Autor : Corona MartĂnez Luis Alberto1, González Morales, Iris1, Fragoso Marchante, MarĂa Caridad1, GarcĂa GĂłmez, Carlos Alberto1
1 Servicio de Medicina Interna, Hospital Universitario Dr. Gustavo AldereguĂa Lima, Cienfuegos, Cuba.
https://orcid.org/0000-0002-4160-1609
https://orcid.org/0000-0003-1663-8335
https://orcid.org/0000-0002-2170-6139
https://orcid.org/0000-0002-0131-8884
Correspondencia : Luis Alberto Corona MartĂnez. Calle 63 N² 607a, entre 6 y 8 NE, Cienfuegos, Province of Cienfuegos, Cuba E-mail: luis.corona@gal.sld.cu Hospital Universitario Dr. GusÂtavo AldereguĂa Lima, CienÂfuegos, Cuba.
ABSTRACT
Background: Risk stratification of patients with community-acquired pneumonia is a
very important process for the comprehensive evaluation of the patient.
Objective: To determine the usefulness of a tool that was created for the
stratificaÂtion of patients with pneumonia in the prognostic assessment on
admission. Materials and Methods: Descriptive research including 2,203 patients
diagnosed with community pneumonia, divided in five series between 2009 and
2020; the mortality rate was calcuÂlated according to the stratification class
and category. For the statistical analysis, we used the cross-product ratio (Odds
Ratio) with its 95% confidence interval.
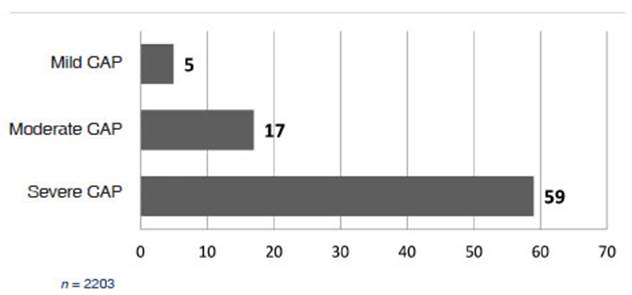
Results: We observed a progressive increase in mortality from mild to severe
class, both in the total number of cases (mild: 5%; moderate: 17%; severe: 59%)
and in each one of the series. There was statistical
significance in the mortality differences between severe and moderate pneumonia
(OR 7[5.6;8.6]). In patients who had moderate and
severe pneumonia on admission, the mortality in category B was higher than in
catÂegory A (moderate pneumonia: 18% vs. 11%, OR 1.7[1;2.7];
severe pneumonia: 68% vs. 29%, OR 5.2[3.4;8]).
Conclusions: We have proven the usefulness of the tool in predicting the progression
of patients with pneumonia and its importance in guiding the decision-making
process. The behavior of the mortality rate in the different strata of the tool
supports the purpose envisioned for it.
Key words: Pneumonia, Community-Acquired Infections, Hospital Admission
INTRODUCTION
Community-acquired pneumonia
(CAP) is an imÂportant health problem in Cuba, in the Cienfuegos province, and
also on a global level1-10 .
The high incidence and mortality
rate of this disease turn it into a challenge for the healthcare systems; other
characteristics that contribute to this challenge are the great damage it
causes to the elderly11, 12,
and the fact that ageing population is one of the features that characterizes
many counÂtries in general, and our national and provincial context in
particular, from a demographic point of view10,
13.
Efforts to create instruments
that allow for the initial prognostic assessment of patients with CAP are not
recent14: some of this
working tools, such as the CURB-65 (or its variant, the CRB-65) and the
pneumonia severity index (PSI)15, 16, to give just two
examples, have been widely used in the most diverse scenarios. We must
recognise that most societies of Internal Medicine worldwide have used some of
these tools for risk assessment in patients with CAP in the emergency
department17-20.
The Internal Medicine Department
of our InÂstitution introduced the stratification of patients with CAP in 2001,
and used the PSI. But it wasn’t a favorable experience, since the
stratification index, an indicator used to evaluate the process, decreased
progressively and reached very low valÂues. This situation entailed a critical
analysis of the tool that we had been using and, accordingly, the creation and
introduction of our own instruÂment, built from a
qualitative approach and called “IENAC” (instrument of stratification of
patients with community-acquired pneumonia, for its acÂronym in Spanish).
Unlike most widely used scales,
as the ones alÂready mentioned, the IENAC doesn’t have the aim of establishing
the patient’s prognosis on hospital admission; its function has been to help
the genÂeral practitioner with the decision-making process regarding treatment
behavior and management.
Apart from that function, the
purpose for which the IENAC was created suggests a secondary yet evident
usefulness in establishing an estimation of what will happen with the patient
throughout the course of the disease, considering such prognosis in terms of
probability of having a fatal outcome.
The objective of this work was to
determine the usefulness of the IENAC in the prognostic assessÂment of patients
with CAP on hospital admission.
MATERIALS AND METHODS
Observational,
descriptive-design study including a populaÂtion of 2, 203 hospitalized patients
with the same diagnosis of CAP both on admission and discharge, between June 1,
2009 and January 30, 2020, distributed in five series. The diagnosis of pneumonia, verified by the authors, has been based on
established clinical, radiological and necropsic (if applicable) criteria5, 17, 21 ; for the
community-acquired origin, we checked if the patients weren’t hospitalized or
hadn’t been admitted to a hospital 14 days before the onset of symptoms3, 22, 23 .
Techniques and Procedures
Information was obtained
retrospectively. The authors located and reviewed each patient’s medical
record, and ensured the presence of clinical and radiological inforÂmation
necessary to do control stratification sampling independent of the
stratification performed in the emerÂgency department. In some cases, certain
information was clarified directly with the patient or his/her relatives. All
the patients were divided into severity strata according to the IENAC criteria.
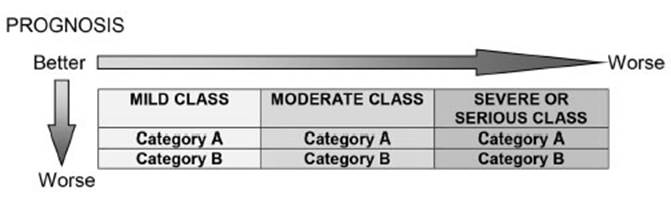
Description of the IENAC
The IENAC is based on the general
practitioner’s use of clinical information supplemented with radiological inforÂmation
(Chart 1) in order to classify the patient into one of three classes, according
to the severity of the process: mild, moderate or severe pneumonia.
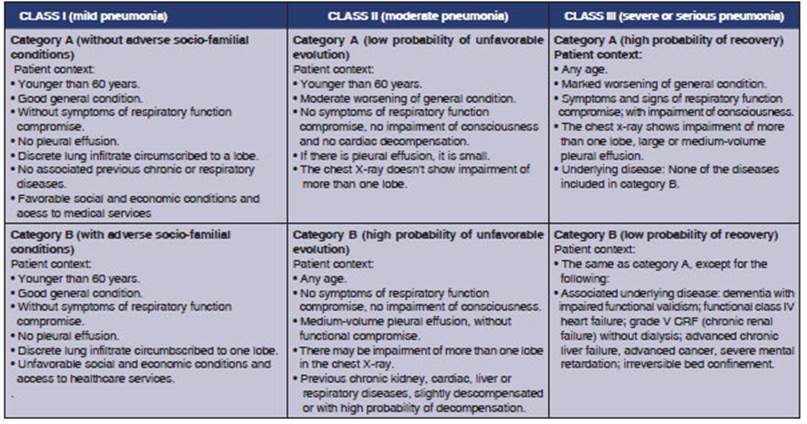
In turn, each class is divided
into two categories (A or B), in accordance with specific criteria for each
class. In patients with mild pneumonia, the criterion used is the existence or
non-existence of some factor of whatever nature that limits or affects the
possibility of receiving outpatient treatment. In patients with moderate
pneumonia, the criterion is relaÂted to the existence of some particularity
that increases the probability that the patient shows an unfavorable disease
course, even if his/her condition isn’t severe at the moment of the initial
assessment. In the case of patients with severe or serious pneumonia, the criterion
is related to the analysis of the patient’s odds of recovery.
Thus, class and category
integration give place to six strata of patients (Chart 2).
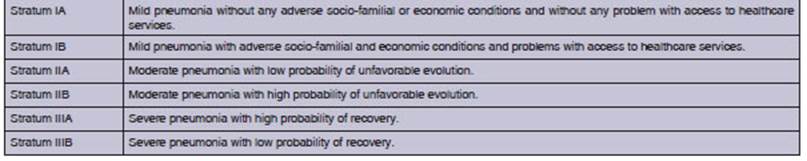
Stratification through the IENAC
implies the physician’s compliance of certain suggestions related to four
aspects of the patient’s management: the specific area inside the emergency
department where the patient is going to receive medical care (urgency with no
immediate risk of death, or yellow zone/emergency with immediate risk of death,
or red zone); the question as to whether the patient needs to be hospitalized
or not; the location of the patient inide the institution, in case he/she needs
hospitalization (location in conventional ward or in the intensive care unit);
and the empiric antimicrobial to be used initially if there isn’t any special
situation that justifies another more sepcific therapeutic approach (Chart 3).
We proceeded with the
determination of mortality as an outcome measure in each class and category
(strata), accorÂding to each series and in the total number of cases. The
mortality comparison was made both in the horizontal sense of the instrument
(comparison between classes) and in the vertical sense in each class
(comparison between categories).
For the statistical processing of
data we used the SPSS program, version 15.0 for Windows. Results are shown in
tables and graphics, expressed in numbers and percentages.
Statistical analysis
For the statistical analysis of
the results, we used the cross-product ratio (odds ratio, OR) with its
95% confidence interval.
Ethical considerations
Given the
characteristics of the study, particular bioethical considerations aren’t
necessary. However, we have ensured the strictly scientific use of the obtained
results and stated opinions. The study was evaluated and approved by the Ethics
Committee of the Institution.
Study Limitations
The subjects of the
research were patients attended under real healthcare conditions of an
emergency department. Almost all the information used for the research has been
gathered under those conditions, considering the implications of that situation
in its full reliability and proper registration in the medical report. The
authors recognize that the retrospective reconstruction of the patient’s
condition upon admisÂsion for the control stratification, a key procedure for
the development of the research, includes inevitable risks with certain degree
of inaccuracy that may have influenced the results.
The authors recognize
that in the outcome to be meaÂsured (mortality) there may be a great diversity
of factors, including those related to the intervention of the general
practitioner post-admission; these factors are not consideÂred in this study
due to the complexity they would imply for the analysis.
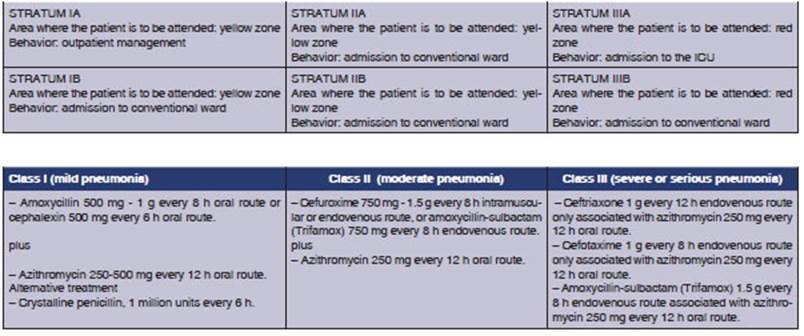
RESULTS
Taking into account all the cases
of the study, we observed a progressive increase of mortality from the mild to
the severe or serious classes (Figure 1). The evident differences observed in
the mortality rate of patients with moderate pneumonia versus those with severe
pneumonia were statistically significant (OR 7 [5.6;8.6]).
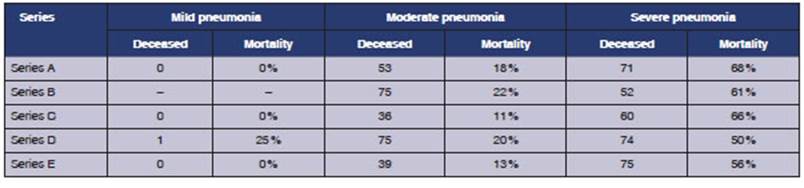
The same behavior was
observed in each of the series that form part of the study population (except
for series D, in which the order of the mild and moderate series was inverted,
conditioned by the low number of patients in the mild class), with significant
differences between patients with moderate and severe pneumonia, in all the
series (series A: OR 9.2[5.5;15.2]; series B: OR 5.4[3.3;9]; series C: OR
16.2[9.2;28.3]; series C: OR 3.9[2.6;6]; series E: OR 8.5[5.3;13.8]) (Table 1).
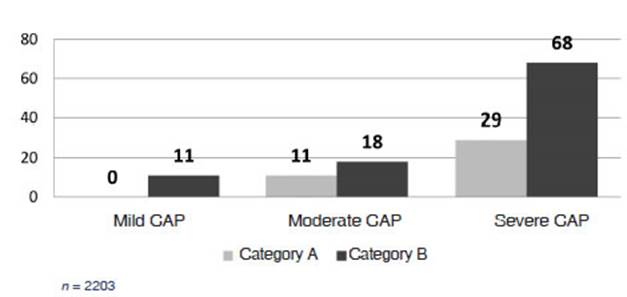
In the same way, the
three classes showed a higher mortality rate in category B than in category A
(Figure 2); this was significant both in patients with severe pneumonia (OR
5.2[3.4;8]) and those with moderate pneumonia (OR
1.7[1;2.7]).
This analysis between
categories (vertical comparison) and classified by study series (Table 2)
showed the same mortality behavior for the total number of cases: higher probability
of dyÂing in patients from category B than those from category A in each of the
five series, regardÂless of the initial degree of severity (given the low
number of patients hospitalized with mild pneumonia, no category comparison was
made in this class).
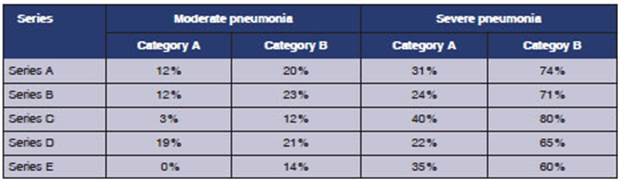
Differences in
mortality between categories A and B were statistically significant in patients
with severe pneumonia in all the independent seÂries (series A: 6[1.8;19.2]; series B: 7.8[2.2;26.8]; series C: 6[2.2;15.7];
series D: 6.5[2.9;14.4]; series E: 2.7[1;7.4]), which is not the case with
patients with moderate pneumonia.
DISCUSSION
The results obtained have
revealed an existent close relationship between the probability of dyÂing from
CAP and the classification strata of the patient with pneumonia, based on the
criteria suggested by the IENAC for patient stratification.
It is necessary to
repeat that the IENAC hasn’t been essentially created as a tool to establish a
prognosis, but as an instrument that guides the physician in the
decision-making process related to the patient’s management, basing on the
patient’s classification of severity degree on admission to the emergency
department.
However, it is
reasonable to assume that patient classification into three classes according
to the seÂverity of the disease implies a prognostic element: the patient with
mild pneumonia should have a better prognosis than the patient with moderate
pneumonia, whereas the patient with severe or serious pneumonia should have a
worse prognosis than the patient with moderate pneumonia. The results obtained
from the comparison between classes (horizontal direction of the instrument)
confirm this supposition: interestingly enough, in 59% of patients with severe
CAP (according to the criteria of the IENAC), the therapeutic intervenÂtion was
unsuccessful.
As we already
explained, apart from the severÂity assessment of the pneumonic process (which
determines the three classes), patient stratificaÂtion through the IENAC is
carried out with other features based on different criteria for each straÂtum
or class, thus determining the formation of categories A and B.
This second
stratification into categories also has additional implications in the initial
prognostic estimate: hypothetically speaking, patients who belong to category B
of whatever class or stratum will have a less favorable prognosis than those of
category A of the same class; this supposition is more evident in the moderate
and severe classes due to the specific criteria used to classify them. This
supposition was also confirmed with the results obtained from the analysis with
a vertical direction of the instrument, that is to say, with the comparison
between categories as explained in Figure 3.
During the creation
of the initial version of the IENAC, every patient with moderate pneumonia was
included in only one stratum, but after studyÂing mortality in this group of
patients over time it was possible to identify an excessively high morÂtality
rate for the evolutionary state (not severe) at the moment of the admission.
The analysis of this situation allowed us to identify subgroups of patients
with different mortality rates but also different features, mainly related to
advanced age, radiological extension of the infectious process, the size of the
pleural effusion and specially, the presence of comorbidities24.
In the same way,
given the high mortality rate of patients with severe pneumonia, we
distinguished between two subgroups of patients whose main difference was the
probability to overcome the acute disease plus previous conditions generally
associated with functional decline and prolonged bed confinement.
In this study, the
behavior of mortality we obÂserved in patients who were initially severe and
also in those with moderate pneumonia confirms the
convenience of defining two categories of patients with different prognosis in
both classes; having verified strong differences in terms of mortality between
categories A and B of initially severe patients is our unquestionable evidence.
The authors recognize
the value of other more widely used tools such as the CURB-65 and the PSI as
instruments to establish a prognosis in paÂtients with CAP who are examined to
be hospitalÂized. Also the current use and future perspectives of other
prognostic factors such as biomarkers (procalcitonin, proadrenomedullin) are
being recognized25-30.
The results of this
research plus the ease of use and feasibility of this instrument (it only uses
clinical and radiological information) allow us to propose the IENAC as a tool
to be considered particularly in a healthcare context of limited material
resources. Thus, the IENAC becomes an alternative to set the stratification of
CAP patients in these workplace scenarios.
The robustness of the
results obtained is based on the statistical significance achieved in many of
the comparisons and also on the consistency and reproducibility of global
results in each of the case series that were part of the universe of study.
But, the lack of a comparison with other tools for the stratification of CAP
patients is considered an additional limitation. Such a comparison would have
contributed to the soundness of these results.
To conclude, the tool
for the stratification of patients with community-acquired pneumonia attending
the emergency department, called IENAC, has shown its usefulness in predicting
a favorable or unfavorable outcome at the moment of admission; thus, it becomes
a clearly valuable tool for the initial prognostic evaluation, apart from being
useful as a guide to the decision-making process related to therapeutic
behavior and management.
Also the mortality
rate behavior in the different classes and categories (strata) in which
patients can be classified through the IENAC is an imporÂtant element that
supports the purpose envisioned for this stratification instrument, in terms of
its structure and also the cirteria used for placing the patient in each
stratum.
Acknowledgement
We would like to
thank Sandy Mederos Sust, Pedro Luis Ocampo Miralles, Jorge Labrada
González, Adan Villamizar Sánchez, Erardo Labrada Ortiz, Edwin
Ojeda Rodríguez and Duniel Sánchez Medina for contributing to the
gatheÂring of information at different moments of the research.
REFERENCES
1. Saldías Peñafiel F, Gassmann
Poniachik J, Canelo López A, Díaz Patiño O.
Características clínicas de la neumonía adÂquirida en la
comunidad del adulto inmunocompetente hosÂpitalizado según el agente
causal. Rev Med
Chile. 2018; 146: 1371-83.
https://doi.org/10.4067/s0034-98872018001201371
2.
Spoorenberg SMC, Bos WJW, Heijligenberg R. Microbial aetiology, outcomes, and
costs of hospitalisation for comÂmunity-acquired pneumonia; an observational
analysis. BMC Infect Dis.
2014; 14: 335-8. https://doi.org/10.1056/NEJMra1312885
3. Longo DL, Musher
DM, Thoner AR, Debakey ME. ComÂmunity acquired pneumonia. N
Engl J Med. 2014; 371: 1619-28. https://doi.org/10.1056/NEJMra1312885
4. Falguera MF, Ramírez R.
Neumonía adquirida en la coÂmunidad. Rev Clin Esp. 2015; 215: 458-67. https://doi.org/10.1016/j.rce.2015.06.002
5. Martínez Vernaza S, Mckinley E, Soto
MJ, Gualtero S. NeuÂmonía adquirida en la comunidad: una revisión
narrativa. Univ Med.
2018; 59(4).
https://doi.org/10.11144/Javeriana.umed59-4.neum
6. Leoni D, Rello J.
Severe community-acquired pneumonia: optimal management. Curr Opin Infect Dis.
2017; 30: 240-7. https://doi.org/10.1097/QCO.0000000000000349
7. Postma DF, van
Werkhoven CH, van Elden L, Thijsen S, Hoepelman A, Kluytmans J, et al.
Antibiotic treatment strategies for community acquired pneumonia in adults. N Engl J Med. 2015; 372: 1312-23.
https://doi.org/10.1056/NEJMoa1406330
8. GBD 2015 LRI
Collaborators. Estimates of the global, regional, and national morbidity,
mortality, and aetioloÂgies of lower respiratory tract infections in 195
countries: a systematic analysis for the Global Burden of Disease Study 2015.
Lancet Infect Dis. 2017; 17: 1133-61. https://doi.org/10.1016/S1473-3099(17)30396-1
9. Bender MT,
Niederman MS. Treatment guidelines for community-acquired pneumonia. Ann Res Hosp.
2018;2:6. https://doi.org/10.21037/arh.2018.05.01
10. Ministry of Public Health. Anuario
estadístico de Salud. La Habana: Dirección Nacional de Registros
Médicos y estadísticas del Minsap; 2019. Available at:
http://bvscuba.sld.cu/anuario-estadistico-de-cuba/
11. Montero Solano G, Hernández Romero
G, Vega Chaves JC, Ramírez Cardoce M. Manejo de la neumonía
adquirida en la comunidad en el adulto mayor. Rev Cl EMed UCR. 2017; 7: 11-20.
https://doi.org/10.15517/rc_ucr-hsjd.v7i2.29141
12. Girón Ortega JA, Pérez
Galera S, Girón González JA. DiÂagnóstico y tratamiento
empírico de la neumonía adquirida en la comunidad en situaciones
especiales: pacientes inÂmunocomprometidos sin infección por el VIH y
ancianos. Medicine. 2018; 12: 3168-73. https://doi.org/10.1016/j.med.2018.03.027
13. Aleaga Hernandez YY, Serra Valdes MA,
Cordero López G. Neumonía adquirida en la comunidad: aspectos
clínicos y valoración del riesgo en ancianos hospitalizados.
Revista Cubana de Salud Pública. 2015; 41(3): 413-26.
14. Huijts SM, Boersma WG, Grobbee DE, Gruber
WC, Jansen KU, Kluytmans JW, et al. Predicting pneumococcal comÂmunity-acquired pneumonia
in the emergency department: evaluation of clinical parameters. Clin Microbiol Infect. 2014; 20:
1316-22. https://doi.org/10.1111/1469-0691.12740
15. Fine MJ, Auble
TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, et al. A
prediction rule to identify low-risk patients with community-acquired
pneumonia. N Engl J Med. 1997; 336: 243-50.
https://doi.org/10.1056/NEJM199701233360402
16. Lim WS, Van der
Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining
community acquired pneumonia severity on presentation to hospital: an interÂnational
derivation and validation study. Thorax.
2003; 58: 377-82. https://doi.org/10.1136/thorax.58.5.377
17. Torres A, Barberán J, Falguera M,
Menéndez R, Molina J, Olaechea P, et al. Guía multidisciplinar
para la valoración pronóstica, diagnóstico y tratamiento
de la neumonía adquirida en la comunidad. Med Clin (Barc). 2013; 140
(223):e1-19. https://doi.org/10.1016/j.medcli.2012.09.034
18. Julián Jiménez A,
Adán Valero I, Beteta López A, Cano Martín LM,
Fernández Rodríguez O, Rubio Díaz R, et al.
Recomendaciones para la atención del paciente con neumonía
adquirida en la comunidad en los Servicios de Urgencias. Rev Esp Quimioter
2018; 31(2): 186-202.
19. Delgado M. Uso rutinario del Pneumonia
Severity Index en el servicio de urgencias: efecto sobre los indicadores de
proceso y resultado en neumonia adquirida en la comuÂnidad. Enferm Infecc Microbiol
Clin. 2013; 31(5): 289-97. https://doi.org/10.1016/j.eimc.2012.04.012
20. Geijo M, Bermejo E, García A.
Protocolo diagnóstico y terapéutico de las neumonías
extrahospitalarias. MediÂcine. 2014; 11: 3076-80.
https://doi.org/10.1016/S0304-5412(14)70742-5
21. Noya Chaveco ME, Moya González
Noel L. Parte VII. Enfermedades del sistema respiratorio. Capítulo 31.
Neumopatías inflamatorias agudas no tuberculosas. Roca Goderich. Temas
de Medicina Interna. Tomo I. Quinta edición. 5 ed. La Habana, CU:
ECIMED, 2017. Available at:
http://bvs.sld.cu/libros_texto/roca_temas_medicina_interna_tomo1_quintaedicion/
cap31.pdf
22. Monedero MJ, Batalla M, García C,
Persiva B, Rabanaque G, Tárrega L. Tratamiento empírico de las
infeccioÂnes del adulto. FMC. 2016; 23(Supl.2):9-71.
https://doi.org/10.1016/j.fmc.2015.12.002
23. Tsilogianni Z, Grapatsas K, Vasileios L,
et al. Community-acquired pneumonia: current
data. Ann Res Hosp. 2017; 1: 25. Available at:
http://dx.doi.org/10.21037/arh.2017.05.02
24. Weir DL, Majumdar
SR, McAlister FA, Marrie TJ, Eurich DT. The impact of multimorbidity on
short-term events in patients with community-acquired pneumonia: Prospective
cohort study. Clin Microbiol Infect. 2015; 21: 264.e7-264. e13.
https://doi.org/10.1016/j.cmi.2014.11.002
25. De Jong E, Van
Oers JA, Beishuizen A. Efficacy and safety of procalcitonin guidance in
reducing the duration of anÂtibiotic treatment in critically ill patients: a
randomised, controlled, open-label trial. Lancet Infect Dis. 2016; 16: 819-27.
https://doi.org/10.1016/S1473-3099(16)00053-0
26. Alan M, Grolimund
E, Kutz A, Christ-Crain M, Thomann R, Falconnier C, et al. Clinical risk scores
and blood bioÂmarkers as predictors of long-term outcome in patients with
community-acquired pneumonia: a 6 year prospective follow-up study. J Intern Med. 2015; 278: 174-84.
https://doi.org/10.1111/joim.12341
27. Yeon Lee S, Cha
S-I, Seo H, Oh S, Choi K-J, Yoo S-S, et al. Multimarker Prognostication for
Hospitalized Patients with Community-acquired Pneumonia. Intern Med. 2016; 55: 887-93.
https://doi.org/10.2169/internalmedicine.55.5764
28. Viasus D, Del Río-Pertuz G,
Simonetti AF, García-Vidal C, Acosta Reyes J, Garavito A, et al. Biomarkers for predicting short-term mortality in
community-acquired pneumonia: A systematic review and meta-analysis. J Infect. 2016; 72: 273-82.
https://doi.org/10.1016/j.jinf.2016.01.002
29. Pereira JM, Azevedo A, Basílio C,
Mergulhão P, Paiva JA. Midregional
proadrenomedullin: An early markÂer of response in critically ill patients with
severe community acquired pneumonia? Rev Port Pneumol. 2016;
22: 308-14. Available at: https://doi.org/10.1016/j.rppnen.2016.03.012
30. Jiménez A
J, González del Castillo J, Candel F. UsefulÂness and prognostic value
of biomarkers in patients with community-acquired pneumonia in the emergency deÂpartment.
Med Clin (Barc). 2017; 148: 501-10.
https://doi. org/10.1016/j.medcle.2017.04.033