Autor :DomĂnguez-Zabaleta, Irene Milagros1, Benedetti, Paola1, Ramos, Alicia Oliva, Maestu, Luis Puente, GarcĂa LĂłpez, JosĂ© Javier
1 Pulmonology Service. Hospital Gregorio Marañón. Madrid. Spain.
2 Thoracic Surgery. ClĂnica de Cuyo. Mendoza, Argentina.
3 Thoracic Surgery. Hospital Santa Isabel de HungrĂa, Mendoza, Argentina.
4Thoracic Surgery. ClĂnica Santa MarĂa, Mendoza, Argentina.
Correspondencia : Irene Milagros DomĂnguez- Zabaleta E-mail: iremidoza@hotmail.com
ABSTRACT
The
endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is
a safe, minimally invasive technique used for the diagnosis of mediastinal and
hilar adenopathy, especially lung cancer. Even though complications are rare
(around 1%), they may include severe bleeding, pneumomediastinum and
tracheomediastinal fistulas. We present the case of a patient with lung
adenocarcinoma diagnosed through EBUS-TBNA who developed a fistula between the
trachea and the tumor after the procedure. No previously described cases were
found in the consulted scientific literature, as the patient did not have the
main risk factors for the development of this type of complicaÂtion. The
patient did not develop any subsequent infectious symptoms, possibly thanks to
the early use of antibiotic therapy.
Key
words: Fístula;
Tumor; Transbronchial needle aspiration; Endobronchial ultrasound
RESUMEN
La
punción con aguja transbronquial guiada por ultrasonido endobronquial
(EBUS-TBNA) es una técnica segura y mínimamente invasiva
utilizada para el diagnóstico de adenopatías mediastínicas
e hiliares, especialmente en el cáncer de pulmón. Aunque las
complicaciones son raras (alrededor del 1%), pueden incluir sangrado grave,
neumomediastino y fístulas traqueomediastínicas. Presentamos un
caso clínico de un paciente con adenocarcinoma de pulmón
diagnosticado mediante EBUS-TBNA, el cual desarrolló una fístula
entre tráquea y tumor tras la realización de la técnica,
no encontÂrando casos descritos previamente en la literatura científica
consultada al no presentar los principales factores de riesgo para el
desarrollo de este tipo de complicaciones. El paciente no desarrolló
clínica infecciosa posterior, posiblemente gracias al uso de
antibioterapia de forma precoz.
Palabras
clave: Fístula;
Tumor; Punción-aspiración con aguja transbronquial;
Ecografía endobronquial
Received: 09/27/2022
Accepted: 03/09/2023
INTRODUCTION
The
endobronchial ultrasound-guided transbronÂchial needle aspiration (EBUS-TBNA)
is a miniÂmally invasive diagnostic bronchoscopic technique performed with the
assistance of an ultrasound convex mini-probe at the tip of the bronchoscope.
It is used for the study of hilar and mediastinal adenopathy, being
particularly useful for staging lung cancer. It is a safe technique because
ultraÂsound allows for the recognition of pulmonary, pleural, and vascular
structures, resulting in a low complication rate, typically around 1%.1 Complications
are generally of minor severity and often resolve with conservative treatment.2 However,
within the spectrum of complications, there is a small percentage, estimated at
0.26%3, that
includes significant bleeding, pneumomediÂastinum, tracheomediastinal fistulas,
and their infectious complications. These complications can lead to prolonged
hospitalization and, in the case of lung cancer, a delay in the start of
oncological treatment.4
Clinical observation
Recently,
we attended a 54-year-old male patient with a significant history of tobacco
use (cumulaÂtive smoking index of 72 packs-years), who initially consulted the
Otorhinolaryngology Service due to dysphonia. During the fiberoptic
examination, right vocal cord paralysis was identified. For furÂther
investigation, a chest computed tomography (CT) was requested, revealing right
paratracheal and mediastinal adenopathies. The patient was then referred to a
pulmonology consultation to be assessed.
During
the initial consultation, the patient reÂported a 6-month history of dysphonia
associated with constitutional symptoms and unintentional weight loss of 20 kg
over the past 6 months, without any additional symptoms. Physical examination
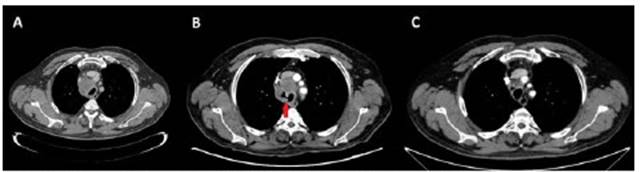
was unremarkable. The chest CT images were reÂviewed, showing conglomerate
lymph node masses in the right paratracheal region (4.8Ă—4.2Ă—5.5 cm in diameter)
and subcarinal region (1.5Ă—2.7Ă—5 cm in diameter) with certain suggestive signs
of necrosis. Additionally, a right hilar adenopathy (3.2Ă—2.7 cm) was observed
(Image 1).
A
bronchoscopy was performed, revealing muÂcosal thickening in the middle and
distal third of the trachea without clear signs of infiltration. Furthermore,
an EBUS-TBNA procedure was conÂducted in the right paratracheal station without
immediate complications. The histologic diagnosis was consistent with
metastasis from non-small cell lung cancer, although the sample was
insufficient to complete the immunohistochemical study.
Therefore,
a new EBUS-TBNA of the same station was performed three weeks later, without
immediate complications. This second procedure confirmed the final diagnosis of
metastatic lung adenocarcinoma, allowing for further relevant studies (EGFR
[epidermal growth factor receptor], ALK [anaplastic lymphoma kinase gene], ROS1
[c-ros oncogene 1], and PDL1 [programmed death ligand-1]).
Two
weeks later, upon completion of staging with PET-CT (positron emission
tomography - computed tomography), an incidental finding was observed,
indicating a contained rupture of the right tracheal wall with air leak towards
the right paratracheal tumor (Figure 1).
The
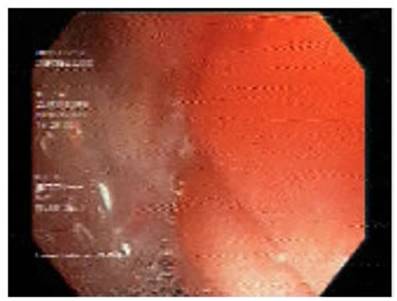
following week, a new diagnostic fiberopÂtic bronchoscopy was performed,
revealing grade III mucosal infiltration of the middle and distal third of the
trachea, along with a fistula in the middle third of the trachea, of
approximately 5 mm, surrounded by tumor tissue (Figure 2). The patient received
prophylactic treatment with oral amoxicillin-clavulanic acid for one week, and
no other complications developed during follow-up.
Given
the diagnosis of stage TĂ—N3M1 lung adenocarcinoma, the patient began
oncological treatment with chemotherapy. However, radiation therapy was not
included due to the high risk of mediastinitis associated with the tracheal
fistula.
DISCUSSION
EBUS-TBNA
is a safe bronchoscopic technique for the study of hilar-mediastinal adenopathy
and staging of lung cancer.1-4
Despite
the fact that serious complications from this procedure account for a very low
percentage (0.26%) and represent exceptional cases,3
given the great usefulness and increasing number of procedures
performed with EBUS-TBNA, we must take it into account to minimize their
occurrence as much as possible.4
After
reviewing the available literature on seriÂous complications following
EBUS-TBNA related to the occurrence of fistulas, we have found a case of
bronchomediastinal fistula with development of pneumomediastinum following the
EBUS-TBNA procedure after a mediastinoscopy5; a case of hemoptysis due to the development
of an aortopulmonary fistula following EBUS-TBNA in a patient who was
previously receiving antianÂgiogenic treatment with bevacizumab6; and even the development of a
tracheomediastinal fistula, without clinical consequences, following the initiaÂtion
of radiotherapy in a patient who had recently undergone EBUS-TBNA3.
However, we have not found any description of tumor fistulization into the
trachea following the EBUS-TBNA procedure, as in the case we present.
Furthermore, this is a patient without apparent risk factors, as he had not
previously undergone any mediastinoscopy or received antiangiogenic treatment
(bevacizumab), or radiotherapy, which also differentiates him from the rest of
the cases of the consulted literature. Although the possible presence of
necrosis in the conglomerate lymph node masses could have been a risk factor in
our patient’s case.
Currently,
there is no clear evidence of the efficaÂcy of the use of prophylactic
antibiotics to prevent infectious complications following EBUS-TBNA.7 However, our
case would support the thesis of Jang et al, who already described that
prophylactic antibiotic therapy should be considered in cases of cystic or
necrotic lesions, with the intention of covering the most common microorganisms
in the oral cavity and preventing the development of infectious complications.4
In
conclusion, we present a case that shows the development of a fistula between
the trachea and tumor following the EBUS-TBNA procedure, not previously
described in the consulted scientific literature, as it does not have the main
risk factors for the development of fistulous complications nor subsequent
infectious symptoms, possibly due to the early use of antibiotic therapy.
Conflict
of interest
The
authors have no conflict of interest to declare that are relevant to the
presented case.
REFERENCES
1.
Asano F, Aoe M, Ohsaki Y, et al. Complications associated with endobronchial
ultrasound-guided transbronchial needle aspiration: a nationwide survey by the
Japan Society for Respiratory Endoscopy. Respir Res. 2013;14:50.
https://doi.org/10.1186/1465-9921-14-50
2.
Eapen GA, Shah AM, Lei X, Jimenez CA, et al. American College of Chest
Physicians Quality Improvement Registry, Education, and Evaluation (AQuIRE)
Participants. Complications, consequences, and practice patterns of endobronÂchial
ultrasound-guided transbronchial needle aspiration: Results of the AQuIRE
registry. Chest. 2013;143:1044-53.
https://doi.org/10.1378/chest.12-0350
3.
Holty JE, Kuschner WG, Gould MK. Accuracy of transbronÂchial needle aspiration
for mediastinal staging of non-small cell lung cancer: a meta-analysis. Thorax.
2005;60:949-55.
https://doi.org/10.1136/thx.2005.041525
4.
Jang JG, Ahn JH, Lee SS. Delayed onset of mediastinitis with tracheomediastinal
fistula following endobronchial ultrasound-guided transbronchial needle
aspiration; A case report. Thorac Cancer. 2021;12:1134-6.
https://doi.org/10.1111/1759-7714.13888
5.
Bougioukas I, Seipelt R, Huwer H. Bronchial Fistula and Pneumomediastinum after
EBUS-TBNA Following MediÂastinoscopy. Thorac Cardiovasc Surg Rep. 2019;8:e11-e13. https://doi.org/10.1055/s-0039-1688476
6.
Wong J, Gutierrez C, Shannon VR, Eapen GA, Faiz SA. Bronchomediastinal Fistula
after Endobronchial Ultrasound-guided Transbronchial Needle Aspiration. Am J
Respir Crit Care Med. 2016;194:114-5. https://doi.org/10.1164/rccm.201601-0144IM
7.
Takagi H, Nagaoka T, Ando K, et al. Efficacy of antibiÂotic prophylaxis after
endobronchial ultrasound-guided transbronchial needle aspiration: a preliminary
prospecÂtive study. J Pulm Respir Med. 2017;7:416.
https://doi.org/10.4172/2161-105X.1000416