproach to the management of massive hemoptysis.
J Thoracic Dis. 2017;9(Suppl
10):S1069-s86. https://doi.org/10.3348/kjr.2018.19.5.866
9. Cody O’Dell M, Gill AE,
Hawkins CM. Bronchial Artery Embolization for the Treatment of Acute
Hemoptysis. Tech Vasc Interv Radiol. 2017;20:263-5. https://doi.org/10.1053/j.tvir.2017.10.006
10. Mondoni
M, Carlucci P, Cipolla G, Fois
A, Gasparini S, Marani
S, et al. Bronchoscopy to assess patients with heÂmoptysis: which is the
optimal timing? BMC Pulm Med. 2019;19:36.
https://doi.org/10.1186/s12890-019-0795-9
11. Torbiarczyk
JM, Sobczak PA, Torbiarczyk
KK, Milkowska- Dymanowska
J, Antczak A, Gorski P, et
al. Is bronchoscopy always justified in diagnosis of haemoptysis?
Adv Respir Med. 2018;86:13-6. https://doi.org/10.5603/ARM.2018.0004
12. Lu MS, Liu HP, Yeh CH, Wu YC, Liu YH, Hsieh MJ, et al. The
role of surgery in hemoptysis caused by thoracic actinomycosis;
a forgotten disease. Eur J Cardiothorac
Surg. 2003;24:694-8. https://doi.org/10.1016/S1010-7940(03)00515-3
13. Fruchter
O, Schneer S, Rusanov V, Belenky A, Kramer MR. Bronchial artery embolization for
massive hemoptyÂsis: long-term follow-up. Asian Cardiovasc
Thorac Ann. 2015;23:55-60.
https://doi.org/10.1177/0218492314544310
14. Khalil A, Fedida
B, Parrot A, Haddad S, Fartoukh M, Carette MF. Severe hemoptysis: From diagnosis to emÂbolization.
Diagn Interv Imag. 2015;96:775-88.
https://doi.org/10.1016/j.diii.2015.06.007
15. Panda A, Bhalla
AS, Goyal A. Bronchial artery embolization in
hemoptysis: a systematic review. Diagn Interv Radiol . 2017;23:307-17.
https://doi.org/10.5152/dir.2017.16454
16. Gagnon S, Quigley N, Dutau H, Delage A, Fortin M. ApÂproach
to Hemoptysis in the Modern Era. Can Resp J. 2017;2017:1565030. https://doi.org/10.1155/2017/1565030
17. Davidson K, Shojaee S. Managing Massive HemopÂtysis. Chest.
2020;157:77-88.
https://doi.org/10.1016/j.chest.2019.07.012
18. Kiral
H, Evman S, Tezel C, Alpay
L, Lacin T, Baysungur V, et
al. Pulmonary resection in the treatment of life-threatening hemoptysis. Ann Thorac Cardiovasc Surg. 2015:oa.
14- 00164. https://doi.org/10.5761/atcs.oa.14-00164
19. Yun JS, Song SY, Na KJ, Kim
S, Jang K-H, Jeong IS, et al. Surgery for hemoptysis
in patients with benign lung disÂease. J Thorac Dis.
2018;10:3532. https://doi.org/10.21037/jtd.2018.05.122