Autor : Gallego Claudio1 Ortega Mayra1 MĂ©ndez Ezcurra Luis1 Poropat Alejandra1 Lepek Gladys1 GarcĂa Fernández Alejandra1 AgĂĽero Silvia1 Verdugo Silvina1 Allegro Fabián1 Salomone CĂ©sar1
1Hospital General de Agudos Parmenio P. Piñero, CABA, Argentina
Correspondencia :Claudio Gallego cgallego@intramed.net
Abstract
In convalescence from the SARS-CoV-2 infection, a high number of
patients require medical consultation due to persisting symptoms.
Objective: To describe the clinical characteristics of
patients who attend the Department of Respiratory Medicine due to persisting
respiratory or thoracic symptoms after COVID-19 epidemiological discharge, and
to assess their etiology by applying a follow-up protocol.
Materials and Methods: we included patients previously
diagnosed with COVID-19 through PCR or with a combination of sympÂtoms and
epidemiological criteria who attended the Department of Respiratory Medicine
spontaneously or referred by another health professional. Clinical examination,
chest X-ray, spirometry, laboratory analysis, and the EQ-5D quality of life and
PHQ-9 depression questionnaires were performed. According to the findings, the
evaluation was complemented with D-dimer, six-minute walk test (6MWT), computed
tomography (CT) and cardiac evaluation, following a predetermined algorithm.
Mental health consultation was offered to patients with a result ≥ 10 in
the PHQ-9 questionnaire.
Results: 95 patients were included: age 48 ± 11 years,
BMI (Body Mass Index) = 28.4 ± 4.9 kg/m2,
57 (60%) women and 64 (67.5%) Argentinians. Among foreigners: 19 (20%) were
Bolivian, 8 (8.5%) Peruvian and 4 (4%) Paraguayan. 91 patients had a PCR-confirmed
diagnosis; and from the remaining patients, two had positive serology and two
clinical and epidemiological criteria. The most frequent comorbidities were:
smoking (34%), arterial hypertension (21%), diabetes (16%), asthma (11%) and
tuberculosis (5%); 38% did not refer any. 45 patients had been hospitalized,
and 8 of them required treatment in the intensive care unit (ICU). The
consultation time from epidemiological discharge was 46 ± 34 days (median = 38
days), and the most frequent symptoms were dyspnea (60%), cough (32%), chest
pain (26%), low back pain (22%) and asthenia (10.5%); 50 patients required
non-steroidal anti-inflammatory drugs (NSAIDs) for pain management. Regarding
the depression questionnaire: 79% presented PHQ-9 > 4 (mild depression) and
36% ≥ 10 (moderate and severe depression); in the latter group we found
higher prevalence in women: 44 vs. 24%, p= 0.03. We didn’t find a relationship
between depression assessed with PHQ-9 and age, nationality or isolation
location; 13 patients agreed to consult with the Department of Mental Health
(PHQ-9 14.9 ± 4; EQ-5D 39 ± 10).
In 6 patients, the spirometry showed values of forced expiratory
volume in the first second (FEV1)
and/or forced vital capacity (FVC) < 80%; they had history of pneumoconiosis
(n = 1), asthma (n = 1) and obesity (n = 1), two presented an abnormal chest
X-ray and the other one had been treated in the intensive care unit (ICU).
Additional studies were performed in 24 patients (six-minute walk test [6MWT]:
3, CT: 6, echocardiogram: 2, D-dimer: 21). Persistence of ground-glass
densities was found in 5 of the 6 tomographies. None of the patients required
an additional medical approach during follow-up.
Conclusion: In post-COVID-19 patients, the most frequent
symptoms for consultation were dyspnea, cough and chest or lumbar pain, as well
as the finding of depression assessed by a questionnaire. The results favor the
holistic approach in the evaluation and follow-up of these cases.
Key words: SARS-CoV-2, Post-COVID-19 syndrome, Post-acute
COVID-19, Post-COVID follow-up
Received: 02/11/2021
Accepted: 07/20/2021
In 2020 the world has suffered a pandemic caused by the SARS-CoV-2
which affected more than 80 million people –considering only confirmed cases–
and resulting in more than 1.5 million deaths. At the beginning of January 2021
there were in Argentina more than 1.5 million cases
and approximately 40,000 deaths. During the follow-up of those patients, it
could be observed that around 10% of recovered individuals show prolonged
symptoms after having the disease1.
These patients are described with the expression post-acute COVID-19 and
generate a high demand of consultations with the health system, which is also
under the pressure of receiving new cases.
This situation repeated itself in different parts of the world and
resulted in the development of local guides with algorithms for cost-effective
management of these patients1, 2,
facilitating the isolation of those with respiratory or cardiac complications
that require strict and specialized follow-up. Some of the severe
manifestations of COVID-19 that stand out are: lung parenchymal involvement3, damage of the
microvasculature with thrombosis-associated risk and myocardial involvement4. However, most patients
who attend the consultation after the acute phase present prolonged nonspecific
symptoms that will gradually improve within weeks or a few months without
showing medium-term or probably long-term sequelae.
This work intends to describe the clinical characteristics of
patients categorized as post-acute COÂVID-19 for persisting with respiratory
symptoms after the epidemiological discharge, using an algorithm based on the
previously mentioned guides.
Materials
and Methods
The prospective descriptive cohort was developed in the Hospital
General de Agudos Parmenio Piñero between October and December, 2020 and
was approved by the Independent Ethics Committee of the Hospital General de
Agudos Dr. Teodoro Álvarez (CR 3766).
All the patients who had attended the Department of Respiratory
Medicine spontaneously or referred by another health professional with
persistent respiratory or thoracic symptoms after the COVID-19 epidemiological
discharge entered the study in a consecutive manner. All the patients had been
previously diagnosed through polymerase chain reaction (PCR), but the study
also admitted patients who fulfilled epidemiological criteria (person cohabiting
with a confirmed case) with a history of clinical condition compatible with
SARS-CoV-2 infection. We excluded patients previously diagnosed with
respiratory or cardiovascular sequelae related to this disease. The patients
underwent a clinical examination (quesÂtions about current symptoms, medical
record and physical examination), chest X-ray, pulse oximetry, spirometry,
laboratory analyses (hemogram, erythrocyte sedimentation, glycemia, ionogram,
hepatogam, urea and creatinine) and answered the EQ-5D quality of life and
PHQ-9 depression questionnaires.
On the basis of the results obtained in the initial evaluation we
applied a follow-up algorithm that is shown in Figure 1. Patients with
dyspnea or chest pain in whom it was considered necessary to dismiss the
cardiovascular origin of the symptoms we included determination of D-dimer
through laboratory tests. If the clinical examination or the result of the
D-dimer test justified a cardiac evaluation, the study would be completed with
the six-minute walk test (6MWT), an echocardiogram and an evaluaÂtion performed
by a specialist.
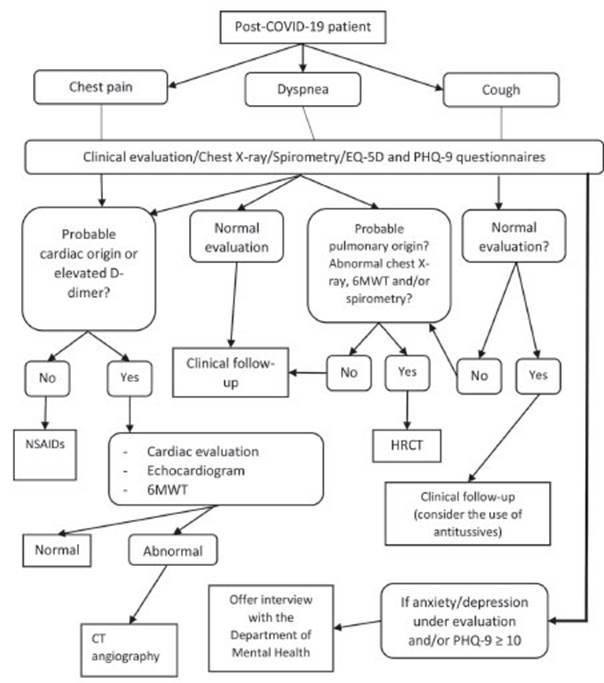
If the origin of the chest pain was determined to be
musculoskeletal, they would be prescribed NSAIDs. We randomly administered 75
mg of diclofenac by oral route (OR) every 12 hours or 10 mg of ketorolac by OR
every 8 hours, as available.
Patients with cough or dyspnea of presumed respiratory origin or
with alterations in the spirometry or chest X-ray completed their evaluation
with the 6MWT and computed tomography (CT), depending on the findings. The use
of antitussives in an individualized manner was considered.
The initial evaluation included two questionnaires:
1. EQ-5D health questionnaire (Spanish version)5:
designed to be self-administered, this questionnaire evaluates the patient’s
health condition through 5 questions that refer to: mobility, self-care, daily
activities, presence of pain or discomfort and anxiety or depression. It is
complemented by a visual analog scale in which the patient makes a mark between
zero (the worst imaginable health condiÂtion) and 100 (the best) in order to
indicate the situation he/she is going through at the moment of the
consultation.
2. PHQ-9 depression questionnaire6,
7: includes 9 items that evaluate the presence of symptoms of
depression (that correspond to the DSM-IV criteria) in the last two weeks. The
patient classifies the answer to each item according to its severity, for
example: 0 = “never”, 1 = “some days”, 2 = “more than half the time” and 3 =
“almost every day”. Those values are summed up and a score is obtained which
categorizes the degree of depression: 0-4 without evidence, 5-9 mild, 10-14
moderate, 15-19 moderately severe, 20-27 severe. All patients with values
≥ 10 (compatible with moderate or severe depression) or with values <
10 but whose clinical evaluation suggests significant alterations in the
emotional sphere were offered an evaluation with the hospital’s Department of
Mental Health.
The respiratory function exploration was performed according to
the guidelines of the ATS/ERS (American Thoracic Society/European Respiratory
Society)8 through a MIR Spirobank
II spirometer. The 6MWT was done basing on the guidelines of the ATS9 with NONIN 8500M equipment.
Data obtained were analyzed with descriptive statistics tools. The
Chi-Square Test was used for the qualitative variables
(https://www.socscistatistics.com) and the Student t Test was used for the
quantitative variables in the comparison between groups (Excel 2016),
considering a value of p<0.05 as significant.
Results
95 patients were included in the study, 91 of which had confirmed
diagnosis of COVID-19 through PCR. Within the remaining patients, apart from
having a compatible clinical condition, two had positive serology and two
fulfilled epidemiological criteria.
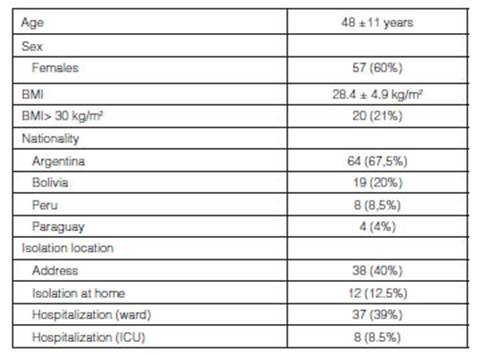
Table 1 shows the demographic characteristics and isolation
location throughout the course of the disease. It is worth mentioning that more
than half of the patients came from their homes or a hotel adapted to fit the
needs to care for isolated individuals; and among hospitalized patients (n=45):
39 (87%) required oxygen and 6 (13%) needed mechanical respiratory assistance.
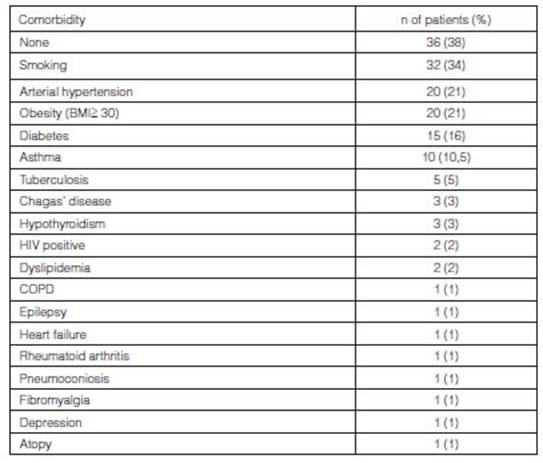
The most frequent comorbidities were: smoking (34%), arterial
hypertension (21%), diabetes (16%), asthma (11%) and tuberculosis (5%); 38% did
not refer any (Table 2).
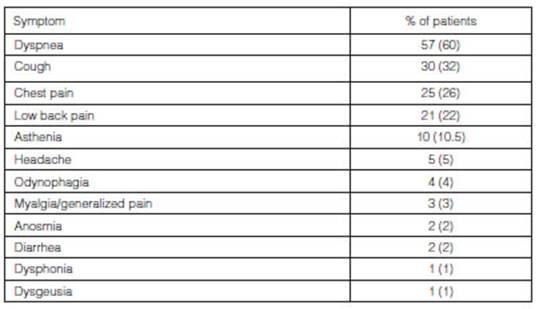
The time to make a consultation since epidemiological discharge
was 46 ± 34 days (median= 38 days), or 63 ± 36 days (median = 55 days) if we
take into account the time since the onset of COVID-19 symptoms. The most
common symptoms which motivated the patients to make a post-COVID-19 conÂsultation
were: dyspnea (60%), cough (32%), chest pain, mostly described as oppressive
and sporadic (26%), low back pain (22%) and asthenia (10.5%) (Table 3); 50
patients required NSAIDs for chest or lumbar pain of musculoskeletal origin.
Regarding the studies carried out in the initial consultation, in
6 patients the spirometry showed values of forced expiratory volume in the
first second (FEV1)
and/or forced vital capacity (FVC) < 80%; they had history of pneumoconiosis
(n = 1), asthma (n = 1) and obesity (BMI > 30 kg/m2 (n = 1), two presented an
abnormal chest X-ray and the other one had been treated in the intensive care
unit (ICU). None of them required specific treatment related to COVID-19. Only
6 patients had SpO2 <
95%, with 92% as the lowest.
Additional individualized studies were done in 24 patients, basing
on their clinical evaluation: 6MWT: 3, CT: 6, echocardiogram: 2, D-dimer: 21.
Persistence of ground-glass densities was found in 5 of the 6 tomographies.
They were considered as lesions in the process of resolution of pneumonia
caused by SARS-CoV-2. D-dimer continued to be high in 4 patients (> 500)
without active cardiac findings to justify it. None of the patients required an
additional medical approach during follow-up.
Regarding the depression questionnaire: 79% presented PHQ-9 > 4
(mild depression) and 36% ≥ 10 (moderate and severe depression); in the
latter group we found higher prevalence in women compared to men: 25 of 57
(44%) vs. 9 of 38 (24%), p = 0.03. We didn’t find any relationship between
depression assessed with the PHQ-9 questionnaire and age, nationality or
isolation location. Patients with PHQ-9 ≥ 10 were offered an interview
with the staff of the Department of Mental Health of the hospital. 13 patients
(38%) agreed: PHQ-9 14.9 ± 4 and a quality-of-life value calculated by means of
the EQ-5D scale of 39 ± 10. When we compared both questionnaires (the EQ-5D was
answered completely by 84 patients), we found a weak inverse correlation
between the value obtained through the PHQ-9 and the visual analog scale of the
EQ-5D (r=0.37). However, the answer to the question that identifies patients
with self-perceived anxiety or depression, “I’m not anxious or depressed”, of
the EQ-5D divided the group that didn’t show evidence of depression, either,
through the PHG-9: out of 26 patients without self-perceived anxiety/depression
in the EQ-5D, 22 (85%) had PHQ-9 < 10.
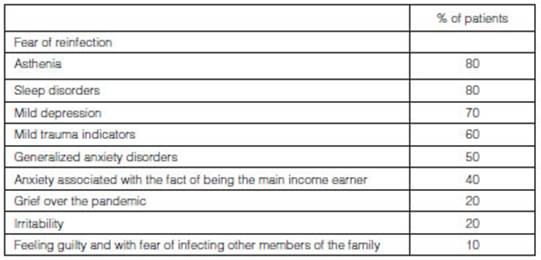
At the end of the study, we obtained feedback from the Department
of Mental Health about the 12 patients who participated (one patient had
accepted the invitation but didn’t show up). The main findÂings were: fear of
reinfection, asthenia, sleep disorders and mild depression (Table 4).
On the other hand, around one third (36 individuals) of the
patients made the first visit and unÂderwent initial studies only. These
patients didn’t show evidence of significant pathologic findings and didn’t
return to the final visit. Those who completed the follow-up visits and
answered a PHQ-9 questionnaire during the final visit showed a significant
decrease in the depression markers assessed by the PHQ-9 questionnaire:
baseline 7.8 ± 6 vs. final 3.6 ± 4 (p < 0.001).
Discussion
The most common reasons for consultation of the group of patients
who had attended the Department of Respiratory Medicine with persistent
symptoms post-acute phase of COVID-19 were: dyspnea, cough, chest pain, low
back pain and asthenia. The psychological burden associated with recovery from
a disease was assessed by means of a depression questionnaire that showed
significant alterations in the mental health sphere in more than one third of
the patients. On the other hand, we didn’t find any significant organic changes
that could explain the symptoms or psychological alterations. This agrees with
the approach described in various guidelines1,2,13 that indicate the need to use a
holistic approach in these patients.
Our study included a population with predominance of mild and
moderate forms of acute COVID-19 over the severe ones, with a mean age slightly
lower than other series10,11 and with greater representaÂtion
of tuberculosis among the comorbidities12.
Symptoms such as dyspnea, cough, asthenia and pain (chest pain or generalized
pain, such as myalgia or arthralgia) are described in all the reports. The
presence of low back pain not related to the isolation location stands out in
our series, but we can’t describe it as a result of prolonged decubitus
position and we can’t establish a causal relationship with the infection,
either.
We set a follow-up protocol in order to identify which patients
are at risk of having cardiac or respiraÂtory sequelae with a clinical
evaluation and low complexity tests (chest X-ray, spirometry, 6MWT and
D-dimer), confirming such sequelae through tests with higher diagnostic specificity,
as for example echocardiogram and CT. None of the patients assessed with this
algorithm showed significant alteraÂtions. A high proportion of patients who
obtained normal results didn’t return for follow-up. We think the reason for
this could be the spontaneous favorable evolution as well as reduced patient
anxiety, but since they didn’t make a subsequent follow-up phone call we can’t
confirm this idea, and this means there is a weakness in the design of the
study in terms of follow-up.
In the patient’s evaluation we included the EQ-5D quality of life
questionnaire and also the one related to depression, the PHQ-9. There are some
studies about psychological disorders in health workÂers who participated in
COVID patients care14,
but this evaluation was not commonly conducted with patients. It is true that
physical manifestations associated with COVID may distort answers to this
questionnaire13,
but physicians not specialized in the diagnosis of mental health diseases could
use it and so it turned out to be a practical way to identify patients with
psychological alterations that could benefit from mental healthcare. The
questionnaire showed elevated numbers that suggest depression in any of its
degrees in most patients. 36% of the population under evaluation showed very
elevated results compatible with moderate or severe depression. In that group
there was higher prevalence of women, in accordance with the gender differences
established in multiple research studies15.
This group of patients were offered a consultation with the Department of
Mental Health, and it was accepted by approximately one third. Whereas the
EQ-5D question assessing anxiety/depression was useful to exclude individuals
who didn’t need a mental health care consultation, the PHQ-9 facilitated the
identification of a subgroup defined as “patients at risk of suffering from
significant depression”, for whom such consultation was in fact necessary.
To conclude, in the group of post-COVID-19 patients who developed
the disease mostly without requiring intensive care the most common symptoms
for consultation were: dyspnea, cough and chest or lumbar pain, without an
organic correlate requiring other actions beyond symptomatic treatment.
Depression assessed through a questionnaire was also common. The results favor
the holistic approach in the evaluation and follow-up of these patients.
References
1. Greenhalgh T, Knight M, A’Court C, et al. Management of
post-acute covid-19 in primary care. BMJ 2020;370:m3026. https:// doi.org/10.1136/bmj.m3026
2. Sibila O, Molina-Molina M, Valenzuela C, et al. Documento de
consenso de la Sociedad Española de Neumología y Cirugía
Torácica (SEPAR) para el seguimiento clínico post-COVID-19. Open
Respiratory Archives. https://doi.org/10.1016/j.opreÂsp.2020.09.002
3. Borczuk AC, Salvatore SP, Seshan SV, et al. COVID-19 pulmonary
pathology: a multi-institutional autopsy cohort from Italy and New York City.
Mod Pathol 2020; 33: 2156–68. https://doi.org/10.1038/s41379-020-00661-1
4. Lowenstein C, Solomon S. Severe COVID-19 is a Microvascular
Disease. https://doi.org/10.1161/CIRCULATIONAHA.120.050354
5. Cabasés JM. El EQ-5D como medida de resultados en salud.
Gac Sanit 2015; 29: 6. http://dx.doi.org/10.1016/j.gaceta.2015.08.007
6. Kroenke K, Spitzer R, Williams J. The PHQ-9 Validity of a Brief
Depression Severity Measure. J Gen Intern Med 2001; 16: 606-13. 368 369
Post-COVID-19 syndrome
7. Baader T, Molina JL, Venezian S, et al. Validación y
utilidad de la encuesta PHQ-9 (Patient Health Questionnaire) en el
diagnóstico de depresión en pacientes usuarios de atención
primaria en Chile. REV CHIL NEURO-PSIQUIAT 2012; 50: 10-22.
8. Graham BL, Steenbruggen I, Miller M, et al. Standardization of
Spirometry 2019 Update. An Official American Thoracic Society and European
Respiratory Society Technical Statement. Am J Respir Crit Care Med. 2019; 200:
e70.
9. ATS statement: guidelines for the six-minute walk test. Am J
RespirCrit Care Med 2002; 166: 111-7
10. Tenforde M, Kim S, Lindsell C, et al. Symptom duration and
risk factors for delayed return to usual health among outpatients with COVID-19
in a multistate health care systems network. MMWR 2020; 69, July 24.
11. Carfi A, Bernabei R, Landi F. Persistent symptoms in patients
after acute COVID-19. JAMA 2020; 324: 6. http://dx.doi.
org/10.1001/jama.2020.12603
12. Richardson S, Hirsch J, Narasimhan M, et al. Presenting
characteristics, comorbidities, and outcomes among 5700 patients hospitalized
with COVID-19 in the NewYork City area. JAMA 2020; 323(20): 2052-9.
http://dx.doi.org/10.1001/jama.2020.677
13. Greenhalgh T, Knight M, A’Court C, et al. Management of
post-acute covid-19 in primary care. BMJ 2020;370:m3026. http://
dx.doi.org/10.1136/bmj.m3026
14. Azoulay E, Cariou A, Bruneel F, et al. Symptoms of Anxiety,
Depression, and Peritraumatic Dissociation in Critical Care Clinicians Managing
Patients with COVID-19. Am J Respir Crit Care Med 2020; 20: 1388-98.
15. Vázquez Machado A. Depresión, diferencias de
género. Multimed 2013; 17: 1-21.