Autor : De Vito, Eduardo L1,2, Arce, Santiago C.1, Monteiro, Sergio G.1
1 Instituto de Investigaciones MĂ©dicas Alfredo Lanari, Faculty of Medicine, Universidad de Buenos Aires, Buenos Aires, Argentina. 2 Centro del Parque, Respiratory Care, Buenos Aires, Argentina.
https://doi.org/10.56538/ramr.RTJY6802
Correspondencia : Eduardo Luis De Vito, E-mail: eldevito@gmail.com
ABSTRACT
This
article is the first in a series dedicated to that strange phenomenon of life
caught halfway between consciousness and unconsciousness: dyspnea. The article
provides information on the definitions of dyspnea over time and presents the
evolution of ideas that led to the understanding of its mechanisms. The
relevance of each of these mechaÂnisms must be evaluated in the context of each
specific clinical and pathophysiological situation. The experience of dyspnea
begins to be seen as a multidimensional phenomÂenon that must be focused
on what the patient perceives. Considering the complexity of the experience and
its multiple dimensions, it is possible for new therapeutic options to be
developed in future times.
Key words: Dyspnea;
Respiratory Distress Syndrome; Definitions; Physiology; Physiopathology
RESUMEN
Este
artículo es el primero de una serie dedicada a ese extraño
fenómeno de la vida atrapado a medio camino entre lo consciente y lo
inconsciente: la disnea. El artículo proporciona información
sobre las definiciones a lo largo del tiempo y presenta la evoÂlución de
las ideas que hicieron a la comprensión de sus mecanismos. La relevancia
de cada uno de ellos debe evaluarse en el contexto de cada situación
clínica y fisiopaÂtológica específica. La experiencia de
la disnea comienza a ser vista como un fenómeno multidimensional que
debe estar centrado en lo que percibe el paciente. Considerando la complejidad
de la experiencia y su multidimensión, es posible que se desarrollen
nuevas opciones terapéuticas en tiempos venideros.
Palabras
clave: Síndrome
de Dificultad Respiratoria; Disnea; Definición; Fisiología;
Fisiopatología
Received: 25/11/2022
Accepted: 09/03/2023
INTRODUCTION
The
survival of our ancestors required strenuÂous physical activity. The
respiratory discomfort experienced during that activity surely generated
concern, but if it occurred at rest, the distress, fear, and uncertainty could
have been unbearable. Due to his lack of understanding, the primitive man
sought relief the best way he could, and attributed his symptoms to
supernatural forces. Today we unÂderstand that, both yesterday and today,
dyspnea is a primary experience associated with behaviors aimed at countering a
threat to survival.
Undoubtedly,
respiratory discomfort is one of the most distressing and frightening symptoms
perceived by humans,1 not only for
those who sufÂfer from it but also for their caregivers. Dyspnea is a symptom
that can occur in very different respiratory and cardiovascular conditions, as
well as in cancer, anemia, anxiety, and psychosomatic disorders, during
exercise, or during respiratory loads in normal subjects.2
This entity should be considered independently from other
respiratory variables and physical sensations such as tachyÂpnea, use of
accessory muscles, hyperventilation or hyperpnea, and is different from the
sensation of bodily effort and general fatigue or asthenia.
Physical
activity, anxiety levels, onset speed, and experience can influence the
perception and intenÂsity of dyspnea.3
Its prevalence varies according to the type of disorder and the
progression stage. In the early stages of certain diseases, it may be
circumstantial, reversible, and self-limiting, but it can become very difficult
to alleviate as the disÂease progresses and, despite the best medical care,
when it is difficult to control, it can deteriorate the quality of life of the
patient and his/her close environment. Dyspnea is an independent predictor of
mortality and is more related to quality of life than to lung function tests.3, 4
The
possibility of improving the quality of care for patients with dyspnea depends
on our ability to define the mechanisms involved, to break down all
communication barriers between us and the paÂtient, and to understand that
dyspnea (similarly to pain) has physical, psychological, social, cultural, and
spiritual components.3
Using
the key word “dyspnea”, the PubMed® database as of March 2022 yields just over
65,000 quotations.5 There has been
an increase in the number of publications since 1963, when Grupo Campbell proposed
the lack of adjustment between tension and length as a central cause in its genÂeration.6, 7 Their highly
influential work will be analyzed in the second part of this series.
This
article provides information on the defiÂnitions and mechanisms of dyspnea from
a hisÂtorical perspective, and highlights the areas of interest for future
research. While the earliest references to dyspnea date back to Hippocrates
(406-360 BC), the history of the evolution of ideas about its mechanisms dates
back to about 120 years.
Evolution of the definition of dyspnea
Most
people have experienced shortness of breath and intuitively know what the term
means, howÂever, since the times of Cockroft and Guz, the need for an
operational definition that allows for its quantification and the performance
of experiÂmental studies became evident. The semantics of breathlessness
generated confusion. The terms “dyspnea” (dyspnoea in UK), breathlessness, and
shortness of breath are often interchangeable. The expression “breathlessness”,
easily understandÂable for patients, is frequently used by them and their
environment.8
History of the definitions of dyspnea and its components
In 1923, Jonathan Meakins defined dyspnea as the awareness of the need to increase the respiraÂtory effort.9 By the 1960s, Julius Comroe, in his legendary book, used the word dyspnea to connote a symptom, a sensory experience that, like pain, can only be perceived and judged by the patient.10 In 1971, in the classic book by Bates, Macklem, and Christie, the authors defined dyspnea as the awareÂness of the respiratory effort.8, 11 In the 1980s, Burky defined it as a pathological shortness of breath, as opposed to the shortness of breath that appears in situations where such difficulty could be expected, such as during exercise.12 Campbell and Guz13 defined dyspnea as a common sensation of uncomfortable breathing, whereas Killian and Jones14 characterized it as the awareness of the motor effector command to the inspiratory muscles and later as a quantitative sensation without a threshold of the required motor effort of the respiÂratory muscles.15 In the 1990s, Malher defined it as a medical term used to characterize a nonspecific sensation of shortness of breath.16 More recently, Killian specified dyspnea as a term commonly used to represent discomfort experienced in association with the act of breathing.17
There
is general agreement that the discomfort of dyspnea comprises two main
elements:
–
An urge to breathe, commonly referred to as “air hunger”.
–
A sensation of excessive effort (inspiratory effort sensation) associated with
breathing.18
Although
the sensations of air hunger and effort usually increase together, they can be
experimenÂtally separated. Dyspnea in an individual patient can represent a
combination of these sensations and can explain the different qualities
(descripÂtors) of dyspnea.
Unlike
localized sensations, such as touch and temperature, which mostly arise from
the stimuÂlation of a defined peripheral receptor, dyspnea is a vague visceral
sensation, analogous to thirst or hunger. In addition, the different sensations
of dyspnea do not usually occur in isolation. The sensation of dyspnea can vary
both in the degree of discomfort and in its emotional and behavioral significance.19, 20
Pathological or
physiological dyspnea?
It has been suggested that there is no accurate boundary between the “pathological” shortness of breath of the disease and the “physiological” dyspnea in normal individuals during intense exÂercise. Many patients report that the dyspnea they have now is qualitatively similar to the one they experienced during intense exercise, but now it occurs with light physical activity or even at rest.21
If
we define dyspnea as the awareness of labored breathing or as air hunger, it
implies an underlying pathological process. That is to say, the sensation must
be experienced in association with a physical activity that should not be
generating respiratory discomfort based on the individual’s experience. However,
it has been demonstrated that normal subjects have unpleasant respiratory
sensations with exercise that can limit their performance and can be considered
as dyspnea.
The
emotional component of the sensory experiÂence may vary if the dyspnea occurs unexpectedly,
but whether the quality of the sensation is differÂent or not, that is not so
evident. A sound of 200 decibels will be bothersome whether or not the subject
is expecting the sound, and most of us exÂperience dyspnea when climbing 10
flights of stairs even when we expect to have shortness of breath.
Should
this sensation be ignored or called something else simply because the
individual has normal lungs and a normal cardiovascular system, and especially
because the difficulty is expected for that physical activity?22
The concept of a sensation that is unexpected or inappropriate
for physical activity is not reasonable: dyspnea is a primary experience
associated with behaviors aimed at countering a threat to survival.
General consensus of
the definition of dyspnea
Trials
of different definitions of dyspnea have resulted from advances in the
knowledge of its mechanisms and multifactorial nature, leading to a consensus
definition proposed by the American Thoracic Society (ATS) some years ago.23
“Term
used to characterize a subjective experiÂence of shortness of breath that
consists of qualiÂtatively different sensations that vary in intensity. The
experience stems from interactions among multiple physiological, psychological,
social, and environmental factors, and can induce secondary physiological and
behavioral responses”.
There
are several aspects to highlight in this definition:
–
The experience is subjective (only the patient can say he/she is
experiencing dyspnea).
–
Different qualities of sensations can be identiÂfied (expressed through
a variety of descriptors).
–
The intensity can vary (and can be evaluated using various scales).
–
The emotional state, personality, experience, and cognitive function of an
individual, as well as social factors, influence the experience and the way the
patient reports such experience.
The
last part of the definition is often not given enough consideration. However,
the sensation of dyspnea has a psychological dimension, just like pain. It is
widely recognized in clinical practice that anxiety and depression can increase
the intensity of dyspnea beyond the alteration of the cardiopulÂmonary function
and can contribute to the degree of disability associated with dyspnea.
The
2012 ATS Consensus Statement proposed that “instruments or groups of
instruments related to dyspnea should be classified as addressing the domains
of sensory-perceptual experience, emoÂtional distress, or symptom/disease
impact and burden.”19
Sensory-perceptual
measures include determiÂnation of intensity (real-time measures of
dyspnea) and sensory quality. Emotional distress can refer to both a
perception of immediate unpleasantness as well as a cognitive evaluative
response or judgÂment about the possible consequences of what is being
perceived (e.g., “if this continues, I may suffocate”). Measures that evaluate
the impact of dyspnea do not directly assess what breathing feels like.19
The
ATS Consensus was categorical: any evaluÂation of dyspnea should attempt to
measure both the intensity and quality of the sensation of
respiratory discomfort, as well as the emotional and behavioral response to
respiratory discomÂfort.19,24 Therefore,
dyspnea represents the sum of pathophysiological and psychological factors that
together result in one of the most common sympÂtoms for which patients seek
medical assistance.
The
therapeutic implication of this ATS defiÂnition recognizes and provides
evidence that strategies to modulate the dyspnea symptom may involve other
dimensions of the experience beyond the physiological domain. These are the
cognitive, sensory, emotional, and behavioral dimensions.
Mechanisms of dyspnea,
a historical perspective
Given
the fact that dyspnea is a perception, studies on its mechanisms must be
limited to human beÂings and are restricted by the difficulty of measurÂing a
subjective experience to underlying neuronal activity. However, for the past
two decades, there has been better understanding of the differences between the
respiratory sensation (the neural activation resulting from the
stimulation of a peÂripheral receptor) and perception (the individual’s
sensitive reaction to that sensation).
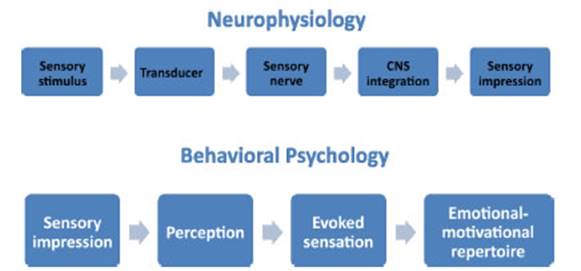
The
pathways involved in the generation of conscious sensations are shown in Figure
1. The upper sequence outlines the neurophysiological pathway from stimulus to
sensory impression, while the lower sequence allows for modulation of the
intensity and quality of symptom perception and is unique to each individual.
The
best understanding of the mechanisms of dyspnea is intimately related to
knowledge in breathing control. In 1905, the ground-breaking work of Haldane
concluded that CO2, acting excluÂsively on the brain, was the dominant
chemoreflex stimulus, and that hypoxia stimulates breathing by acidifying the
brain. This was the vision durÂing the first quarter of the 20th century, but
in 1920, two key observations indicated that this scenario was incorrect.
First, it was found that arterial pH does not decrease, but rather increases
during hypoxia, indicating that something other than a hydrogen ion was driving
the ventilatory response to hypoxia. It was also shown that during a voluntary
suspension of respiratory movements, the respiratory oscillator in the
brainstem stops, refuting the original concept that corticospinal projections
were the dominant pathway by which the cortex influenced breathing. This
established the importance of supratentorial influence on humans in breathing
control.25, 26 The interaction
of chemical stimuli and respiratory sensations was subsequently confirmed by
Fowler and Remmers.27,
28 Despite
that breakthrough, it was during the second half of the 20th century that the
relationship between the control of ventilation and dyspnea began to be understood.19, 26, 29-31
Table
1 shows the evolution of ideas that led to the understanding of the mechanisms
that generate dyspnea. The more recent ones do not necessarily discard the
previous ones. Due to its complexity, the relevance of each mechanism should be
evaluated in the context of each specific clinical and pathophysiological
situation. The time periods for each of the aspects under evaluation should be
used for guidance purposes.
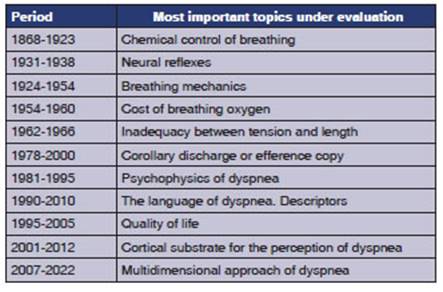
After
almost 120 years, psychometric measureÂments and descriptors of dyspnea have
been added to traditional pathophysiological hypotheses. In the last 30 years,
certain neurophysiological aspects (efference copy-corollary discharge) have
been refined. Only at the end of the 20th century did interest arise in the
quality of life and sufferÂing in the experience of dyspnea.32,33 In the 21st century, brain areas that perceive
dyspnea have begun to be identified, a modern analogue of Wilder Penfield’s
homunculus. The experience of dyspnea is beginning to be seen as a multidimenÂsional
phenomenon that must be centered on what the patient feels.
Integrated analysis of
the dyspnea mechanisms
Although
the precise mechanisms of dyspnea are not fully understood, it is possible to
build a neurobiological model to describe our current understanding of
the perception of dyspnea in parallel with breathing control (Figure 2). The
simplified neurophysiological model describes both the control of breathing
that regulates ventilation and the perception of dyspnea. With the activation
of one or more sensory receptors (chemoreceptors, mechanoreceptors, and those
located in respiraÂtory muscles/chest wall), afferent impulses are transmitted
to the central nervous system (CNS; brainstem, limbic system, and cerebral
cortex) for integration and processing of information. Discriminative and
affective pathways have been proposed. The CNS directs an outgoing motor
command through the phrenic nerves to the reÂspiratory muscles.
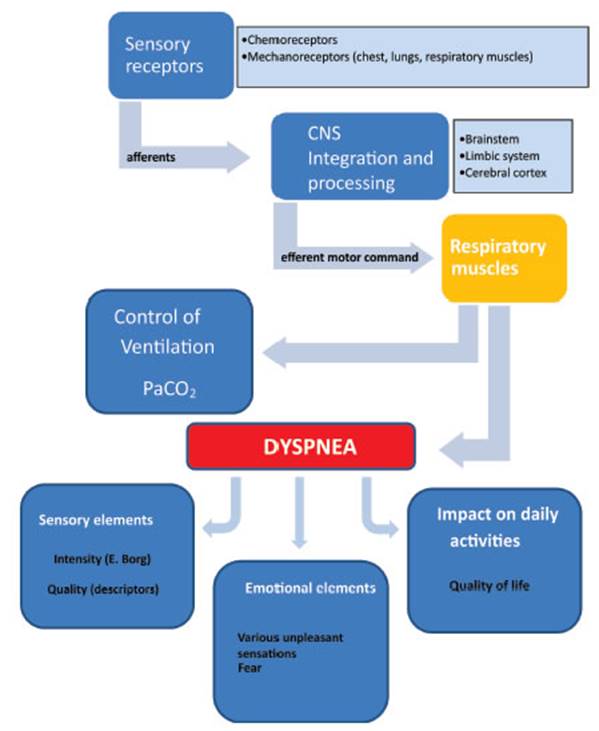
The
different receptors inform the CNS to integrate the information. Dyspnea
results in various elements (sensory, emotional, impact on daily activities).
CONCLUSIONS
In
this first part, we have analyzed the evolution of the definitions of dyspnea
and its mechanisms. Technological breakthrough has undoubtedly alÂlowed for the
exploration of mechanisms that were once inaccessible, and as in many other
fields, the 20th century allowed us to ask questions and answer them like never
before. It is noteworthy that after almost 90 years of studying dyspnea it was
at the end of the 20th century that we started to consider that it could
deteriorate the quality of life and could be measurable. At the beginning of
the 21st century, dyspnea began to be seen as a multidimensional phenomenon that
should be centered on what the patient perceives. The experiÂence of dyspnea
involves both sensory components (intensity and quality) and emotional
components (discomfort, distress) that generally impact or imÂpose a burden
on an individual’s ability to perform daily activities and on his/her quality
of life.
Considering the complexity of the dyspnea exÂperience and its
multiple dimensions, it is possible that new therapeutic options develop in the
future. Making reference to Table 1, in the second part of this series we will
detail the dyspnea production mechanisms.
Key points
– Without a doubt, the discomfort experienced in relation to the
act of breathing - dyspnea - is one of the most distressing and frightening
symptoms perceived by humans, and only the patient can report it.
– Dyspnea should not be ignored in individuals with normal lungs
and a normal cardiovascular system only because the difficulty is the one
expected for physical activity. We think the concepts unexpected or
inappropriate sensation or physiological dyspnea aren’t reasonable.
– We understand that dyspnea is a primary exÂperience associated
with behaviors intended to counteract a threat to survival.
–
It is possible to identify different qualities of sensations; the intensity may
vary, and an indiÂvidual’s emotional state, personality, experience, cognitive
function, as well as social factors can influence the experience of dyspnea and
the way the patient describes it.
–
Therefore, any assessment of dyspnea should attempt to measure the intensity
and quality of the respiratory discomfort sensation and the emotional and
behavioral response to that respiratory discomfort.
–
The possibility of improving the management of patients with dyspnea depends on
our abilÂity to define the mechanisms involved, break down all communication
barriers between us and the patient, and understand that dyspnea (similarly to
pain) has physical, psychological, social, cultural, and spiritual components.
–
The experience of dyspnea is starting to be seen as a multidimensional
phenomenon that should be centered on what the patient perceives.
Conflict
of interest
The
author has no conflict of interest to declare.
REFERENCES
1.
Burki NK, Lee LY. Mechanisms of dyspnea. Chest. 2010;138:1196-201.
https://doi.org/10.1378/chest.10-0534
2.
Fitting JW. Mechanisms of Dyspnea. Current Topics in Rehabilitation. 1991;119-23.
https://doi.org/10.1007/978-1-4471-3782-5_15
3.
Davis CL. ABC of palliative care. Breathlessness, cough, and other respiratory
problems. BMJ. 1997;315:931-4. https://doi.org/10.1136/bmj.315.7113.931
4.
Sarkar S, Amelung PJ. Evaluation of the dyspneic patient in the office. Prim
Care. 2006;33:643-57. https://doi.org/10.1016/j.pop.2006.06.007
5.
PubMed.gov. NIH, U.S. National Library of Medicine. NaÂtional Center for Biotechnology
Information. En: https:// pubmed.ncbi.nlm.nih.gov/ Website [Internet].
6.
Campbell EJM, Howell JBL. The Sensation of Dyspnoea. BMJ. 1963;2:868.
https://doi.org/10.1136/bmj.2.5361.868-c
7.
Howell JBL, Campbell EJM. Breathlessness. Nature. 1965;206:1301–2.
https://doi.org/10.1038/2061301a0
8.
Davis CL. Palliation of breathlessness. Cancer Treat Res. 1999;100:59-73.
https://doi.org/10.1007/978-1-4615-5003-7_4
9.
Meakins J. A British Medical Association Lecture on the cause and treatment of
dyspnoea in cardiovascular disease. Br Med J. 1923;1:1043-5.
https://doi.org/10.1136/bmj.1.3260.1043
10.
Comroe JH, Foster RE, Dubois AB, Briscoe WA, Carlsen E. El pulmón.
Fisiología clínica y pruebas funcionales pulmonares. Editorial
Universitaria; 1964.
11.
Bates DV, Macklem PT, Christie RV, Anthonisen NR. Respiratory Function in
Disease: An Introduction to the Integrated Study of the Lung. WB Saunders,
Philadelphia; 1971. 584 p. (Second Edition).
12.
Burki NK. Dyspnea. Clin Chest Med. 1980;1:47-55. https://doi.org/10.1016/S0272-5231(21)00050-2
13.
Campbell EJM, Guz A. Breathlessness In: Hornbein TF, ed. Regulation of
breathing, part II. New York, NY: Marcel Dekker. 1981;198: 95.
14.
Killian KJ, Jones NL. The use of exercise testing and other methods in the
investigation of dyspnea. Clin Chest Med. 1984;5:99-108.
https://doi.org/10.1016/S0272-5231(21)00235-5
15.
Roussos C, Macklem PT. The Thorax. Roussos C, Macklem PT, editors..Marcel
Decker; 1986;42. https://doi.org/10.1016/S0003-4975(10)61851-6
16.
Mahler DA, Hunter B, Lentine T, Ward J. Locomotor-respiratory coupling develops
in novice female rowers with training. Med Sci Sports Exerc. 1991;23:1362-6.
https://doi.org/10.1249/00005768-199112000-00007
17.
Killian KJ. Nature of breathlessness and its measurement. In: Campbell M,
editor. The Campbell Symposium. BoehÂringer Ingelheim (Canada) Inc; 1993:p1050–1. https://doi.org/10.1136/thx.48.10.1050-c
18.
De Vito EL, Roncoroni AJ, Berizzo EE, Pessolano F. EfÂfects of spontaneous and
hypercapnic hyperventilation on inspiratory effort sensation in normal
subjects. Am J Respir Crit Care Med. 1998;158:107-10.
https://doi.org/10.1164/ajrccm.158.1.9709098
19.
Parshall MB, Schwartzstein RM, Adams L, et al. American Thoracic Society
Committee on Dyspnea. An official AmeriÂcan Thoracic Society statement: update
on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care
Med. 2012;185:435-52. https://doi.org/10.1164/rccm.201111-2042ST
20.
Meek PM, Banzett R, Parsall MB, Gracely RH, SchwartzÂstein RM, Lansing R.
Reliability and validity of the mulÂtidimensional dyspnea profile. Chest. 2012;141:1546-53. https://doi.org/10.1378/chest.11-1087
21.
Cockcroft A, Guz A. Breathlessness. Postgrad Med J. 1987;63:637-41.
https://doi.org/10.1136/pgmj.63.742.637
22.
Schwartzstein RM, Manning HL, Weiss JW, Weinberger SE. Dyspnea: a sensory
experience. Lung. 1990;168:185-99.
https://doi.org/10.1007/BF02719692
23.
Dyspnea. Mechanisms, assessment, and management: a consensus statement.
American Thoracic Society. Am J Respir Crit Care Med. 1999;159:321-40.
https://doi.org/10.1164/ajrccm.159.1.ats898
24.
Scano G, Gigliotti F, Stendardi L, Gagliardi E. DysÂpnea and emotional states
in health and disease. Respir Med. 2013;107:649-55.
https://doi.org/10.1016/j.rmed.2012.12.018
25.
Orem J. The activity of late inspiratory cells during the beÂhavioral
inhibition of inspiration. Brain Res. 1988;458:224-
30. https://doi.org/10.1016/0006-8993(88)90465-9
26.
Remmers JE. A century of control of breathing. Am J Respir Crit Care Med. 2005;172:6-11. https://doi.org/10.1164/rccm.200405-649OE
27.
Fowler WS. Breaking point of breath-holding. J Appl PhysiÂol. 1954;6:539-45. https://doi.org/10.1152/jappl.1954.6.9.539
28.
Remmers JE, Brooks JE 3rd, Tenney SM. Effect of conÂtrolled ventilation on the
tolerable limit of hypercapnia. Respir Physiol. 1968;4:78-90.
https://doi.org/10.1016/0034-5687(68)90009-1
29.
Manning HL, Schwartzstein RM. Pathophysiology of dyspnea. N Engl J Med. 1995;333:1547-53. https://doi.org/10.1056/NEJM199512073332307
30.
Hayen A, Herigstad M, Pattinson KT. UnderstandÂing dyspnea as a complex
individual experience. MaÂturitas. 2013;76:45-50.
https://doi.org/10.1016/j.maturiÂtas.2013.06.005
31.
Stevens SS. The direct estimation of sensory magniÂtudes-loudness. Am J Psychol.
1956;69:1-25. https://doi.org/10.2307/1418112
32.
Mahler DA. Understanding mechanisms and documentÂing plausibility of palliative
interventions for dyspnea. Curr Opin Support Palliat Care. 2011;5:71-6.
https://doi.org/10.1097/SPC.0b013e328345bc84
33.
Mahler DA, O’Donnell DE. Dyspnea: Mechanisms, MeaÂsurement, and Management. CRC
Press. 2014;3:256. https://doi.org/10.1201/b16363