Autor : RodrĂguez-Sanz, Jorge1, GĂłmez-Miranda, Ricardo Ignacio2
1 Pulmonology Service, Hospital Universitario Miguel Servet 2Radiodiagnostic Service, Hospital Universitario Miguel Servet
https://doi.org./10.56538/ramr.BSJF4572
Correspondencia : Jorge RodrĂguez Sanz E-mail: jrsanz265@gmail.com
ABSTRACT
We present the case of a patient affected
by multiple myeloma refractory to various lines of treatment who was admitted
due to hemoptysis caused by the appearance of a plasmacytoma in the trachea.
The finding was obtained from a bronchoscopy, and the diagnosis and treatment
were made by means of endoscopic techniques, with a very good functional
result. This case is of interest because it is unusual and also because it
allows us to raise awareness among the community of this atypical presentation
and possible management.
Key word: Plasmacytoma; Hemoptysis; Bronchoscopy
RESUMEN
Presentamos el caso de un paciente afectado por un
mieloma múltiple refractario a diversas líneas de tratamiento,
que ingresó por hemoptisis causada por la aparición de un plasmocitoma en la tráquea. El hallazgo se produjo
por broncoscopia y el diagnósÂtico y
tratamiento se realizó mediante técnicas endoscópicas, con
muy buen resultado funcional. El caso es de interés por su escasa
frecuencia, así como para dar a conocer a la comunidad este tipo de
presentación atípica y su posible manejo.
Key words: Plasmacitoma; Hemoptisis; Broncoscopía
Received: 5/30/2022
Accepted: 8/18/2022
INTRODUCTION
Tracheal plasmacytomas are
unusual findings. In our case, the patient has multiple myeloma of poor
evolution with hemoptysis caused by the tracheal lesion. Due to the fact that
it is a high-risk patient, we decided to use minimally invasive endoscopic
techniques, and a good result was obtained without recurrence of blood
expectoration.
CASE REPORT
Patient diagnosed with multiple
myeloma, IgG kappa, stage IIIA, ISS (International Staging System) 2, who has
been receiving follow-up treatment by the Hematology Service of the HosÂpital
Universitario Miguel Servet since 2014. The patient showed torpid evolution
with eight lines of treatment, including autologous hematopoietic stem cell
transplant in 2015, with disease progresÂsion until today. The patient is
currently receiving treatment with daratumumab.
The patient went to the Emergency
Department due to hemoptysis and said that he/she had expectoÂrated red blood
and hadn’t had any previous episodes. He/she had a thrombocytopenia of 59,000
platelets per milliliter; chest X-ray without acute alterations. Due the acute
condition, he/she was admitted to the Pulmonology Department to be evaluated.
At the time of admission, the
patient was hemoÂdynamically stable, with blood-streaked sputum. He/she was
referred to the Otolaryngology Service for assessment: it reported normal
oropharynx without blood residue, normal cavum and normal hypopharynx and
vallecula. The epiglottis was free and without lesions, and the pyriform
sinuses were free and open. Finally, the vocal cords were free, mobile and
lesion-free. When the patient was asked to cough, a bloody mucus clot was
observed. No lesions or blood were observed at the upper level of the airway.
Due to the suspicion that blood
could be comÂing from the bronchial tree, a bronchoscopy was requested.
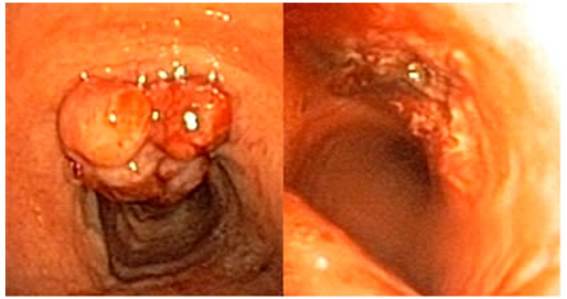
The bronchoscopy showed an
irregular papilliÂform nodule of exophytic growth in the anterior wall of the
trachea, two centimeters apart from the vocal cords, showing signs of recent
bleeding but without active bleeding at the time of the screening. Despite the
lesion, the trachea had a 70% free lumen.
Considering such findings and
taking into acÂcount that the patient had thrombocytopenia, a new bronchoscopy
was set for two days later, with biopsies and laser vaporization of the lesion.
When screening the patient’s
trachea, a clear increase in the size of the lesion was observed. The biÂopsy
was performed without significant findings, and samples were sent to the
hospital’s pathology laboraÂtory. After laser vaporization of the lesion, there
was 100% tracheal lumen, with good macroscopic result. The patient didn’t show
signs of extrinsic compresÂsion or dynamic collapse of the airway.
The final pathology report
characterized the leÂsion as plasmacytoma with diffuse plasma cell proÂliferation,
with restriction of the Kappa light chain.
A new positron emission
tomography was perÂformed six weeks after resecting the lesion. The tomography
showed multiple myeloma with signs of progression due to a lesion in the
anterior wall of the trachea. Pre-existing lytic lesions showed an increase in
the metabolic activity together with generalized hypermetabolism in the spinal
cord.

DISCUSSION
This case is interesting because
this type of tumor in the trachea is very rare,1, 2 and because
of the good results obtained with the endoscopic techÂniques that were used.
The tumors of plasma cells are divided in: multiple myeloma, extramedullary
plasmacytoma, and solitary plasmacytoma of bone.3
Extramedullary plasmacytomas more
comÂmonly occur in the upper part of the digestive tube and the upper airway.
We might find this type of neoplasm generally in the nasal cavity, nasal
sinuses, and the oronasopharynx.1,
2
This finding has been described
in the literature on rare occasions. Clinical symptoms can be non-specific and
often related to tracheal invasion. Croup, chronic cough, dyspnea, voice
alterations, sibilance or hemoptysis, as in our case, can be manifestations of
this disease.1,
2, 4
The diagnosis of this particular
case couldn’t be considered as extramedullary plasmacytoma itself, since this
disease refers to only one lesion without affecting the bone marrow or
skeleton, and without causing anemia, hypercalcemia or renal alterations.5
Our patient shows multiple
myeloma refractory to treatment. It is true that 20% of patients with
extramedullary plasmacytomas can progress to multiple myeloma.3
The presence of extramedullary
disease in a patient diagnosed with multiple myeloma is associÂated with a
worse prognosis and could be related to secondary changes in the cell clone,
aggressive progression of the disease or treatment resistance, like in our
case.6
The cell clone that is
responsible for the myÂeloma could even be different from the one responÂsible
for the extramedullary plasmacytoma, thus the treatment becomes complex.6
The treatment of soft-tissue
plasmacytomas is controversial, and is commonly managed with surÂgery or
radiation therapy.5 In our patient, the lesion was resected by endobronchial
laser vaporization. Despite the resection, the positron emission tomograÂphy
showed a metabolically active uptake in the site where the lesion had
previously been found, so it will be necessary to perform a clinical follow-up
in order to evaluate the effectiveness of the intervention.
Conflict of interest
The authors declare that there is
no conflict of interest.
REFERENCES
1. Sukumaran
R, Nair RA, Jacob PM, Koshy SM, Mathew AP.
Extramedullary Plasmacytoma of the Trachea. Head Neck Pathol. 2014;8:220-4. https://doi.org/10.1007/s12105-013- 0491-7
2. Dammad
T, Jalil BA. Extramedullary
plasmacytoma presenting with acute airway compromise,
treated with emergent rigid bronchoscopic resection. J Bronchol InÂterv
Pulmonol. 2016;23:e18-20.
https://doi.org/10.1097/LBR.0000000000000266
4. Jizzini
MN, Shah M, Yeung SCJ. Extramedullary
PlasmaÂcytoma Involving the Trachea: A Case Report
and LiteraÂture Review. J Emerg Med
[Internet]. 2019;57(3):e65-7. https://doi.org/10.1016/j.jemermed.2019.05.032
5. Soutar
R, Lucraft H, Jackson G, ,
et al. Guidelines on the diagnosis and management of solitary plasmacytoma of
bone and solitary extramedullary plasmacytoma. Br J Haematol.
2004;124:717-26. https://doi.org/10.1111/j.1365-
2141.2004.04834.x
6. Oriol A. Multiple myeloma with
extramedullary disease. Adv Ther. 2011;28(SUPPL.
7):1-6. https://doi.org/10.1007/s12325-011-0079-0