Autor :Rey, DarÃo RaÚl1, SÃvori, MartÃn SÃvori2
1 Director of the Specialization Career, UBA (University of Buenos Aires), Academic Unit, Hospital TornÚ 2 Director of the Specialization Career, UBA, Academic Unit, Hospital Ramos MejÃa
https://doi.org/10.56538/ramr.KJRC8333
Correspondencia : Dario Rey. E-mail: darioraul.rey@gmail.com
ABSTRACT
We present a case initially
interpreted as allergic asthma triggered by dog hair and later confirmed as
non-fibrotic hypersensitivity pneumonitis (HP) associated with domestic
environmental conditions.
Key words: Bronchial hyperreactivity, Hypersensitivity
pneumonitis, Allergy to domestic dogs
RESUMEN
Se
presenta un caso clÃnico interpretado al principio como asma alÃĐrgica al pelo
de perro y luego documentado como neumonitis por hipersensibilidad (NHS) no fibrÃģtica vinculada al antecedente ambiental domÃĐstico.
Palabras
clave: Hiperreactividad
bronquial, Neumonitis por hipersensibilidad, Alergia a perros domÃĐsticos
Received: 02/12/2023
Accepted: 04/14/2023
CASE REPORT
44-year-old male
patient. After adopting 2 dogs, the
patient began to show unproductive cough due to bronchospasm, which required
periodic visits to the Emergency Room. He was treated with aerosolized
salbutamol on-demand because the animals live in an open space in the garden,
and in a kennel away from the house. It had been interpreted as bronchial hyperreactivity to dog hair. The patient reported having
suffered bronchial asthma from childhood to adolescence, when it had subsided.
He consulted for unproductive
cough. The physiÂcal examination showed 98% SO2
and auscultation showed moderate hypoventilation in both hemoÂthorax with little wheezing at the bases. He was
medicated with formoterol + budesonide aerosol
(160/4.5mcg) tid, and fexofenadine, betamethasone and
salbutamol on-demand. At 7 days, he presentÂed very good clinical and
symptomatic evolution. The following tests were requested:
â Lab tests: no particularities.
â Spirometry
(with/without bronchodilators): FVC 4390/5410 ml (94/100% predicted), FEV1 2370/2640 ml
(67/76% predicted), FEV1/FVC:
0.71, response to bronchodilators in FEV1:
15%
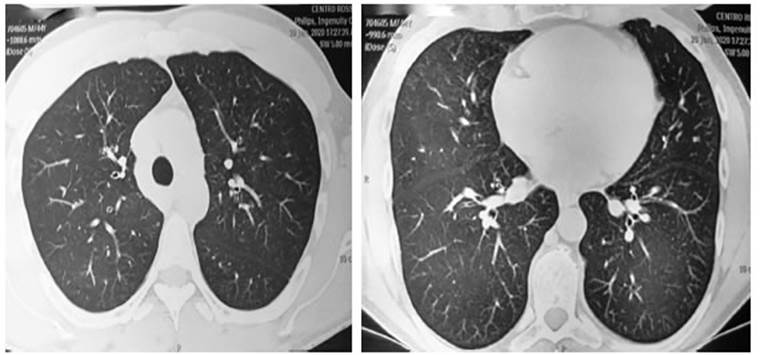
â High resolution computed axial
tomography (HRCAT): inflammatory changes in the bronÂchial wall and areas of
increased attenuation with a âground-glassâ appearance in the posterior segment
of the right upper lobe and the apicoposterior
segment of the left upper lobe (Figure 1).

The current clinical condition
was interpreted as hypersensitivity pneumonitis (HP) with a non-fibrotic
phenotype. Oral prednisone was preÂscribed at a dose of 0.5 mg/kg/day for 15
days, with dose tapering over the following six weeks until complete clinical
remission was achieved. At the two-month follow-up, the patient presented good
general health and was asymptomatic, with normal respiratory signs. The spirometry showed imÂproved FEV1 but with persistent moderate airflow
obstruction. The HRCAT showed the resolution of the ground-glass opacities
(Figure 2). The patient was advised to continue using bronchodilator medication
and to adhere to complete vaccination schedules, including influenza,
pneumococcal, 2-in-1 for adults, and SARS-CoV-2 vaccines.
COMMENT
Various studies show that 10-20%
of the world population is affected by allergies to domestic dogs and cats,
which is a health problem.1-2 Likewise,
there are analogous allergies to owls, parakeets, pheasants, chinchillas, and
cockatoos.1-2 Due to the
frequent prevalence of dog and cat allergens, there is an essential need to
accurately diagnose and treat this allergy in order to reduce morbidity and
mortality from exposure.1-2 The high
prevalence of allergic diseases, including rhinoconjunctivitis
and bronchial asthma, is associated with significant individual morbidity as
well as high social costs, including the loss of work productivity. Among
adults who are allergic to household dogs, asthma exacerbation costs add from
$500 to $1,000 million in the United States.3
Determinations made by elements
of senÂsitization to allergenic proteins contribute to significantly improve
the diagnosis.4 The ability
to accurately identify individuals susceptible to dogs and cats is essential to
reduce the burden of asthma and allergic rhinitis by allowing a better
assessment of therapeutic efficacy. Unlike patients with allergy to cats, the
diagnosis and treatment of patients with allergy to dogs are still a chalÂlenge.
Continuous exposure to animal allergens leads to sensitization and progression
to clinical allergic symptoms.4 Diagnostic
agreement is only 52.2% between skin tests and dog-specific serum allergen IgE test. There is still a great difficulty in using skin
prick tests to detect dog allergies in patients. Commercially available
extracts used in such tests consist of several proteins whose dosage varies
considerably. Domestic animals and humans share and exchange
pathogens, microbiomes, and lipocalins
through secretions and dermal shedding. The latter can show a faulty
load of allergens, and in that case they may induce Th2 hypersensitivÂity.5 Allergenic
components have been identified in the serum, dander, skin, hair, saliva, and
urine of dogs. Initial studies revealed the importance of the allergenic
component Can f 1 (canis familiaris allergen 1) suggesting that dander is the
preferred source for most commercial preparations of allerÂgenic extracts for
dogs.5 Gradually,
canine proteins have been differentiated and isolated. Currently, there are
seven canine allergens identified as Can f 1-7 by the International Union of
Immunological Societies. Although many are classified as âimporÂtantâ
allergens, only 50% of allergic patients react to them, and none of them has
been identified as having a high degree of reactivity.6
With regard to treatment, in order to control clinical symptoms,
patients are mostly advised to avoid exposure to the animal. The animals should
be bathed two times a week to minimize dander, saliva, skin shedding, and hair.7 Separation or
exclusion of the pet will not contribute to reducing symptoms, especially if
there are carpets in the house, since allergens, which are stable, can remain
in the environment for up to 6 months. Symptom manÂagement with antihistamines
and steroids (CS) is used when preventive and therapeutic strategies have
already been used but symptoms persist.7
Finally, subcutaneous immunotherapy is
effecÂtive, but less effective than for cat allergies. This gradual
introduction of allergens at constant and gradually increasing doses over 3 to
5 years is related to changes in the function of Th2 cells to a Th1 phenotype
and the induction of regulatory T cells. Publications on dog immunotherapy from
1963 showed symptom attenuation in 11 patients treated with dog allergenic
extracts.7
Treatment with immunotherapy
depends on reliable and safe extracts. The safety of the subcuÂtaneous route is
also a concern: if a patient is very sensitive, different batches produced by
the same manufacturer with varying amounts of allergenic protein components can
lead to adverse reactions when these individuals are suddenly exposed to high
levels. Desensitization treatment can also be done intradermally
(ID), which may last for 3 to 5 years through the administration by qualified
personnel. In the last 20 to 30 years, the sublingual route (SL) has gained
gradual recognition. Since the clinical indications for both administration
routes overlap, if SL is available, it might be preÂferred by some patients due
to the convenience of administration, although ID is considered more effective.10
Exposure to pets has been
considered a risk factor for asthma. Takkouche et al
examined the association between pet exposure, asthma, and allergic rhinitis
through a meta-analysis.10 In 32 articles,
the risk for asthma related to exposure to any pet was 1.39 (95% CI:
1.00-1.95), and for dogs, it was 1.14 (95% CI: 1.01-1.29). Among cohort
studies, exposure to cats yielded a relative risk of 0.72 (95% CI: 0.55-0.93),
while for allergic rhinitis, the relative risk of exposure to any pet was 0.79
(95% CI: 0.68-0.93)10.
The authorsâ conclusion was that exposure to cats has a slight preventive
effect on asthma, which is more evident in cohort studies. Exposure to dogs
slightly increases the risk of asthma.10
The patient of this case had not
undergone any diagnostic test to confirm his allergy to dog hair. Instead, he
had been treated symptomatically with environmental avoidance measures and
prevenÂtive inhaled bronchial medication (budesonide/ formoterol),
antihistamines, and corticosteroids, which had resulted in clinical
improvement.
Furthermore, HP is an
immune-related disÂease that manifests in susceptible individuals following
exposure to identified or unidentified environmental agents.11
Several definitions have been proposed, but the experts havenât
reached a consensus.11 According to
the new ATS/ERS/ ALAT/JRS Guidelines, the characteristic pattern of
non-fibrotic HP is identified tomographically by centrilobular nodules, mosaic attenuation during
inspiration, air trapping during expiration, and a âground glassâ appearance.11 In HP, the moÂsaic
attenuation (manifested distinctively) shows that lobes affected by pneumonitis
(increased attenuation) alternate with lobes of normal or slightly decreased
attenuation due to bronchiolar obstruction.11
They tend to be bilateral and symÂmetrical with diffuse
distribution, both coronal and axial.11 Although this pattern of
irregularities sugÂgests non-fibrotic HP, isolated air trapping is anÂother
potential pattern to be found in this variant. Following the latest evaluation,
the patient was interpreted as having the non-fibrotic phenotype of HP. It
should have been completed with a bronÂchoalveolar
lavage (BAL).11 Typically,
the presence of a higher lymphocyte count distinguishes fibrotic HP from sarcoidosis and idiopathic pulmonary fibrosis, and
non-fibrotic HP from sarcoidosis.11 Serum
determination of IgG against the suspected antigen is
also useful, but it is not available in the country.12
Due to the patientâs history of contact, clinical symptoms, HRCAT
findings, and theraÂpeutic response, the decision was made to skip this step.
The percentage of lymphocytes in the HP BAL is equal to or greater than 20%.11The
recomÂmended treatment for the non-fibrotic phenotype of HP is prednisone or
equivalent at 0.5 mg/kg/day for 1-2 weeks, followed by a gradual reduction to a
maintenance dose of 10 mg/day for 2 to 4 weeks. To avoid the adverse effects of
CS, mycophenolate and azathioprine can be used,
especially in patients who experience relapse or progression when good
environmental control is not feasible.12
The patient responded rapidly to decreasing doses of predniÂsone
over two months. In contrast, for the fibrotic phenotype of HP, with limited
evidence, CS can be used alone or in combination with mycophenolate
and azathioprine at decreasing doses for up to six months, though a few
patients may require lifelong treatment.12
Rituximab, a monoclonal antibody targeting CD20 could be useful,
especially if there is no pattern of usual interstitial pneumonia or
non-specific interstitial pneumonia.
Anti-fibrotic drugs like pirfenidone and nintÂedanib are
also being studied for this indication, particularly if the disease progresses
with a usual interstitial pneumonia pattern.12
In conclusion, we present the
case of a patient with allergic asthma triggered by dog hair who
later developed non-fibrotic phenotype hypersenÂsitivity pneumonitis (HP). The
patient was treated with prednisone for less than three months until
discontinuation, resulting in the remission of tomographic images and
improvement in respiraÂtory symptoms.
REFERENCES
1.
DÃaz Perales A, GonzÃĄlez de Olano D, PÃĐrez Gordo M, et al. Allergy to uncommon pets: new allergies but the same alÂlergens. Front Immunol 2013;4:1-6.
https://doi.org/10.3389/fimmu.2013.00492
2. Partridge SJ, Pepperell JC,
Forrester-Wood C, Ibrahim NB, Raynal A, Swinburn CR. Pheasant rearerâs
lung. Occup Med (Lond). 2004;54:500-3. https://doi.org/10.1093/occmed/kqh092
3. Hellgren
J, Cervin A, Nordling S,
Bergman A, Cardell LO. Allergic
rhinitis and the common cold-high cost to society. Allergy.
2010;65:776-83.
https://doi.org/10.1111/j.1398-9995.2009.02269.x
4. Chan SK, Leung DYM. Dog and
Cat Allergies: Current State of Diagnostic Approaches and Challenges. Allergy Asthma
Immunol Res. 2018;10:97-105.
https://doi.org/10.4168/aair.2018.10.2.97
5.
Jensen Jarolim E, Pacios L,
Bianchini R, et al. Structural similarities of human and mammalian lipocalins,
and their function in innate immunity and allergy. Allergy 2016; 71: 286-94. https://doi.org/10.1111/all.12797
6. Virtanen T. Immunotherapy for
pet allergies. Hum Vaccin Immunother.
2018;14:807-14. https://doi.org/10.1080/216
45515.2017.1409315
7. Dhami
S, Kakourou A, Asamoah F,
et al. Allergen immuÂnotherapy for allergic asthma: A systematic review and
meta-analysis. Clin Transl
Allergy 2017;7:25-36.
https://doi.org/10.1186/s13601-017-0160-0
8. Smith DM, Coop CA. Dog
allergen immunotherapy: past, present, and future. Ann
Allergy Asthma Immunol. 2016;116:188-93.
https://doi.org/10.1016/j.anai.2015.12.006
9. Hodson
T, Custovic A, Simpson A, Chapman M, Woodcock A,
Green R. Washing the dog reduces dog allergen levels, but the dog needs to be
washed twice a week. J Allergy Clin
Immunol. 1999;103:581-5.
https://doi.org/10.1016/S0091-6749(99)70227-7
10. Takkouche
B, GonzÃĄlez-Barcala FJ, Etminan
M, FitzgerÂald M. Exposure to furry pets and the risk of asthma and allergic
rhinitis: a meta-analysis. Allergy. 2008;63:857-64. https://doi.org/10.1111/j.1398-9995.2008.01732.x
11. Raghu G, Remy-Jardin M, Ryerson CJ, et al. Diagnosis of Hypersensitivity
Pneumonitis in Adults. An Official ATS/JRS/ALAT Clinical
Practice Guideline. Am J Respir Crit Care Med 2020; 202:e36-e69.
https://doi.org/10.1164/rccm.202005-2032ST
12. Alberti
ML, RincÃģn-Ãlvarez E, BuendÃa-RoldÃĄn
I, Selman M. Hypersensitivity Pneumonitis: Diagnostic
and TheraÂpeutic Challenges. Front Med (Lausanne).
2021;8:718299. https://doi.org/10.3389/fmed.2021.718299