Autor : Abrate, Vanesa del Valle1, Ubal, Leonardo GermÃĄn1, FernÃĄndez, JÃĐsica Noelia1, ElÃas, Marcos Alfonso1, Olmos, MarÃa Eugenia1, Cesaratto, Favio1, Carrizo, MarÃa Fernanda1, Stechina, Juan1, Usedo, NicolÃĄs1, LÃģpez de Navarro, Ana MarÃa1
1 Hospital Privado Universitario de CÃģrdoba
https://doi.org/10.56538/ramr.WBJZ3403
Correspondencia : Abrate Vanesa del Valle Mail: abrate.vanesa@gmail.com
ABSTRACT
Objectives:
To
evaluate the evolution of comorbidities in a cohort of patients with COPD after
5 years of follow-up. To evaluate mortality. To assess and correlate COPD
severity, COPD-specific comorbidity test (COTE) Index, and mortality.
Materials
and Methods: Prospective
observational study in a cohort of patients with COPD during 2015-2020 at the
Pulmonology Service of the Hospital Privado Universitario de CórÂdoba.
Information of electronic medical records. In order to predict the mortality
risks, we used the COTE Index. Statistical analysis: Fisherâs exact test,
Studentâs t test and InfoStat.
Results:
68
patients, 37 male (54.41%), age 75 Âą 6.69. 2 patients lost to follow-up. The
time since COPD diagnosis was 13.23 Âą 5.88 years at the study entry. More than
50% of patients had moderate COPD. There were no differences in
post-bronchodilator FEV1(forced expiratory volume in one second) (0.57 in 2015
vs. 0.58 in 2020), nor in the frequency of exacerbations in the last year (1.06
Âą 1.26 vs. 0.85 Âą 1.44). In 2015, 29.41% of patients (n20) were active smokers,
and the number was reduced to 18.18% (n12). In 2015, 73.53% of patients (n50)
were receiving ICS (inhaled corticosteroids), and in 2020 the number decreased
to 56.92% (n37) (p0.047). In 2015, 4.41% of patients (n3) were receiving
systemic steroids, and the number increased to 20% (n13) in 2020 (p 0.007).
There werenât any significant differences in the frequency of hospitalizations
(0.13 Âą 0.38 vs. 0.97 Âą 2.34). COTE Index ≥ 4; no significant changes
after 5 years: 23.53% (n16) vs. 29.41% (n20). In 2020, an increase in arterial
hypertension (AHT) (66% n45 vs. 77%, p0.181), depression (19.12% n13 vs. 30.30%
n20, p0.161) and anxiety (22.06% n15 vs. 32% n21, p0.243) was detected. In
2020, 3.03% of patients (n2) were diagnosed with abdominal aortic aneurism.
Decrease in obesity from 25% (n17) to 19.70% of patients (n13). During
follow-up, 9 patients died (13.24%), and they had fewer comorbidities (p <
0.009). Higher mortality in patients with COTE Index ≥ 4 (p0.429). Deceased
patients had more severe COPD, with lower post-BD FEV1 after 5 years (p0.102).
Patients with cardiovascular or metabolic disease had a lower mortality rate at
5 years (p < 0.05). Although patients with a COTE Index ≥ 4 in 2015
had a lower mean post-BD FEV1 at baseline and after the 5-year follow-up, the
difference wasnât significant. It was observed that the COTE Index increased in
patients with COPD with post-BD FEV1 of moderate to severe degree (p <
0.05).
Discussion:
The
comorbidities of COPD constitute a prognostic factor with a cumulative effect
on morbidity and mortality. Hence, the importance of this study. One limitation
is the small population size, which could explain the lack of correlation
between mortality and increased comorbidities. We highlight the overuse of ICS
and systemic steroids in this population, despite not experiencing increased
exacerbations or hospitalizations.
Conclusions:
After
a 5-year follow-up of this COPD population with comorbidities, a statistically
significant increase in AHT, depression, and anxiety was detected. 3.03% of
patients were diagnosed with abdominal aortic aneurism. There was 13.24%
mortality after 5 years. There was a significant correlation between the
severity of COPD and a COTE Index ≥ 4, but neither of these variables
correlated with mortality. Our main limitation was the small cohort included in
this study.
Key
word: Pulmonary
Disease, Chronic Obstructive; Indicators of Morbidity and Mortalit
RESUMEN
Objetivos:
Evaluar
la evolución de las comorbilidades en una cohorte de pacientes EPOC
durante 5 años de seguimiento. Evaluar la mortalidad. Valorar y
correlacionar la gravedad de la EPOC, el índice de COTE y la mortalidad.
Material
y Métodos: Estudio
prospectivo observacional en una cohorte de pacientes EPOC durante 2015-2020,
en el Servicio de Neumonología Hospital Privado Universitario de
Córdoba. Información de Historias Clínicas
electrónicas. Para predecir riesgo de mortalidad se utilizó el
índice de COTE. Análisis estadístico: prueba exacta de
Fisher, Prueba t de Student e InfoStat.
Resultados:
Sesenta
y ocho pacientes, masculinos 37 (54,41%), edad 75 Âą 6,69. Sin seguimiento: 2
pacientes. En el momento del ingreso, el tiempo del diagnóstico de EPOC
fue de 13,23 Âą 5,88 años. Más del 50% tenían EPOC
moderado. Sin diferencias en VEF1/post-BD (0,57 en 2015 vs. 0,58 en 2020), ni
en frecuencia de exacerbaciones en último año (1,06 Âą 1,26 vs.
0,85 Âą 1,44). En 2015, el 29,41% (n 20) eran TBQ actiÂvos y se redujo al 18,18%
(n 12). En 2015, recibían CI el 73,53% (n 50) y en 2020 el 56,92% (n 37)
(p 0,047). En 2015, un 4,41% (n 3) recibían esteroides sistémicos
y se incrementó al 20% (n 13) en 2020 (p 0,007). Sin diferencias
significativas en frecuencia de internaciones (0,13 Âą 0,38 vs. 0,97 Âą 2,34).
índice de COTE ≥ 4, no se modificó sigÂnificativamente a
los 5 años: el 23,53% (n 16) vs. el 29,41% (n 20). Se detectó en
2020, un incremento de HTA (el 66%, n 45 vs. el 77%, p 0,181), depresión
(el 19,12%, n 13 vs. el 30,30%, n 20, p 0,161) y ansiedad (el 22,06%, n 15 vs.
el 32%, n 21, p 0,243). En 2020, diagnóstico de aneurisma de aorta
abdominal en el 3,03% (n 2). Reducción de obesidad en el 25% (n 17) al
19,70% (n 13). En el seguimiento, fallecieron 9 pacientes (13,24%) y
tenían menos comorbilidades (p < 0,009). Mayor mortalidad en
pacientes con índice de COTE ≥ 4 (p 0,429). Los fallecidos
tenían mayor gravedad de la EPOC, con menor VEF1/post-BD a 5 años
(p 0,102). Aquellos con enfermedad cardiovascular o metabólica, a los 5
años, tenían menor proporción de fallecimiento (p <
0,05). Si bien los pacientes con índice de COTE en 2015 ≥ 4
presentaban menor promedio de VEF1/ post-BD al comienzo y en seguimiento a 5
años, la diferencia no fue significativa. Se observó que el
índice de COTE aumentaba en pacientes EPOC con VEF1/post-BD de grado
moderado y grave (p < 0,05).
Discusión:
Las
comorbilidades de la EPOC constituyen un factor pronóstico con efecto
acumulativo en morbimortalidad; por ello, la importancia de este estudio. Una
limitaÂción es la reducida población, que podría explicar
que no se observó correlación entre mortalidad y aumento de
comorbilidades. Destacamos el sobreuso de CI y esteroides sistémicos en
esta población, a pesar de no tener incremento de exacerbaciones ni internaciones.
Conclusiones:
En 5
años de seguimiento de esta población EPOC con comorbilidades, se
detectó un incremento de la HTA, depresión y ansiedad
estadísticamente signifiÂcativos. En un 3,03%, se diagnosticó
aneurisma de aorta abdominal. La mortalidad a los 5 años fue del 13,24%.
Hubo una correlación significativa entre la gravedad de la EPOC y el
índice de COTE ≥ 4, pero ninguna de estas variables se
correlacionó con la mortalidad. Nuestra principal limitación fue
la reducida cohorte incluida.
Received: 11/04/2022
Accepted: 05/02/2023
INTRODUCTION
Chronic
obstructive pulmonary disease (COPD) is a complex, multi-component,
heterogeneous disease with clinical, functional, and radiological
manifestations that vary significantly from paÂtient to patient, despite having
a similar airflow obstruction.1
The
associated comorbidities can be causally related, with smoking as a common risk
factor (ischemic heart disease or lung cancer), secondary to a complication of
COPD (pulmonary arterial hypertension or heart failure), or they can be asÂsociated
with advanced age (such as AHT, diabetes mellitus).2,3
It
is important to highlight that the symptoms of comorbidities can be similar to
those of COPD and may be underestimated, for example, dyspnea in heart failure
and lung cancer, or depression, which causes fatigue and reduces physical
activity.3
Comorbidities
are a prognostic factor with a cumulative effect on mortality. The MultidimenÂsional
COTE Index, which complements the well-accepted BODE Index (body-mass index,
airflow obstruction, dyspnea, and exercise capacity), is a predictor of
mortality risk that could be used to quantify the burden of comorbidities in
both cliniÂcal and research settings.4, 5, 6
The
relationship between COPD and the comorÂbidities is not fully understood.
However, a connecÂtion has been suggested through the inflammatory pathway,
given the persistent low-grade inflamÂmation, both pulmonary and systemic,
which are known risk factors for cardiovascular disease and lung cancer and are
present in COPD, regardless of the smoking status.7
Comorbidities
are common across all severities of COPD. Despite the negative impact of
multiple comorbidities in COPD, COPD itself is one of the most important
comorbid conditions that adÂversely affect the course of other diseases, such
as heart failure in hospitalized patients or coronary revascularization
surgery, leading to increased morbidity and mortality when COPD is present.3
In
the population-based PLATINO study, which examined the prevalence of COPD in
five cities in Latin America, it was concluded that in an unselected
population, individuals with COPD have more comorbidities. Age, female gender,
and higher body mass index (BMI) were identified as the main factors associated
with comorbidities in these patients with COPD.8
In
recent years, there has been an increased interest in understanding the
influence of comorÂbidities in COPD patients, with the ultimate goal of
reducing morbidity and mortality.2
There
is indeed sufficient evidence that comorÂbidities in COPD not only contribute
to increase symptoms, impair exercise capacity, and reduce quality of life with
a high economic burden of the disease but also serve as a prognostic factor
with a cumulative effect on mortality. For this reason, it was considered
important to conduct a follow-up on this population to assess their evolution.
OBJECTIVES
1.
To evaluate the progression of comorbidities in a cohort of COPD patients after
5 years of follow-up at the Pulmonology Service of the Hospital Privado
Universitario de Córdoba.
2.
To evaluate the mortality rate in a group of patients.
3.
To assess and correlate the severity of COPD with the COTE Index, and both of
them with the mortality.
MATERIALS AND METHODS
1)
Patients and data collection
Prospective
observational study that evaluated a cohort of patients diagnosed with COPD
during 2015-2020 who were attended at the Pulmonology Service of the Hospital
Privado Universitario de Córdoba.
We
considered the COPD definition provided by the GOLD 2021 (Global
Initiative for Chronic Obstructive Pulmonary Disease): âcommon, preventable
and treatable disease that is characterized by persistent respiratory sympÂtoms
and airflow limitation that is due to airway and/or alÂveolar abnormalities
usually caused by significant exposure to noxious particles or gases and
influenced by host factors including abnormal lung development. Significant
comorÂbidities may have an impact on morbidity and mortality.â
The
spirometric criterion for diagnosing COPD accorÂding to the GOLD 2021 is based
on a âpost-bronchodilator forced expiratory volume in one second (FEV1)/ forced vital capacity (FVC) ratio of less than 0.7.â
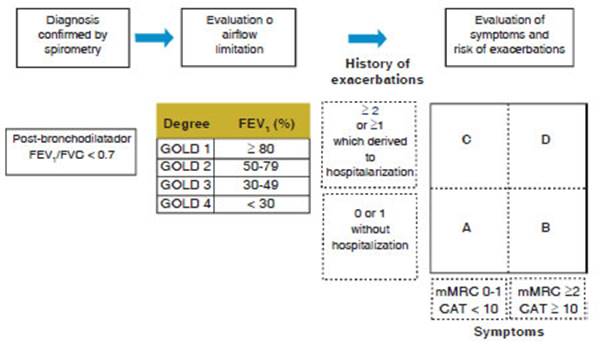
The
GOLD 2017 classification was considered for the analysis of the severity of
COPD. (Figure 1)
According
to the World Health Organization (WHO), âcomorbidityâ is defined as the
simultaneous occurrence of two or more diseases in the same person. This
definition aligns with what was published by Feinstein A. in 1970.
The
information was obtained from the electronic medical records of COPD patients.
Data collection was performed using an ad-hoc spreadsheet, which included the
following information:
âĒ Patient information
(age, sex, weight, height, BMI)
âĒ Spirometric data
âĒ Smoking habits
(current smoker, former smoker, smokÂing load determined by the âpack-yearsâ)
âĒ Status of respiratory
condition (years since diagnosis, degree of severity, number of exacerbations
and hosÂpitalizations in the past 12 months, current medical treatment)
âĒ Known comorbidities
documented in the latest pulmoÂnary medical check-up. The following were
included:
âĒ Cardiovascular
diseases (CVDs): AHT, heart failure (HF), ischemic heart disease (IHD), atrial
fibrillation (AF), peripheral vascular disease (PVD), pulmonary hypertension
(PHT), valvular heart disease, abdomiÂnal aortic aneurysm (AAA).
âĒ Metabolic diseases:
diabetes mellitus (DM), obesity, dyslipidemia (DL), hyperuricemia,
hypothyroidism, malnutrition.
âĒ Digestive diseases:
gastroesophageal reflux disease (GERD), gastric or duodenal ulcer, liver
cirrhosis, gastritis.
âĒ Musculoskeletal
diseases: osteoporosis, osteoarthritis, sarcopenia.
âĒ Psychiatric
disorders: depression, anxiety, sleep disÂorders.
âĒ Oncological diseases:
lung cancer, esophageal cancer, stomach cancer, pancreatic cancer, colon
cancer, prosÂtate cancer, breast cancer.
âĒ Other diseases:
ophthalmologic, hematologic, anomaÂlies of the kidney and urinary tract, and
other pulÂmonary conditions.
âĒ Deceased patients
âĒ COTE Index
In
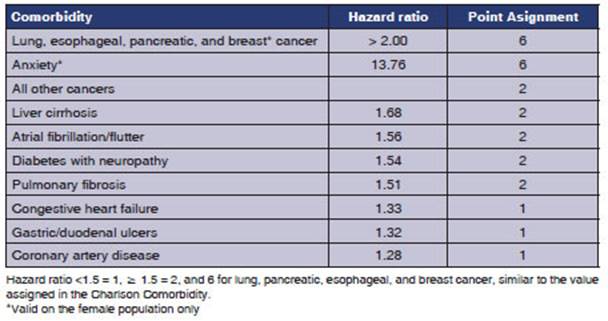
order to predict the mortality risk at 5 years, we used the Multidimensional
COTE Index, which consists of the most common comorbidities in patients with
COPD. A total score of 24 points indicates that the higher the score the
greater the number of comorbidities that predict mortality in COPD.4, 5, 6
An
increase in the COTE Index was associated with a higÂher risk of COPD-related
death (hazard ratio [HR], 1.13; 95% confidence interval, 1.08-1.18; P, 0.001)
as well as non-COPD-related causes of death (HR, 1.18; 95% confidence interval,
1.15-1.21; P, 0.001). Additionally, the increase in this index was
independently associated with an increased risk of death.4-6
A
COTE score greater than or equal to 4 points increaÂsed the risk of death by
2.2 times (HR, 2.26-2.68; P, 0.001). (Table 1) 4-6
2) Statistical analysis
A
descriptive analysis of the recorded variables was conducÂted. To relate the
number and type of comorbidities to the degree of severity of COPD, a
multivariate correspondence analysis was carried out. The statistical analysis
was conÂducted using the InfoStat 2014e program. A value of p < 0.05 was
considered to be significant.
For
inferential statistics, the Fisherâs exact test was used for studying the
relationship between categorical variables in 2x2 tables.
To
analyze the difference between quantitative variables, the Studentâs t test was
used for independent samples with one-tailed significance, and the
nonparametric Mann- Whitney U test and the Kruskal-Wallis test were used in
cases where the normal distribution of variables could not be assumed.
Lastly,
the SPSS for Windows v.22 was used for statisÂtical analyses, and the usual
significance level of 0.05 was applied in all cases.
RESULTS
68
patients were included, 37 male (54.41%), age 75Âą6.69. Two patients were lost
to follow-up durÂing the 5-year period.
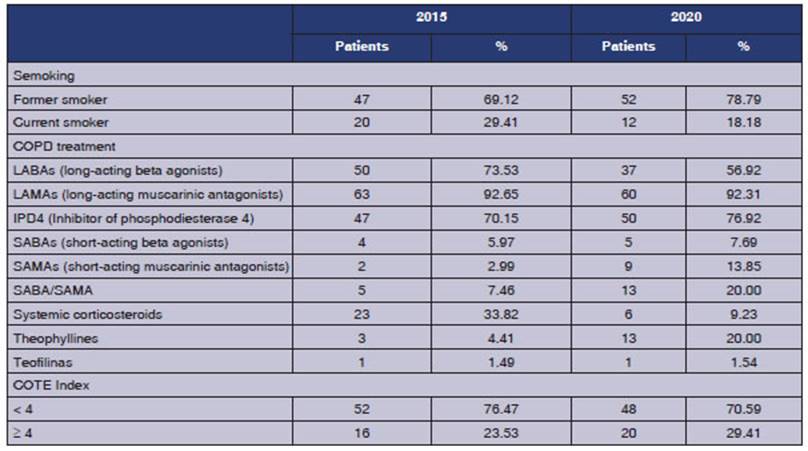
As
shown in Table 2, at the study entry, the time elapsed since the COPD diagnosis
of the entire population was 13.23 Âą 5.88 years. Regarding the post-BD FEV1, there were no
differences after 5 years (mean of 0.57 in 2015 vs. 0.58 in 2020). Furthermore,
in relation to exacerbations in the last year, there were no significant
differences during the 5-year follow-up (1.06 Âą 1.26 vs. 0.85 Âą 1.44). There
werenât any differences, either, in the frequency of hospitalizations in the
last year (0.13 Âą 0.38 vs. 0.97 Âą 2.34).
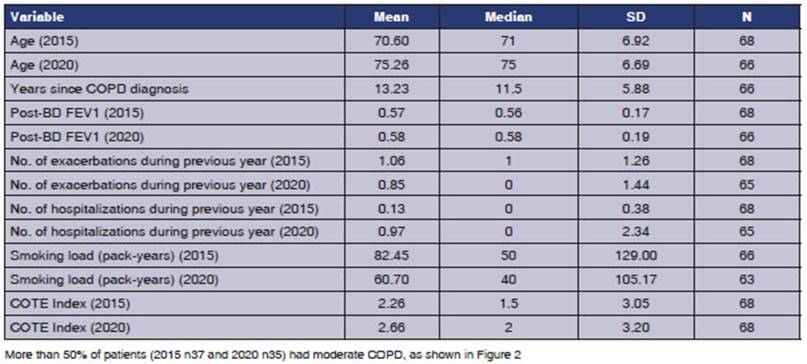
In
2015, 29.41% (n20) of the patients were acÂtive smokers, and this percentage
was reduced to 18.18% (n12) due to smoking cessation after 5 years (p 0.157),
as observed in Table 2.
Regarding
the treatment, in 2015, 73.53% (n50) of patients were receiving inhaled
corticosteroids (ICS), and after 5 years, this percentage decreased to 56.92%
(n37) (p 0.047). Only 7.5% (n5) received LABAs (long-acting beta agonists) at
study entry, and this percentage did not change during the subsequent follow-up
period. It was also observed that in 2015, 4.41% (n3) of patients were
receiving systemic steroids, and this percentage increased to population was 13.23 Âą 5.88 years. Regarding the post-BD
FEV1, there were no
differences after 5 years (mean of 0.57 in 2015 vs. 0.58 in 2020). Furthermore,
in relation to exacerbations in the last year, there were no significant
differences during the 5-year follow-up (1.06 Âą 1.26 vs. 0.85 Âą 1.44). There
werenât any differences, either, in the frequency of hospitalizations in the
last year (0.13 Âą 0.38 vs. 0.97 Âą 2.34).
In 2015, 29.41% (n20) of the patients were acÂtive smokers, and
this percentage was reduced to 18.18% (n12) due to smoking cessation after 5
years (p 0.157), as observed in Table 2.
Regarding the treatment, in 2015, 73.53% (n50) of patients were
receiving inhaled corticosteroids (ICS), and after 5 years, this percentage
decreased to 56.92% (n37) (p 0.047). Only 7.5% (n5) received LABAs (long-acting
beta agonists) at study entry, and this percentage did not change during the
subsequent follow-up period. It was also observed that in 2015, 4.41% (n3) of
patients were receiving systemic steroids, and this percentage increased to 20%
(n13) after 5 years. The cause of this change was not specified in the medical
record (p 0.007). The COTE Index, with a cutoff point of ≥4, did not show
statistically significant changes over the 5-year follow-up period: 23.53%
(n16) vs. 29.41% (n20) (Table 2).
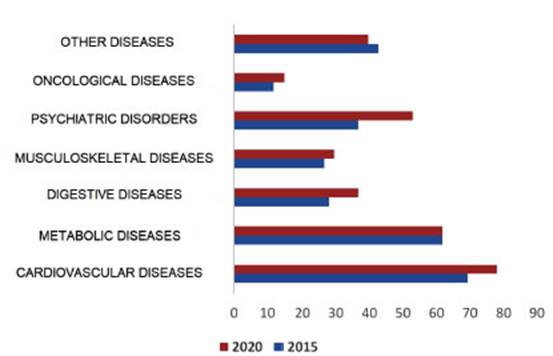
Regarding comorbidities, over the 5-year follow-up period, an
increase in the diagnosis of hypertenÂsion (AHT) was detected (66% n45 vs. 77%
n51, p 0.181). There were 2 cases of abdominal aortic aneurysm (AAA) in 2020
(3.03%), and increase in depression (19.12% n13 vs. 30.30% n20, p 0.161) and
anxiety (22.06% n15 vs 32% n21, p 0.243). Regarding obesity, a reduction was
detected from 25% (n17) to 19.70% (n13).
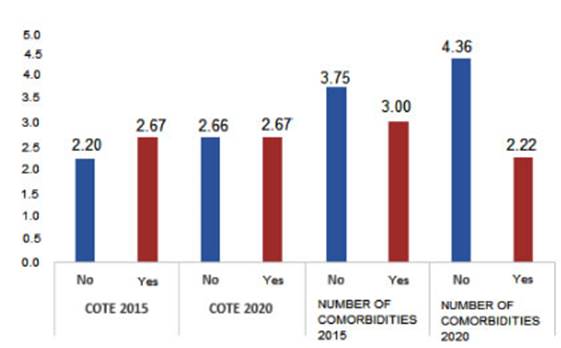
During the 5-year follow-up, 9 patients (13.24%) died. After the
5-year period, it was observed that this group had fewer comorbidities, with
statistiÂcal significance (p < 0.009), as shown in Figure N 3. There was a
higher mortality rate in patients with a COTE index ≥4, but it was not
statistically significant (p 0.429). The patients who died showed a lower
post-BD FEV1 at 5 years, but the difference between the groups was not
statistically significant (p 0.102). Although the difference wasnât statistiÂcally
significant, it was observed that increased severity of COPD was associated
with a higher mortality rate. Patients with cardiovascular or metabolic disease
had a lower rate of deaths at 5 years, and the relationship between these
variables is statistically significant (p < 0.05).
2) Statistical analysis
A
descriptive analysis of the recorded variables was conducÂted. To relate the
number and type of comorbidities to the degree of severity of COPD, a
multivariate correspondence analysis was carried out. The statistical analysis
was conÂducted using the InfoStat 2014e program. A value of p < 0.05 was
considered to be significant.
For
inferential statistics, the Fisherâs exact test was used for studying the
relationship between categorical variables in 2x2 tables.
To
analyze the difference between quantitative variables, the Studentâs t test was
used for independent samples with one-tailed significance, and the
nonparametric Mann- Whitney U test and the Kruskal-Wallis test were used in
cases where the normal distribution of variables could not be assumed.
Lastly,
the SPSS for Windows v.22 was used for statisÂtical analyses, and the usual
significance level of 0.05 was applied in all cases.
RESULTS
68
patients were included, 37 male (54.41%), age 75Âą6.69. Two patients were lost
to follow-up durÂing the 5-year period.
As
shown in Table 2, at the study entry, the time elapsed since the COPD diagnosis
of the entire population was 13.23 Âą 5.88 years. Regarding the post-BD FEV1, there were no
differences after 5 years (mean of 0.57 in 2015 vs. 0.58 in 2020). Furthermore,
in relation to exacerbations in the last year, there were no significant
differences during the 5-year follow-up (1.06 Âą 1.26 vs. 0.85 Âą 1.44). There
werenât any differences, either, in the frequency of hospitalizations in the
last year (0.13 Âą 0.38 vs. 0.97 Âą 2.34).
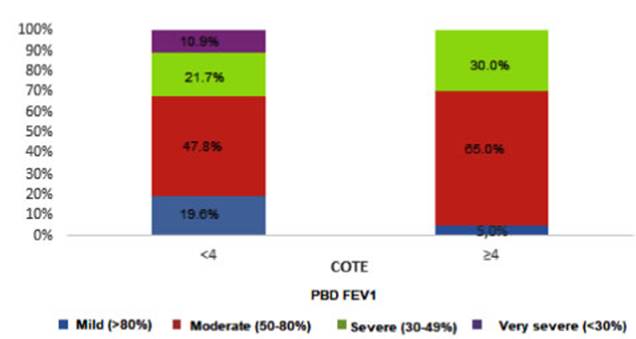
Although patients with a COTE Index ≥4 in 2015 had a lower
mean post-BD FEV1 at baseÂline and at 5-year follow-up, the difference beÂtween
the groups wasnât statistically significant (p>0.05). It was observed that
the COTE Index increases in patients with COPD with post-BD FEV1 of moderate
and severe degree, and the difference is statistically significant (p<
0.05), as shown in Figure 5.
DISCUSSION
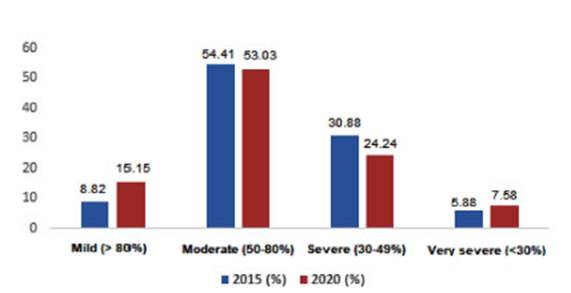
The importance of this study was the follow-up of patients with
COPD and comorbidities over a period of 5 years. In our population, more than
50% of all COPD patients were classified as modÂerate, similar to what was
observed in the EPOC AR study (52%).
With regard to the treatment, it is concerning that the use of
systemic steroids increased durÂing the follow-up period, despite the fact that
no increase in exacerbations was observed in the study group. However, the use
of ICS decreased after 5 years (73.53% vs. 56.92%), and one possible
explanation could be that the guidelines are being followed. On the other hand,
it is noteworthy that 7.35% of patients were not receiving LABAs, and that this
medication wasnât subsequently incorpoÂrated into their treatment.
There is no doubt that comorbidities have an impact on the overall
health status, the use of healthcare resources, hospitalizations, and morÂtality
of patients with COPD. In fact, while the most common cause of death in COPD
patients with advanced disease is respiratory in origin, in individuals with
mild to moderate COPD, mortalÂity is associated with cardiovascular
comorbidities and lung cancer.8
In the PLATINO study, the reported comorÂbidities were (in
decreasing order of frequency): any cardiovascular disease (41.5%),
hypertension (37.2%), peptic ulcer disease (31.8%), asthma (22.8%), heart
disease (13.7%), diabetes (8.4%), stroke (3.2%), and lung cancer (1.1%). These
results align with studies indicating that cardioÂvascular problems are among
the most common comorbid conditions in COPD.6 After the 5-year follow-up, we
detected in our population a non-significant increase in AHT (66% vs. 77%),
depresÂsion (19.12% vs. 30.30%), and anxiety (22.06% vs. 32%), and we also
observed the occurrence of AAA in 2020 (3.03%).
The curvilinear relationship between comorÂbidity score and BMI
observed in the group of COPD individuals allows us to speculate about the
adverse effect of underweight in these patients (unhealthy underweight).8
In the study group, it was observed that obesity decreased during the 5-year
follow-up (25% vs. 19.70%), which could be a factor associated with a poor
prognosis.
Divo et al mention a higher risk of death asÂsociated with the
presence of pulmonary fibrosis, peptic ulcer disease, and liver cirrhosis, but
no increased risk of atrial fibrillation (AF) was obÂserved. These findings
raise the possibility of a close interaction between these diseases, which may
share common biological pathways.4-6
Although hypertension, hyperlipidemia, and obstructive sleep apnea
are highly prevalent, the direct risk of death attributable to these conditions
is not significant. They propose that the most likely reason is that all these
conditions are treatable or not significant risk factors for the development of
more lethal diseases, such as coronary artery disease. While neoplasms in
general confer a sigÂnificant risk of death, lung cancer is the one that most
frequently shows an aggregated prevalence of 9%. One striking finding they
encountered was the relatively high prevalence of interstitial pulÂmonary
fibrosis (6%) and its strong independent association with the risk of death.4-6
Liver cirrhosis and anxiety were also associÂated with a higher
risk of death, suggesting certain correlation with the lifestyle and social
behavior of this population. The mechanisms by which anxiety was identified as
a risk factor for mortality in COPD patients, particularly in feÂmales, are
still unknown. However, it was found that anxiety has an impact on the rate of
exacÂerbations and hospitalizations. We observed an increase in anxiety, though
it wasnât statistically significant. The risk of by peptic ulcer disease is
very interesting in view of the findings reported by researchers of the ECLIPSE1
study, where one of the predictors of frequent exacerbations in COPD was the
presence of gastroesophageal reflux.4-6
At the 5-year follow-up, 9 patients (13.24%) died. Unlike what has
been observed in other studies, the deceased patients in this series had fewer
comorbidities (p < 0.009). However, the mortality rate was higher, though
not statistically significant, in patients with a COTE index ≥ 4 and a
higher degree of obstruction as evaluated by FEV1. In contrast to what has been
published in the literature, we observed that patients with cardiovascular or
metabolic disease had a lower proportion of mortality after 5 years (p <
0.05). Although the difference wasnât statistically sigÂnificant, it was
observed that increased severity of COPD was associated with a higher mortality
rate.
As observed in other studies, patients with a COTE Index ≥ 4
in 2015 had a lower mean post-bronchodilator FEV1 at baseline and at the 5-year
follow-up, but this finding did not reach statistical significance (p>0.05).
One of the main limitations of this study is the small population
size, which could explain the lack of correlation between mortality and
increased comorbidities.
CONCLUSIONS
In the 5-year follow-up, there was an increase in AHT, depression,
and anxiety, but these changes were not statistically significant. A total of
3.03% of the population was diagnosed with AAA by the end of the study.
The overall mortality rate at the end of the study was 13.24%.
There was a statistically significant correlation between the
severity of COPD and a COTE Index ≥ 4, but neither of these variables
correlated with mortality.
Our main limitation was the small cohort inÂcluded in this study.
REFERENCES
1. Agusti A, Calverley PM, Celli B, et al. Characterisation of
COPD heterogeneity in the ECLIPSE cohort. Respir Res. 2010;11:122.
https://doi.org/10.1186/1465-9921-11-122
2. de Miguel Díez J, García TG, Maestu LP.
Comorbilidades de la EPOC. Arch Bronconeumol. 2010 Dec;46 Suppl 11:20-5.
https://doi.org/10.1016/S0300-2896(10)70058-2
3. https://goldcopd.org 2021
4. Divo M, Cote C, de Torres JP, Casanova C, et al. Comorbidities
and risk of mortality in patients with chronic obstructive pulÂmonary disease.
Am J Respir Crit Care Med. 2012;186:155- 61.
https://doi.org/10.1164/rccm.201201-0034OC
5. Jimenez JJ Sívori M. Comparación de los
índices de Charlson y COTE en la enfermedad pulmonar obstructiva
crónica (EPOC) y su relación con la mortalidad. Rev Am Med Resp 2022;1:3-9.
6. Stolz D, Louis R, Boersma W, et al. COPD-specific coÂmorbidity
test (COTE) for predicting mortality in COPD â Results of an European,
multicenter study. Eur Respir J. 2014;44:P566.
7. Sin DD, Anthonisen NR, Soriano JB, Agusti AG. Mortality in
COPD: Role of comorbidities. Eur Respir J. 2006;28:1245-
57. https://doi.org/10.1183/09031936.00133805
8. López Varela MV, Montes de Oca, Halbert R, Muiño
A, Tálamo C, Pérez-Padilla R, el al. Comorbilidades y estado de
salud en individuos con y sin EPOC en 5 ciudades de América Latina:
Estudio PLATINO. Arch BronÂconeumol. 2013; 49:468â74.
https://doi.org/10.1016/j.arbres.2013.05.003
9. Echazarreta AL, Arias SJ, Del Olmo R, et al. Prevalence of COPD
in 6 Urban Clusters in Argentina: The EPOC. AR Study.
Arch Bronconeumol (Engl Ed). 2018;54:260-9.
https://doi.org/10.1016/j.arbr.2017.09.017