Autor Carnero Echegaray, JoaquĂn1-2-3, Motti, Victoria1-4, Gil Rossetti, Gregorio1-4-6
1Santa Catalina NeurorrehabilitaciĂłn ClĂnica y Cuidados CrĂticos CrĂłnicos, Autonomous City of Buenos Aires (CABA), Argentina. 2Hospital General de Agudos J. M. Penna, CABA, Argentina. 3Associate professor. Universidad Abierta Interamericana. 4Hospital General de Agudos Carlos G. Durand, CABA, Argentina. 5ClĂnica Basilea, CABA, Argentina. 6ClĂnica de InternaciĂłn Aguda en RehabilitaciĂłn y CirugĂa (CIAREC), CABA, Argentina.
https://doi.org/10.56538/ramr.RASE9918
Correspondencia : Santa Catalina NeurorrehaÂbilitaciĂłn ClĂnica. Respiratory Kinesiology Service. RepĂşbliÂca Bolivariana de Venezuela 2592 C1096 - Autonomous City of Buenos Aires, RepĂşÂblica Argentina. E-mail: jcarneroechegaray@gmail.com
ABSTRACT
It is essential to prioritize the
decannulation of tracheostomized patients. A successful procedure could avoid
prolonged hospital stay. Accordingly, there could be a reduction in mortality.
Removing the tracheotomy cannula is a very controversial issue, because there
are different types of strategies and approaches to do so. The prolonged use of
the cannula must be avoided, since it entails different complications such as
tracheal malacia, tracheal stenosis, tracheoesophageal fistula, and
functionally altered swalÂlowing and phonation; thus, it is very important to
be able to know exactly which are the variables that need to
be measured before a patient is decannulated. Several pubÂlished studies
disagree on which are the best indicators that should be observed to be
successful. So, the objective of this review was to analyze which are the most
effective target variables when performing the decannulation.
Key words: Tracheostomy; Decannulation; Intensive care Unit
RESUMEN
Es imprescindible poder priorizar la decanulación
de los pacientes traqueostomizados. El éxito en el procedimiento
podría evitar estadías hospitalarias prolongadas y, por
consiguiente, llegar a disminuir la mortalidad. La retirada de la cánula
de traqueostoÂmía es un tema muy controversial, dado que, para lograrla,
existen diferentes tipos de abordajes y estrategias. Teniendo en cuenta que su
uso prolongado debe ser evitaÂdo, ya que conlleva a diferentes complicaciones,
como traqueomalacia, estenosis traÂqueal, fistula traqueo-esofágica,
alteraciones funcionales en la deglución y la fonación, es de
suma importancia poder conocer con exactitud cuáles son las variables
que mensurar para que el paciente pueda ser decanulado. Diversos trabajos
publicados difieren en cuáles son los mejores indicadores que deben ser
observados para lograr el éxito. Por lo tanto, el objetivo de la
presente revisión es analizar cuáles son las vaÂriables objetivables
con mayor eficacia al momento de llevar a cabo la decanulación.
Palabras clave: Traqueostomía; Decanulación; Unidad de cuidados intensivos
Recibido: 01/31/2022
Aceptado: 05/30/2022
INTRODUCTION
The tracheostomy (TQT) is one of
the most comÂmonly used procedures at the Intensive Care Unit (ICU) in patients
with prolonged invasive mechanical ventilation (PIMV).1, 2 It is performed in 34% of patients with
invasive mechanical venÂtilatory support (IMVS) for more than 48 hours.3 It is also
indicated in patients with poor secretion management, with alterations in the
upper airway, extubation failure, and prolonged mechanical ventilation.4
It is essential to prioritize the
decannulation of tracheostomized patients, because if the procedure is
successful, prolonged hospital stay (with greater predisposition to infections)
could be avoided; thus, mortality could be reduced. Various publications
analyze if the success or failure of decannulation are determining factors of
patients’ survival. In a multicenter study about tracheostomized patients
carried out in Argentina, Díaz Ballve et al found that mortality was
higher in patients who couldn’t decannulate. Among patients who couldn’t be
decannulated, after 90 days, only 64% were alive, whereas those who could be
decannulated reached 94.1% survival.5
Scrigna et al observed in an analysis of 181 patients with TQT
that having been decannulated was a protective factor for mortality during
hospitalization.6 On the other
hand, Rapela et al analyzed patients with chronic obstructive pulmonary disease
(COPD), tracheostomized under PIMV, and observed that most patients who
couldn’t be weaned from IMVS (47.5%) were either referred to a higher
complexity health center or died (78.9%).7
Another multicenter study conÂducted in Germany which observed
831 tracheosÂtomized patients with a diagnosis of neurological origin upon
hospital admission found that 93.5% of the 62 patients that died hadn’t been
able to be decannulated.8
We should also consider that, due
to the facts previously described, delayed decannulation could increase public
health costs.9
Removing a TQT cannula is a very
controÂversial issue, because there are different types of strategies and
approaches to do so, according to the published bibiliography.4 Knowing that the prolonged use of the
cannula must be avoided, because it entails different complications such as
tracheal malacia, tracheal stenosis, tracheoesophaÂgeal fistula, and
functionally altered swallowing and phonation,10-13 it is very important to be able to know
exactly which are the variables that need to be taken into account for a
patient to be successfully decannulated.
Various published studies
disagree on which are the best indicators that should be observed to achieve a
successful removal of the tracheostomy cannula.5, 14, 15 So, the
objective of this review was to analyze which are the most effective target
variables when performing the decannulation.
MATERIALS AND METHODS
Bibliographic search
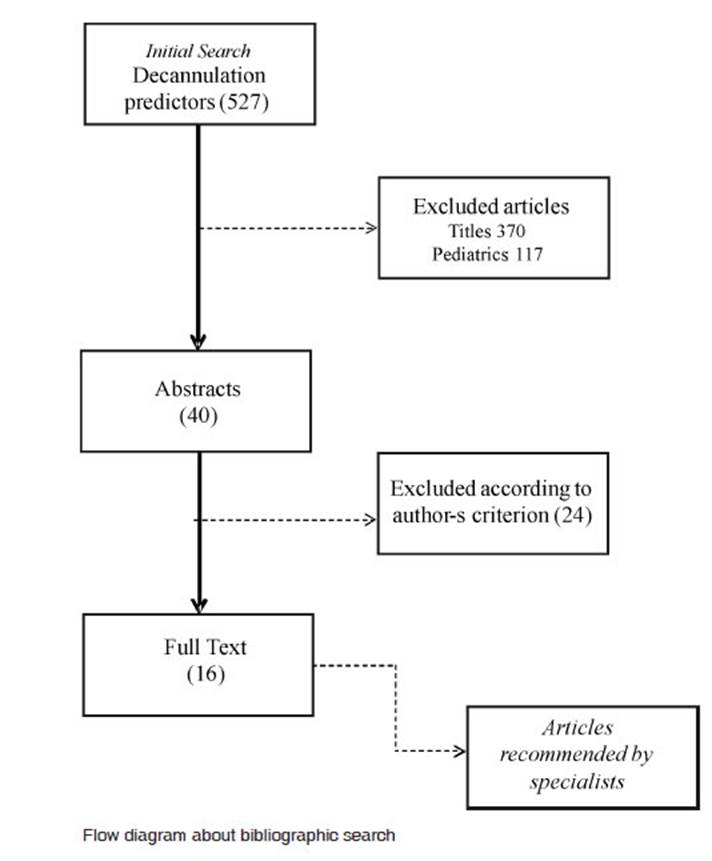
Bibliographic search was
performed in the following dataÂbases: LILACS, PUBMED, MEDLINE and SciELO,
using the following keywords: tracheostomy, decannulation, termination of
tracheostomy, swallowing disorders and decannulation predictors during the period
between 2010 and 2020. The other studies were obtained through recomÂmendation
of specialists, and so the selection was completed according to the criterion
and objective of the study.
We excluded articles about
pediatric patients and those in which the title did not match the objective of
the work.
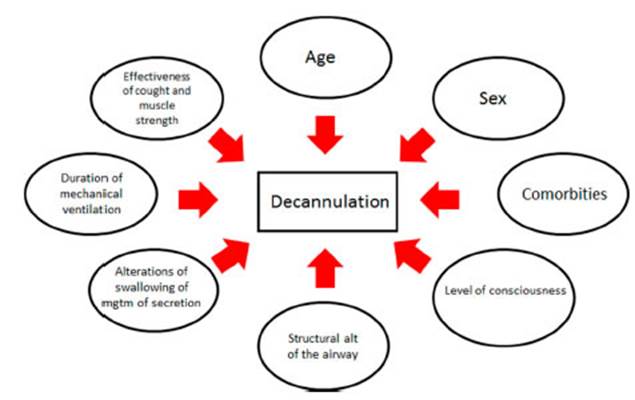
Different decannulation
predictive indicators (of both failure and success) were evaluated:
- Age: expressed in years.
- Sex: female and male.
- Comorbidities: history
of admission to the Intensive Care Unit or mechanical ventilation weaning and
rehabiliÂtation center (MVWRC).
- Level of consciousness: state
of consciousness before decannulation.
- Structural alterations of
the airway: anatomical alterations produced during the patient’s stay with
an artificial airway.
- Alteration in swallowing or
management of seÂcretion pooling: alterations produced as a consequence of
treatment.
- Duration of mechanical
ventilation: number of days with invasive mechanical ventilation.
- Effectiveness of cough and
muscle strength: evaluated before decannulation.
Development
The objective of the
decannulation process is to reÂmove the artificial airway. Generally, it is
based on a protocol that varies according to the attending inÂstitution. 31%-44%
of tracheostomized patients are decannulated, with a percentage of
recannulation of 3%-4% according to published information.1, 6, 16, 17, 18 Taking into account the low percentage of
success and complications associated with decannulation failure (alteration of
consciousness, poor manageÂment of secretions, impossibility to wean from
invasive mechanical ventilatory support, weakness of respiratory muscles and
structural alterations of the airway), decannulation becomes an extremely
important topic of study, since multiple variables involved in the process have
to be analyzed. These variables are represented in Figure 1.
Age
According to the bibliography,
the mean age of paÂtients who require a tracheostomy cannula ranges from 55 to
70 years.5,
19-22 Distefano
et al observed that 40% of decannulated patients from a total of 50 had a mean
age of 66 years, whereas Scrigna et al obtained a median of 63 and 66 years of
success and failure, respectively, with 44% of success in decannulation.6, 23
Thomas and Schneider observed
that successÂfully decannulated patients had a mean age of less than 70 years.22, 24 In turn,
Díaz Ballve et al found in their univariate analysis that advanced age
(more than 70 years) was a predictive factor independently associated with
decannulation failÂure.5 In the same
way, Budweiser et al found that having a median of age of 72 years is
predictive of recannulation.25 It is worth mentioning
that, whereas the mean age of the observed populaÂtions of tracheostomized
patients from the studies published by Luo and Berney was 44 and 47 years,
those patients had been admitted due to multiple trauma, which was one of the
possible causes of a reduction in the age range.26, 27 Age is possibly a factor to be highlighted
when we talk about the possibility to decannulate. Old patients generally show
varied medical records and comorbidities on admission to the Intensive Care
Unit (ICU), thus complicating the decannulation process, which is even more
difficult in cases of Intensive Care Unit-acquired weakness.
Sex
In almost all the analyzed
bibliography, males were predominant in both the group of patients who couldn’t
decannulate and also in the failure group that required recannulation. Scrigna
et al provide support for this finding in their multivariate analysis, in which
they found that the male sex is a risk factor independently associated with
decanÂnulation failure.5,
6, 14, 15, 19, 20, 23 However, Tawfik et al found, in their search
for risk factors associated with decannulation following laryngotracheal reÂconstruction,
that female patients with tracheosÂtomy cannula were predominant. Moreover,
most patients who didn’t have success in decannulation were females (62.2%).
This author didn’t analyze the reason for such predominance, but observed that
almost 60% of the sample had a history of gastroesophageal reflux (GER). This
could be the cause of tracheal stenosis by mucosal injury and consequent
requirement of airway reconstruction. GER is one of the causes of failure in
post-surgical decannulation.28 Taking this
finding into considÂeration, it is necessary to remember that females
predominate in patients with history of GER.29
The latter author found that decannulation failed in a great
percentage of female patients, but females were predominant in that sample,
clearly showÂing that male patients are the ones who definitely entail more
risks of failure in the decannulation process, according to the bibliography.
Comorbidities
There is strong predominance of
patients with history of cardiovascular disease, followed by toxic-metabolic
history, among patients with TQT adÂmitted to the ICU or the MVWRC.5, 6, 30 On the other
hand, Stelfox observed in his two studies published for two consecutive years
about tracheostomized patients, that subjects with terminal renal disease were
less succesful in decannulation compared to patients with chronic respiratory
failure.31, 32
Hernández et al compared
two groups: one consisted of patients with TQT with predominance of neurologic
history and difficulty in managing secretions; in the other one, there were
patients with TQT under PIMV with predominant history of COPD, diabetes
mellitus, respiratory diseases, arterial hypertension, and a similar APACHE II
average score of 18 and 19, respectively, where no significant difference was
found between both groups as regards the percentage of decannulaÂtion success,
which was 90% and 85% of the total number of patients.21
It is worth mentioning that, in
the multivariate analysis of Scrigna et al, the presence of respiratory history
was associated with decannulation failure, taking into account the fact that in
the cohort of their study, the neurologic history was predominant.6
Comorbidities could possibly have
a major role in the course of the patient’s hospitalization. If the patient
also has an extensive history, treatment complexity becomes even more evident.
Patients with respiratory and neurologic history are the ones who have greater
difficulty in weaning from mechanical ventilation and also in the decanÂnulation
process. The reason for this may be the physiopathology of these comorbidities,
which pose a big challenge to treating professionals in order to reach
treatment success.
Level of consciousness
There is lack of consensus in the
bibliography about which level of consciousness is necessary to begin the
decannulation protocol. This is a such a controversial issue that many authors
deÂcided not to include in the decannulation protocol those patients who can’t
provide minimum active cooperation with a value of more than 8 in the Glasgow
Coma Scale (GCS).12,
19, 21, 33, 34
Villalba et al state that the level of consciousness can be a
determining factor of the process of decannulation if it interferes with the
protection of the airway.4 However,
Stelfox et al came to the conclusion (through a survey) that, whereas the level
of conÂsciousness was one of the determining factors of decannulation success,
it wasn’t an indispensable requirement, so it was considered a secondary variÂable.
The main variables that were studied were tolerance to occlusion and cough
effectiveness.32
Choate et al believe the state of
consciousness is a predictor of decannulation,35
whereas Bellon et al conducted a study that analyzed the relationÂship
between the chronic alteration of the state of consciousness and decannulation,
using the coma recovery scale-revised (CRS-R) as a measurement tool, and observed
that of the 33% of patients who were able to decannulate and had chronic alteraÂtion
of the state of consciousness, 40% had unreÂsponsive wakefulness (GCS < 8)
the moment the TQT cannula was being removed.30
The Glasgow scale is not recommended for the population of
patients with chronic alteration of the state of consciousness.30
Structural alterations of the airway
Both the placement and prolonged
presence of an artificial airway (AAW) cause the patient to be at risk of
having structural lesions such as stenosis, granulomas and tracheal malacia.10 One of the
most prevalent structural complications present when performing a
fibrobronchoscopy before decannulation were granulomas.36, 37 A large perÂcentage of patients with
granulomas had a mild lesion of the airway that did not exceed the 50%
occlusion of the tracheal tube, so, according to Rumbak et al, in patients with
a good general conÂdition, it would not prevent a successful decannulaÂtion.
They also observed that a lesion is clinically important if it functionally
obstructs more than 50% of the tracheal tube, because if the trachea has an
approximate diameter of 1.6 cm to 1.8 cm, an 8 mm lesion (the most common
internal diameter of TQT cannulas) wouldn’t offer strong resistance to tolerate
spontaneous ventilation.38
On the other hand, some authors
consider stenosis as one of the most severe complications. Even though stenosis
has a 3%-12% prevalence in patients with TQT, it could prevent decanÂnulation
given its difficult surgical resolution or possible progression, if it occludes
more than 50% of the tracheal tube.36 It’s
important to mention that Planells et al, just like Epstein et al, found an
association between advanced age and the deÂvelopment of tracheal stenosis. Also,
the number of days with an artificial airway proved to be a significant
variable for the development of these complications, with a median of 84.5 days
[IQR, interquartile range of 49-135.5].10, 38
Mathur et al observed that age
and number of days with TQT were associated with the presence of structural
complications and the difficulty to achieve decannulation; but they didn’t find
any significant correlation between the failure of the procedure and the
findings of the fibrobronchosÂcopy; thus, they came to the conclusion that this
tool must be used as part of the decannulation and not as a determining factor
of the process.39 On the
contrary, Enrichi et al consider the endoscopic evaluation of the airway as a
determinant of the successful removal of the tracheostomy cannula.40
To conclude, we must highlight
the fact that, whereas tolerance to the occlusion of the tracheosÂtomy cannula
not only depends on the permeability of the airway, several authors thought of
it as a variable of success in the process of decannulaÂtion. Enrichi et al
found that the combination of an adequate permeability of the airway evaluated
through an endoscopy, and a positive result in the blockage testing of the
tracheostomy cannula resulted in a sensitivity of 94.1% and a specificity of
94.7% for decannulation. We have to mention that separate studies of these
variables showed lower percentages of sensitivity and specificity.40
Therefore, the fibrobronchoscopy
and the evaluÂation of the TQT cannula occlusion would be the most useful tools
to get close to decannulation success. The most prejudicial lesion is stenosis,
which occludes more than 50% of the tracheal tube, preventing decannulation and
probably requiring a surgical resolution, laser therapy or an endoscopic procedure.
Alteration in swallowing and management of secretion pooling
Some authors consider that
swallowing solid, semi-solid or liquid food is not determinant of decanÂnulation,32, 34 whereas other
researchers think it is necessary to formally and thoroughly study this
function for the purpose of achieving a successful artificial airway removal.12
At present, the use of the Blue
Dye Test as a preÂdictor of decannulation success is being questioned
because, despite the fact that it is highly sensitive, it has low specificity;
thus, it may show false negaÂtive results.41
However, Enrichi et al conducted a study on patients with
acquired brain injury in a post-acute center where they analyzed different
variables used in an experimental decannulation protocol and came to the
conclusion that the Blue Dye Test together with other factors, such as
ocÂclusion of the TQT cannula, endoscopic evaluation of airway permeability,
and the instrumental swalÂlowing assessment should be used as a decannulaÂtion
prediction tool. When considered individually, the variables showed high levels
of reliability, but when they were all combined, increased sensitivÂity (100%)
and specificity (82%) were found the moment decannulation was achieved.40
Fernández Carmona et al,
in a study of 2012 describe multiple conditions produced by the use of this
device and focus on oropharyngeal dysphagia in patients with TQT. They develop
an algorithm that has to be followed for the difficult treatment of this
condition and recommend the use of video fluoroscopy, fibroscopy and isotopic
transit as a tool for the study of patients with suspected dysphagia. In
patients without this suspicion, the approach includes methylene blue staining
(clearing its low specificity) and multiple coadjuvant strategies for the
evaluation of this situation in order to remove the patient’s ventilatory
support.42
Tracheostomized patients
diagnosed with COPD have a complex approach, because, apart from having an
artificial airway, there is asynÂchrony between ventilation and swallowing.
This asynchrony is inherent to the disease and gets worse with the exacerbation
of the underlying disease.43-45
Microaspirations, together with the presence of
gastroesophageal reflux between 17%-78%, with risk of aspiring gastric content,
cause these patients to have greater difficulty in weaning from mechanical
ventilation and a low decannulation rate,6, 7 resulting in prolonged use of the tracheostomy
and higher risk of suffering exacerbations that increase mortality.46
In view of the above, the
swallowing tests would be useful tools for any situation in which, for some
reason (patient’s disease on admission to the ICU, history, prolonged
treatment of invasive mechanical ventilation), there is any suspicion of saliva
bronchoaspiration. We should also explain that oral feeding isn’t an essential
requirement for decannulation, since there are other routes through which food
can be supplied that allow for the removal of the ventilatory support.
Duration of mechanical ventilation
The study of Sansone et al, with
an analyzed sample of 437 patients, showed that the duration of mechanical
ventilation didn’t have a significant efÂfect on successful weaning and
long-term survival, but would probably have a dangerous and counterÂproductive
effect in relation to the decannulation rate, because it increases the hospital
length of stay.47 In the same
way, several authors were able to show that the PMV intervenes in the failed
removal of the tracheostomy cannula through different factors. These studies
were conducted in heterogeneous populations, strengthening this concept.19, 21, 26
The complications related to PMV
entail indiÂrect negative effects on decannulation. Heidler et al suggest that
the absence of physiological airflow through the upper airway causes sensory
damage due to lack of stimulation of the chemoreceptors and pressure in the
laryngeal mucosa which, together with the tracheal tube cuff pressure for
prolonged periods of time caused by the difficulty in weaning from IMVS, extend
the duration of the artificial airway and complicate decannulation.
According to what has been
mentioned, the use of IMVS for prolonged periods of time complicates
decannulation but not long-term survival. We can analyze the possibility that
maybe the cause of decannulation failure isn’t the PMV itself, but the critical
state or the patient’s comorbidities that prevent the weaning process.
Effective cough and muscle strength
Back in 1996, Bach showed that in
patients with respiratory failure produced by different causes and etiologies,
the peak cough flow (PCF) was one of the most important predictive factors
(together with vital capacity) for decannulation, which obÂtained a reference
value that had to exceed 160 L/min.48
Fluctuating levels of
consciousness shouldn’t be conditioning factors of decannulation,30 however, a
study carried out in Hong Kong analyzed if the induced peak cough flow (iPCF)
in neurosurgical patients with alteration of consciousness was a predictor of decannulation
success. The results of the study showed that 66% of a total of 32 patients
were successfully decannulated, 2% required reÂcannulation, and 28% couldn’t be
decannulated according to the study’s criteria. Also, the multiÂvariate
analysis showed that, a value ≥ 29 L/min of iPCF is independently
associated with decanÂnulation success.49
On the other hand, in order to
confirm cough effectiveness, Ceriana et al used the maximum expiratory pressure
(MEP) with a cut-off point of 40 cmH2O and obtained 80% success in
decanÂnulation34.
Then, Hernández et al observed that, for a patient to be decannulated,
he/she shouldn’t exceed two secretion aspirations, with an interval of 8 h
between each, and also the quality of those aspirations had to be considered21.
The surveys conducted by Stelfox
among health professionals addressed this problem, where cough effectiveness
and secretion management, together with other variables (patient’s state of
consciousÂness and tolerance to occlusion) were the most important factors for
patient decannulation.31,
32
There is an extensive
bibliography of published writing supporting the fact that cough strength and
good secretion management are predictors of decannulation success19, 26, 36, 50, 51 However,
Enrichi et al found that, in tracheostomized patients with acute brain injury,
both voluntary and reflex cough are important variables to be evaluated, but
they are not determinant of decannulation. In this work, the cough evaluation
showed high sensitivÂity (85%) but low specificity (31.5%) with a low positive
predictive value.40
With regard to the
aforementioned, Choate et al found that retention of secretions and the
impossibility to remove them were the main comÂplications involved in
decannulation failure. As a result of that study, 4.8% (39 of 823 patients) had
decannulation failure, 60% of which failed due to poor secretion management.35
Regarding the evaluation of
muscle strength and cough, probably the MEP and peak cough flow are the main
variables to consider when decanÂnulating a patient. They are consistent with
good secretion management; thus, we could think that with numbers exceeding the
lower limit described by the bibliography we would more effectively get closer
to decannulation.
CONCLUSION
Tolerance to the occlusion of the
TQT cannula for more than 24 h and a peak cough flow ≥ 160 L/ min are the
most determining variables of decanÂnulation success. Alterations in
swallowing, in the state of consciousness and anatomical alterations of the
airway are still controversial when evaluatÂing the decannulation process. On
the other hand, advanced age, male sex and tracheal stenosis with a tube
reduction of more than 50% are the most common risk factors associated with
decannulaÂtion failure.
When predictor variables of
success or failure in the process of decannulation with the most scientific
evidence are those that can be observed when evaluating the patient, it would
possibly be easier to recognize if that procedure can be used or not, and if it
can’t be used, to acknowledge the cause that prevents it.
Most analyzed studies are
conducted in relaÂtively short follow-up period. Long-term follow-up would
allow us to know even better the impact of decannulation in patients.
It is very important to know new
variables that could predict success or failure in decannulation.
Authors have no external funding
or conflict of interest to declare.
REFERENCES
1. O’Connor HH, Kirby KJ, Terrin
N, Hill NS, White AC. Decannulation following tracheostomy for prolonged mechanical
ventilation. J Intensive Care Med. 2009; 24: 187-94.
https://doi.org/10.1177/0885066609332701
2. Tobin AE, Santamaria JD. An
intensivist-led tracheostomy review team is associated with shorter
decannulation time and length of stay: a prospective cohort study. Crit Care.
2008; 12: R48. https://doi.org/10.1186/cc6864
3. Dhand R, Johnson JC. Care of
the chronic tracheosÂtomy. Respir Care. 2006;
51(9): 984-1004.
4. Frutos-Vivar F, Esteban A, Apezteguía C, et al.
Outcome of mechanically
ventilated patients who require a traÂcheostomy. Crit Care Med. 2005; 33(2): 290-8.
https://doi.org/10.1097/01.ccm.0000150026.85210.13
5. Diaz Ballve P, Villalba D,
Andreu M, et al. Decanular. Factores predictores de dificultad para la
decanulación: Estudio de cohorte multicéntrico. Rev Am Med Resp. 2017; 17: 12-24.
6. Scrigna M, Plotnikow G, Feld
V, et al. Decanulación después de la estadía
en UCI: Análisis de 181 pacientes traqueotoÂmizados. Rev Am Med Resp
2013; 13: 58-63.
7. Rapela L, Plotnikow G, Feld V, et al
. Factores de riesgo para el fracaso de destete en una población
de pacientes con EPOC en ventilación mecánica prolongada. Rev Am Med Respir. 2014; 14: 232-43.
8. Heidler MD, Salzwedel A,
Jöbges M, et al. Decannulation of tracheotomized patients after long-term
mechanical ventilation - results of a prospective multicentric study in German
neurological early rehabilitation hospitals. BMC Anesthesiol.
2018; 18: 65. https://doi.org/10.1186/s12871-
018-0527-3
9. Engels PT, Bagshaw SM, Meier
M, Brindley PG. TracheosÂtomy: from insertion to
decannulation. Can J Surg. 2009; 52: 427-33.
10. Epstein SK. Late
complications of tracheostomy. Respir Care. 2005; 50: 542-9.
11. Heffner JE, Miller KS, Sahn
SA. Tracheostomy in the intensive care unit. Part 2:
Complications. Chest. 1986; 90:
430-6. https://doi.org/10.1378/chest.90.3.430
12. Christopher KL. Tracheostomy decannulation. Respir Care. 2005;
50: 538-41.
13. O’Connor HH, White AC.
Tracheostomy decannulaÂtion. Respir Care. 2010; 55: 1076-81.
14. Medeiros GC, Sassi FC,
Lirani-Silva C, Andrade CR. CriÂteria for tracheostomy decannulation:
literature review. Critérios para
decanulação da traqueostomia: revisão de literatura.
Codas. 2019; 31(6): e20180228. https://doi. org/10.1590/2317-1782/20192018228.
15. Santus P, Gramegna A, Radovanovic D, et al. A systemÂatic review on tracheostomy decannulation: a proposal of a
quantitative semiquantitative clinical score. BMC Pulm Med 2014; 14: 201. https://doi.org/10.1186/1471-2466-14-201.
16. Martinez GH, Fernandez R, Casado MS, et al. TracheosÂtomy tube in place at intensive care unit discharge is asÂsociated
with increased ward mortality. Respir Care. 2009; 54:
1644-52.
17. Mackiewicz-Nartowicz H,
Mackiewicz-Milewska M, Lach S, Szymanska-Skrzypek A, Owczarek A. DecanÂnulation
factors in patients after serius brain injuries. Advances in Palliative
Medicine 2008; 7: 69-72.
18. Scheinhorn DJ, Hassenpflug
MS, Votto JJ, et al. Post-ICU mechanical ventilation at 23 long-term care
hospitals: a multicenter outcomes study. Chest. 2007; 131: 85-93. https://doi.org/10.1378/chest.06-1081
19. Pandian V, Miller CR, Schiavi
AJ, et al. Utilization of a standardized tracheostomy capping and decannulation
protocol to improve patient safety. Laryngoscope. 2014; 124: 1794-800. https://doi.org/10.1002/lary.24625.
20. Warnecke T, Suntrup S,
Teismann IK, Hamacher C, OelenÂberg S, Dziewas R. Standardized endoscopic
swallowing evaluation for tracheostomy decannulation in critically ill
neurologic patients. Crit Care Med. 2013; 41: 1728-32.
https://doi.org/10.1097/CCM.0b013e31828a4626
21. Hernández G, Ortiz R,
Pedrosa A, et al. The indication of tracheotomy conditions the predictors of
time to decannuÂlation in critical patients. Med Intensiva.
2012; 36: 531-9.
https://doi.org/10.1016/j.medin.2012.01.010
22. Schneider H, Hertel F, Kuhn
M, et al. Decannulation and Functional Outcome After Tracheostomy in Patients
with Severe Stroke (DECAST): A Prospective ObservaÂtional Study. Neurocrit Care. 2017; 27: 26-34. https://doi. org/10.1007/s12028-017-0390-y
23. Distéfano E, Picón Fuster S, Destefanis
C, y cols. PredictoÂres de éxito después de la
decanulación en pacientes adultos críticamente enfermos: un
estudio de cohorte retrospectivo. Rev Hosp Ital
B Aires 2018; 38: 132-8.
24. Thomas S, Sauter W, Starrost
U, Pohl M, Mehrholz J. Time to decannulation and associated risk factors in the
postÂacute rehabilitation of critically ill patients with intensive care
unit-acquired weakness: a cohort study. Eur J Phys Rehabil
Med. 2017; 53: 501-7. https://doi.org/10.23736/
S1973-9087.16.04400-2.
25. Budweiser S, Baur T,
Jörres RA, Kollert F, Pfeifer M, Heinemann F. Predictors of successful
decannulation using a tracheostomy retainer in patients with prolonged weaning
and persisting respiratory failure. Respiration. 2012; 84: 469-76. https://doi.org/10.1159/000335740
26. Luo C, Yang H, Chen Y, Zhang
Z, Gong Z. Respiratory nursing interventions following tracheostomy in acute
traumatic cervical spinal cord injury. Cell Biochem BioÂphys.
2014; 70: 455-9. https://doi.org/10.1007/s12013-014- 9940-5.
27. Berney L, Wasserfallen JB,
Grant K, et al. Acute neuÂrorehabilitation: does a
neurosensory and coordinated interdisciplinary programme reduce tracheostomy
weaning time and weaning failure? NeuroRehabilitation.
2014; 34: 809-17. https://doi.org/10.3233/NRE-141081.
28. Tawfik KO, Houlton JJ,
Compton W, Ying J, Khosla SM. Laryngotracheal reconstruction: A ten-year review
of risk factors for decannulation failure. Laryngoscope 2015; 125: 674-9.
https://doi.org/10.1002/lary.24963
29. Kim YS, Kim N, Kim GH. Sex and Gender Differences in Gastroesophageal Reflux Disease.
J Neurogastroenterol Motil. 2016; 22: 575-88.
https://doi.org/10.5056/jnm16138
30. Bellón P, Bosso M, Motti MV, y cols.
Decanulación y evoÂlución de la alteración crónica
del estado de conciencia. Rev Neurol Arg. 2020:
12: 20-6. https://doi.org/10.1016/j.
neuarg.2019.11.002
31. Stelfox HT, Crimi C, Berra L,
et al. Determinants of tracheÂostomy decannulation: an international survey.
Crit Care. 2008; 12: R26. https://doi.org/10.1186/cc6802
32. Stelfox HT, Hess DR, Schmidt
UH. A North American survey of respiratory therapist and physician tracheostomy
decannulation practices. Respir Care. 2009; 54:
1658-64.
33. Zanata Ide L, Santos RS, Hirata GC. Tracheal decanÂnulation protocol in patients affected
by traumatic brain injury. Int
Arch Otorhinolaryngol. 2014;18:108-14. https://
doi.org/10.1055/s-0033-1363467
34. Ceriana P, Carlucci A,
Navalesi P, et al. Weaning from traÂcheotomy in
long-term mechanically ventilated patients: feasibility of a decisional
flowchart and clinical outcome. InÂtensive Care Med. 2003;
29: 845-8. https://doi.org/10.1007/ s00134-003-1689-z
35. Choate K, Barbetti J, Currey
J. Tracheostomy decannulaÂtion failure rate following critical illness: a
prospective descriptive study. Aust Crit Care. 2009; 22: 8-15. https:// doi.org/10.1016/j.aucc.2008.10.002
36. Law JH, Barnhart K, Rowlett
W, de la Rocha O, Lowenberg S. Increased frequency of obstructive airway
abnormalities with long-term tracheostomy. Chest. 1993; 104: 136-8. https://doi.org/10.1378/chest.104.1.136.
37. Planells F, Villalba D,
Viviana F, et al. Prevalence and Characteristics of Tracheal Lesions Observed
in TracheÂostomized Patients J Bronchology Interv Pulmonol. 2019;
26: 119-23. https://doi.org/10.1097/LBR.0000000000000538
38. Rumbak MJ, Graves AE, Scott
MP, et al. Tracheostomy tube occlusion protocol predicts significant tracheal
obstruction to air flow in patients requiring prolonged mechanical ventilation.
Crit Care Med. 1997; 25(3): 413-7. https://doi.
org/10.1097/00003246-199703000-00007.
39. Mathur NN,
Sohliya LM. Pre-decannulation Peristomal
Findings in Tracheostomized Cases and Their Effect on the Success of
Decannulation. Indian J Otolaryngol Head Neck Surg. 2015;67
(Suppl 1): 91-7. https://doi.org/10.1007/ s12070-014-0785-4.
40. Enrichi C, Battel I, Zanetti
C, et al. Clinical Criteria for Tracheostomy Decannulation in Subjects with
Acquired Brain Injury. Respir Care. 2017; 62(10): 1255-63. https://
doi.org/10.4187/respcare.05470.
41. Béchet S, Hill F,
Gilheaney Ó, Walshe M. Diagnostic AcÂcuracy of the Modified Evan’s Blue
Dye Test in Detecting Aspiration in Patients with Tracheostomy: A Systematic
Review of the Evidence. Dysphagia. 2016; 31:
721-9. https:// doi.org/10.1007/s00455-016-9737-3
42. Fernández-Carmona A, Peñas-Maldonado L,
Yuste- Osorio E, Díaz-Redondo A. Exploración y abordaje de
disfagia secundaria a vía aérea artificial. Med Intens. 2012;36:423-33.
43. Terada K, Muro S, Ohara T, et
al. Abnormal Swallowing ReÂflex and COPD Exacerbations. CHEST.
2010;137:326–32.
https://doi.org/10.1378/chest.09-0482.
44. Cassiani RA, Santos CM,
Baddini-Martinez J, Dantas RO. Oral and pharyngeal bolus transit in patients
with chronic obstructive pulmonary disease. Int J Chron Obstruct PulÂmon Dis.
2015; 10: 489-96. https://doi.org/10.2147/COPD. S74945.
45. O’Kane L, Groher M.
Oropharyngeal dysphagia in patients with chronic obstructive pulmonary disease:
a systematic review. Rev CEFAC. 2009; 11: 499-506.
46. Clini E, Vitacca M, Bianchi
L, Porta R, Ambrosino N. Long-term tracheostomy in severe COPD patients weaned
from mechanical ventilation. Respir Care. 1999; 44: 415-20.
47. Sansone GR,
Frengley JD, Vecchione JJ, Manogaram MG, Kaner RJ. Relationship of the Duration of VentilaÂtor Support
to Successful Weaning and Other Clinical Outcomes in 437 Prolonged Mechanical
Ventilation PaÂtients. J Intensive Care Med. 2017; 32:
283-91. https://doi. org/10.1177/0885066615626897
48. Bach JR, Saporito LR.
Criteria for extubation and tracheosÂtomy tube removal for patients with
ventilatory failure. A different approach to weaning. Chest. 1996; 110: 1566-71.
https://doi.org/10.1378/chest.110.6.1566
49. Chan LY, Jones AY, Chung RC,
Hung KN. Peak flow rate durÂing induced cough: a predictor of successful
decannulation of a tracheotomy tube in neurosurgical patients. Am J Crit Care. 2010; 19: 278-84.
https://doi.org/10.4037/ajcc2009575
50. Marchese S, Corrado A, Scala
R, Corrao S, Ambrosino N. Intensive Care Study Group, Italian Association of
Hospital Pulmonologists (AIPO). Tracheostomy in paÂtients with long-term
mechanical ventilation: a surÂvey. Respir Med. 2010; 104:
749-53. https://doi.org/10.1016/j.
rmed.2010.01.003.
51. Shrestha KK, Mohindra S,
Mohindra S. How to decannulate tracheostomised severe head trauma patients: a
comparison of gradual vs abrupt technique. Nepal Med Coll J. 2012; 14: 207-11.