Autor : Walter Mattarucco1
1Pulmonologist. Vice-president of the AAMR (Argentinian Association of Respiratory Medicine)
Despite
substantial advances in reducing the imÂpact of many non-communicable diseases
(such as heart disease and cancer), the morbidity and mortality of chronic
respiratory disease continue to rise. This increase is mainly due to the
growing burden of chronic obstructive pulmonary disease (COPD), which has
occurred despite the fact that smoking was identified as the leading risk
factor for the disease over 50 years ago. Many factors have contributed to what
must now be considered a public health emergency: failure to limit the sale and
consumption of tobacco products, and lack of control over lifelong exposure to
environmental pollutants, in addition to the aging of the global population.1 In the
introduction of this document, The Lancet Commission acknowledges that this is
the start of a debate and that not all actions can be implemented basing on
evidence or be applied equitably in different parts of the world.
In
the year 2020, Argentina recorded 376,219 deaths from all causes, with
respiratory diseases ranking third (14.5%), though in a lower proporÂtion
compared to the previous year (18%). This decrease was due to the emergence of
SARS-CoV-2 (14.1%) as a cause of death, which ranked fourth.2
This clearly demonstrates that COPD and its conÂsequences
continue to increase steadily.
The
EPOC.AR study showed that in our country, the prevalence of this condition
reaches 14.5%, with an observed underdiagnosis that reached 77%.3
Similar to other countries, the lack of detecÂtion of COPD
remains a problem for healthcare systems. There are multiple reasons for this
lack of detection: first, smoking patients with symptoms often attribute them
to their smoking habit, age, or deconditioning. Secondly, these symptoms are
not routinely investigated during consultations when compared, for example, to
blood pressure or glucose control. Thirdly, brief intervention for smoking
cessation (which has proven effectiveÂness) is not provided consistently.
Fourthly, the spirometry is not a widely or equitably available test in our
healthcare system, and its availability in the private sector is often
restricted in terms of frequency.
In
recent years, the GOLD initiative has emphaÂsized several issues related to
etiology, taking into account other exposures such as the use of biomass and
illicit drugs as causes of COPD. However, the requirement of a FEV1/FVC ratio
< 0.70 is still necessary to confirm the diagnosis.4
In
recent years, Alvar Agusti et al have been advocating for the holistic approach
to COPD through GETomics.5 The acronym GET
stands for gene, environment, and time, describing the possible relationship
between a person’s genetic burden associated with exposure/events throughÂout
their lifetime, and the timing in which it is expressed or acts. These events
are associated with various “omics”, which are sets of features within a
specific sphere (clinical, radiological, genetic, imaging, or structural).
This
is a comprehensive approach of biological events occurring in a specific
individual, who is subjected to etiological environmental factors. With this
integrated strategy, through the indiÂvidual patient’s history, we can
establish the presÂence of life events (such as low birth weight, preÂmaturity,
childhood infections, childhood asthma, tuberculosis) that become determinants
of what we call the “pulmonary function trajectory.” This traÂjectory expresses
the unnatural evolution of our pulmonary function; it determines the alteration
in the FEV1 value at different moments in life (at birth, during adolescence,
in adulthood) which may go unnoticed and, if subjected to various types of
exposure (smoking, biomass smoke, toxic fumes, inhalation of heated nicotine
products) it increases the likelihood of developing COPD.
From
a practical perspective, in the clinic, we find patients with all the symptoms
of COPD who never smoked, patients with risk factors and strucÂtural
abnormalities in their imaging but without symptoms, and young adult smokers
who were asthmatic and suffered from bronchiolitis at an early age. Some will
have functional impairment, while others won’t. The latter fall into what GOLD
refers to as early COPD.
At
present, we lack evidence that supports active searching for at-risk
individuals or undiagnosed COPD patients. And healthcare systems neither
support nor promote an active search of cases, and this initiative is limited
to individual action within a system that does not encourage multidisÂciplinary
work.
In
this issue of RAMR, Uribe Echevarría et al present a multidisciplinary
and integrated strategy for the “Prevention, Diagnosis, and Management of Pre-COPD.”
6 Based on The Lancet CommisÂsion’s initiative, it not only covers
diagnosis but also prevention and early detection. How does this group propose
to undertake this colossal task? Firstly, clear and precise objectives: to
emphasize the existence of situations that facilitate the alteraÂtion of the
pulmonary function trajectory, to inform the population about the risks, and
encourage the search for undiagnosed individuals, provide inforÂmation about
the types of exposure that predispose the development of COPD, conduct imaging
and functional studies in symptomatic patients or paÂtients with compatible
medical history.
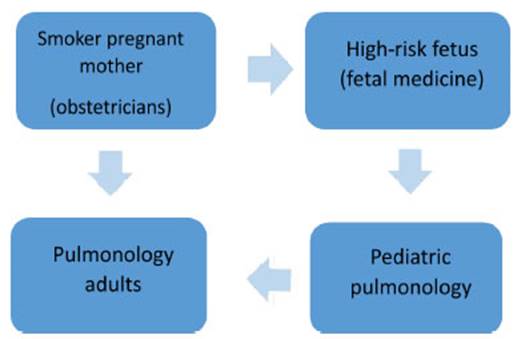
The
group proposes active searching from birth to adulthood for life situations
combined with alÂterations in pulmonary function or structure that can lead to
the development of COPD.
Clearly,
this initiative falls within the realm of precision medicine, in a manner
consistent with current trends. It promotes interdisciplinary work and the
involvement of multiple specialties, with a clear objective: to eliminate COPD.
However, it also faces some obstacles, such as obtaining the commitment of all
the disciplines involved, securing economic and logistical resources, and
sustaining the initiative over time.
I
have no doubt that they will succeed. Lastly, it is worth acknowledging that
actions like this should be imitated by all healthcare systems, both public and
private. Some of the described situaÂtions can be detected through simple
questioning, an easily accessible tool, and the first step in this set of
actions that lead us to fulfill our role in the elimination COPD.
REFERENCES
1.
Stolz D, Mkorombindo T, Schumann DM, Agusti A, Ash SY, Bafadhel M, et al.
Towards the elimination of chronic obstructive pulmonary disease: a Lancet
Commission Lancet 2022;400:921-72. https://doi.org/10.1016/S0140-6736(22)01273-9
2.
Fuente: elaborado por el SIVER-Ca sobre la base de los registros de mortalidad
de la DEIS, Ministerio de Salud de la Nación. Instituto Nacional del
Cáncer (INC), Argentina 2022.
3.
Echazarreta AL, Arias SJ, Del Olmo R, Giugno ER, ColodenÂco FD, Arce SC, et al.
Prevalencia de enfermedad pulmonar obstructiva crónica en 6 aglomerados
urbanos de Argentina: el estudio EPOC.AR. Arch Bronconeumol (Engl Ed). 2018;54:260-9. https://doi.org/10.1016/j.arbres.2017.09.018
4.
Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the
Diagnosis, Management, and PreÂvention of Chronic Obstructive Pulmonary Disease
(2023 Report). 2022.
5.
Agustí A, Melén E, DeMeo DL, Breyer-Kohansal R, Faner R.
Pathogenesis of chronic obstructive pulmonary disease: unÂderstanding the
contributions of gene-environment interactions across the lifespan. Lancet
Respir Med. 2022;10:512- 24.
https://doi.org/10.1016/S2213-2600(21)00555-5.
6.
Uribe Echevarría L, Bertolin AV, Hidalgo G, Arato G, Aguilera J,
Álvarez R, et al. Implementation of a COPD Eradication Program
Multidisciplinary Program for PreÂvention, Diagnosis, and Management of
Pre-COPD. Rev Am Med Resp 2023;23:84-88.
https://doi.org/10.56538/ramr.SLAR8378