Autor : Gatica, David1-2, Pitrella, Alicia3, Villalobos, Walter4
1Hospital Del Carmen, Department of Pneumonology. 2Universidad Nacional de Cuyo, Faculty of Medical Sciences, Mendoza, Argentina. 3Hospital Del Carmen, Department of Diagnostic Imaging, Mendoza, Argentina. 4Fundación Escuela de Medicina Nuclear FUESMEN.
https://doi.org/10.56538/ramr.TXVT8924
Correspondencia : E-mail: drdavidgatica@gmail.com
CASE REPORT
We received a clinical medicine
cross-consultation of a 56-year-old female patient with history of apÂpendiceal mixed adenoneuroendocrine
carcinoma, diagnosed on September 3rd,
2019: pT4a pN2 pMx, who received chemotherapy as
first line of treatment. Subsequent follow-up was done through PET/ CT
(positron emission tomography/computed tomography), and the results indicated
disease progresÂsion without lung compromise. In February 2021, the patient
began treatment with immunotherapy (nivolumab/ipilimumab) until September 2021, when it was decided that
the treatment had to be susÂpended because the patient started to have
nonproductive cough, fever of 38 °C predominantly at night for one month, chest
pain and dyspnea, functional class 4 according to the mMRC
(Modified Medical Research Council) scale. She was hospitalized at the internal
medicine department with regular general condition, alert, blood pressure:
80/50 mmHg. Expansion with physiological solution with good response, blood
pressure: 100/60 mmHg, heart rate: 82 beats/min, breathing rate: 19 bpm, oxygen saturation: 95% (FiO2:
0.21). Semiology of the respiratory system: normal breath sounds. Laboratory
testing on admission: hematocrit 29%, hemoglobin: 9.8 mg/dL,
leucocytes: 13,330 mm3,
segmented neutrophils: 10,260 mm3,
band neutrophils 27 mm3,
lymphocytes: 1690 mm3,
uremia: 41.1mg/dL, creatinine:
0.99 mg/dL, normal hepatogram.
Arterial blood gases: pH: 7.45, pCO2:
36.2 mmHg, pO2: 82.6 mmHg, SatO2: 96.7%, bicarbonate: 24.7 mmol/L, lactate: 1.25 mmol/L.
Chest CT (11/10/2021) (See
Figure 1):
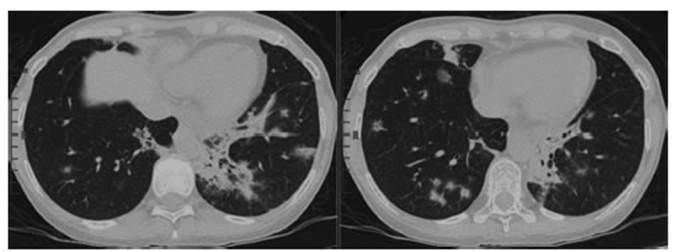
The CT shows multiple peribronchovascular âground glassâ infiltrates with central
and peripheral distribution, with compromised patchy lungs predominantly bibasilar, and consolidations with air bronchogram
in left posterior basal segment.
Which are the diagnoses?
1 Pneumonia: viral, bacterial, mycosis.
2 Progression of
oncological disease to the lungs.
3 Checkpoint
inhibitor-associated pneumonia.
During hospitalization, the
patient underwent a fibrobronchoscopy with bronchoalveolar lavage. The bacteriology report and viral
panel were negative, so the empiric antibiotic therapy was suspenÂded due to
suspected pneumonia (it started after the fibronchoscopy)
and the patient began treatment with 1 mg/kg/d of corticosteroids. The mycology
report, acid-fast bacillus culture and biopsy sent to the department of
pathological anatomy are still pending. The patient was discharged due to
improved clinical symptoms, with presumptive diagnosis of checkpoint
inhibitor-associated pneumonia.
DIAGNOSIS
Corticoids were suspended gradually
(2 months of treatment). The patient consulted again for dry cough and fever of
more than 38 °C, which was partially lowered with paracetamol,
1 g. She brought a pathological anatomy report of a transbronchial
biopsy: associated with organizing pneumonia.
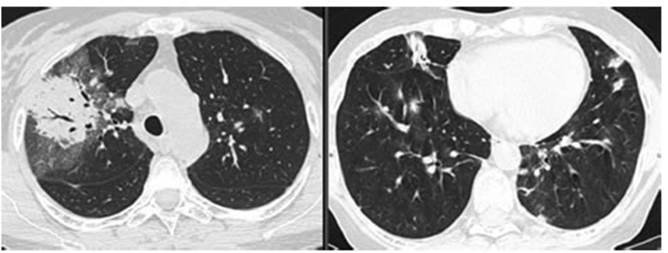
New CT requested 01/21/2022 (Figure
2): reduced bibasilar infiltrates with appearance of new inÂfiltrates in upper
lobes. Consolidation with air bronchogram
surrounded by âground glassâ opacities with interlobular septa thickening in
the anterior and posterior segment of the right upper lobe.
A bronchoalveolar
lavage was performed, in case there was an infectious process, with negative
results for microorganisms.
Basing on all this information,
the patient was diagnosed with noninfectious pneumonitis and began treatment
with corticosteroids, 1 mg/kg/d. She showed good therapeutic response, symptom
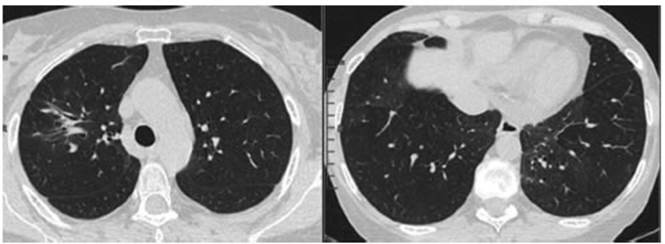
resolution and improved tomographic images after two months of treatment. CT 03/8/2022
(Figure 3): marked size reduction of consolidation in the right corner and
disappearance of the other infiltrates in lung parenchyma.
CLINICAL DISCUSSION
Including chekpoint-inhibiting
monoclonal antibodies has improved the treatment and prognosis of many patients
with cancer.1 In
this type of treatment, several checkpoint routes are used to interfere with
anti-tumor immunity, resulting in a higher activation of the patientâs immune
system.
This treatment is thought to be
less toxic than chemotherapy, but may have infectious complications, among
other things 1-5.
The most common adverse effects
related to the immune system are cutaneous, and occur in 20% to 50% of patients
(rash or pruritus) within the first two cycles. Gastrointestinal effects are
manifested from 5 to 10 weeks after the beginning of treatment. Pulmonary
effects, such as noninfectious pneuÂmonitis, are not so common, they
have a 5% incidence rate after 9 to 20 months of treatment; other reviews3 report a median time of
2.6 months. In our case, the time to develop pneumonitis was 7 months.
A review published by J. A. Ross et al6 describes an infection rate
of 18% to 19% in patients treated with checkpoint inhibitors, where the use
of corticosteroids wasnât associated with a higher risk of infection. The
proportion of patients with suspected bacterial infection was 24%, with 8% of
confirmed bacterial cultures. 29% of patients who received nivolumab
developed an infectious process, and 23% of those who received ipilimumab showed infections. Most patients were treated
empirically. No fungal or parasitic infections were identified.
The rates of noninfectious
pneumonitis were 13% with ipilimumab, compared to
2% with nivolumab. 80% of patients were hospitalized
due to noninfectious pneumonitis. According to a puÂblished study,3 the most common symptoms are
cough (60%) and dyspnea (55%). The most common tomographic patterns are
cryptogenic organizing pneumonia (COP), followed in terms of frequency by
nonspecific interstitial pneumonia, hypersensitivity pneumonitis, acute
interstitial pneumonia/acute respiratory distress syndrome. The most suitable
treatment is corticotherapy (85%); 35% of patients
began treatment again with nivolumab, and 29% of them
showed recurring noninfectious pneumonitis (which improved with
corticosteroids). 5% experienced a pneumonia outbreak after completing gradual
reduction of corticosteroids.
Most patients received
corticosteroids, with a mean time of 6.1 weeks and different doses according to
the presentation and evolution of each case.
We presented a patient who
developed noninfectious pneumonitis during the course of treatment with
immunotherapy, 7 months after the beginning of treatment. Given her clinical
spectrum and radiographic patterns, it is important to be sure thereâs no
infectious process. The patient had a good response to the initial treatment
with corticosteroids for 2 months, but showed a rebound that responÂded
satisfactorily after administering treatment. This poses the importance of
knowing the different scenarios that patients receiving immunotherapy may show,
and their difficult management.
Conflict of interests
The authors have no conflict of
interests to declare.
REFERENCES
1. Bala-Hampton
JE, Bazzell AF, Dains JE. Clinical Management of Pneumonitis in Patients Receiving
Anti-PD-1/PD-L1 Therapy. J Adv
Pract Oncol. 2018;9:422-8. https://doi.org/10.6004/jadpro.2018.9.4.5
2. Drakopanagiotakis
F, Paschalaki K, Abu-Hijleh
M, et al. Cryptogenic and secondary organizing pneumonia: clinical presentaÂtion,
radiographic findings, treatment response, and prognosis. Chest. 2011;139:893-900. https://doi.org/10.1378/chest.10-0883
3.
Koyama N, Iwase O, Nakashima E, et al. High incidence and early onset of nivolumab-induced
pneumonitis: four case reports and literature review. BMC Pulm
Med. 2018;18:23.
https://doi.org/10.1186/s12890-018-0592-x
4. Nishino M, Ramaiya
NH, Awad MM, et al. PD-1 Inhibitor-Related
Pneumonitis in Advanced Cancer Patients: Radiographic Patterns and Clinical
Course. Clin Cancer Res. 2016;22:6051-60.
https://doi.org/10.1158/1078-0432.CCR-16-1320
5. Ishiwata
T, Ebata T, Iwasawa S, et al. Nivolumab-induced
Acute Fibrinous and Organizing Pneumonia (AFOP). Intern
Med. 2017;56:2311-5.
https://doi.org/10.2169/internalmedicine.8271-16
6. Ross, JA, Komoda,
K, Pal, S, et al. Infectious complications of immune checkpoint inhibitors in
solid organ malignancies. Cancer Med. 2022;11:21- 7.
https://doi.org/10.1002/cam4.4393