Autor : Sierra Murillo Luis Miguel1, Hernández Borge Jacinto1
1Pulmonology Service. Hospital Universitario de Badajoz. Badajoz, España
https://orcid.org/0000-0002-9463-3161
https://orcid.org/0000-0001-6694-8556
Correspondencia : Luis Miguel Sierra Murillo. Email: sierramurillolm@gmail.com
CASE REPORT
This report describes the case of a 51-year-old female,
non-smoker, without any relevant medical or surÂgical history,
who is an
information technology professor. She was referred to pulmonology consultation due to an expiratory
stridor of two months of evolution that was partially
interfering with her work, under
suspicion of possible bronchial asthma. The physical examination
only revealed said expiratory stridor. The forced
spirometry showed a flow-volume curve suggestive of
irreversible airway obstruction
with the following values: forced vital capacity (FVC) 95%, forced expiratory volume on the
first second (FEV1) 52.8% and FEV1/FVC ratio
47.23%, with negative bronchodilator test. Basing on such findings,
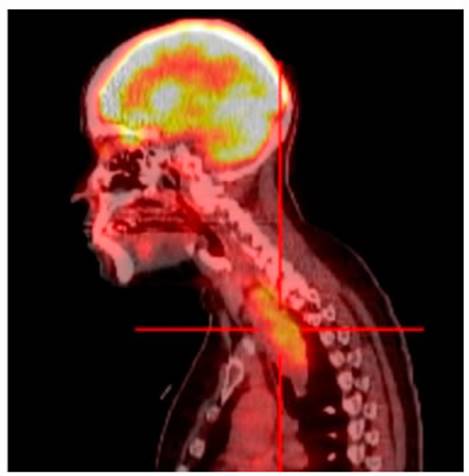
hospitalization was indicated in order to study a possible intrathoracic mass. The following imaging
tests were done: computed tomography (CT) and positron emission tomography (PET-CT), showing a large mediastinal mass (Figures 1 and 2).

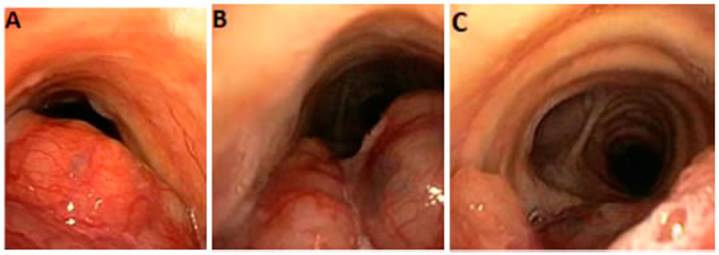
Also, a flexible bronchoscopy was performed (Figure 3), showing great damage to the tracheal pars membranosa. No samples were taken due to risk of bleeding. It was decided to do video-assisted thoÂracoscopic surgery (VATS) to obtain histological material from an area that could ensure more safety and control in case of hemorrhage.
Finally, the
diagnosis obtained was locally advanced adenoid cystic carcinoma of the trachea. CheÂmotherapy
with carboplatin and paclitaxel was indicated and completed in 3 cycles plus radiotherapy fractionated in 33 sessions. The clinical tolerance
of the patient to this treatment was adequate, and she didn’t develop
any notable complications. Approximately 5 months after finishing treatment, there was certain mass
size reduction, and it remained stable
during successive radiological controls until now, with
a length of 6 cm, anteroposterior diameter
of 2.4 cm and transverse diameter
of 2.1 cm. Also a reduction
in the 18-FDG uptake could be seen in the subsequent control PET-CT. At
present, the patient is under
close follow-up for medical oncology and radiation oncology, and the possibility of resection has been discarded.
DISCUSSION
The adenoid cystic carcinoma of the trachea is an
exceptional clinical condition; with an incidence of 0.1-0.2 cases every 100,000 inhabitants per year, it represents
the second most common primary
tracheal malignant neoplasm following the squamous cell
carcinoma1, 2.
It poses a diagnostic challenge, due to its nonspecific, insidious symptoms. The typical patient
is between 50-70 years old, no sex preference, non-smoker, and shows
progressive dyspnea in most cases. In its differential diagnosis, it is important to consider the tracheal
squamous cell carcinoma,
more common in smokers and typically ocurring in association with hemoptysis.
At
present there isn’t any agreed
standard for obtaining a confirmation diagnosis and subsequent
staging3. However, there seems to be agreement among the specialized
centers that the length of traÂcheal damage is the
variable that defines tumor resection.
For lesions larger than 5 cm, like the one
evidenced in this report, surgical treatment is not
recommened1.
Radiation therapy associated with chemotherapy is recommended in all cases, especially if there
is extracapsular extension, perineural, bronchial or vascular invasion or associated
adenopathies. 5-year overall
survival in resectable
cases is between 50-80%,
and drops to 30% in the rest of the patients1, 4, 5.
Conflicts of interests: The
authors declare no conflict
of interest in relation to the contents of this article.
REFERENCES
1.
Lilenbaum R. Malignant tracheal tumors. UpToDate, 2020. [access April 25 2021].
2.
Urdaneta AI, Yu JB, Wilson LD. Population
Based Cancer Registry Analysis of Primary Tracheal Carcinoma. Am J Clin Oncol. 2011;34:32-7.
https://doi.org/10.1097/COC.0b013e3181cae8ab
3.
Sherani K, Vakil A, Dodhia C, et al. Malignant tracheal tumors: a review of current diagnostic and management strategies. Curr Opin Pulm Med
2015, 21:322-6. https://doi.org/10.1097/MCP.0000000000000181
4.
Bhattacharyya N. Contemporary
Staging and Prognosis for Primary Tracheal Malignancies: A Population-Based Analysis. Otolaryngol Head Neck Surg. 2004;131:639-42.
https://doi.org/10.1016/j.otohns.2004.05.018
5.
Saoud M, Patil M, Singh S,
et al. Rare airway tumors: an update
on current diagnostic and management strategies. J Thorac Dis 2016;8:1922-34. https://doi.org/10.21037/jtd.2016.07.40