Autor : Freire Figueroa Francisco1, MarĂn Navarro Viviana1, Poblete Figueroa Christian1, Montt Garrido Roberto2
1 Physiotherapist, Hospital at Home, Dr. SĂłtero del RĂo Care Complex, South East Metropolitan Health Service, Cordillera Province. Santiago de Chile 2 Physiotherapist/Veterinarian, National Fishery and Aquaculture Service, ValparaĂso Province, Chile
Correspondencia :f.freire.figueroa@gmail.com
Abstract
Introduction: Hospital at Home (HAH) is considered an extremely important service, showing great efficacy in the treatment of respiratory diseases.
Objectives: To evaluate the effects of high-flow nasal cannulas (HFNCs), describe the experience of patients treated with this therapy as HC and propose a protocol that standardizes the use of this equipment in the context of acute respiratory diseases as home care.
Materials and Methods: This was done by means of a quasi-experimental study with patients admitted to HAH between May and September 2019. For the statistical analysis we used Minitab 17.0.
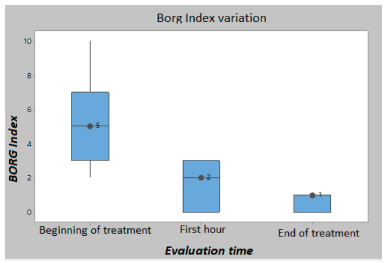
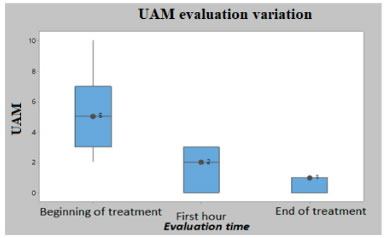
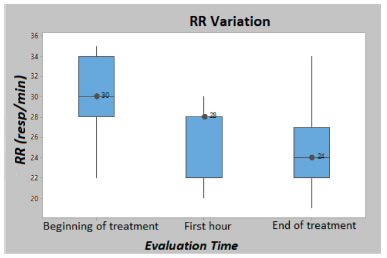
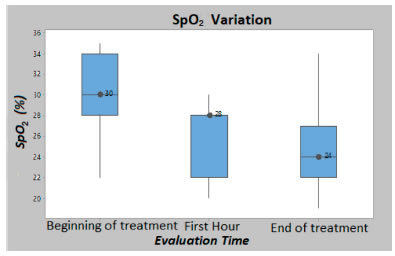
Results: 11 subjects met the inclusion criteria, with a mean age of 73 ± 7.8 years. 100% of them (N = 11) had been referred from the emergency service with oxygen requirements. 73.2% (N = 8) were admitted with diseases classified as J15 and J44; 18.1% (N = 2) had diagnosis code J84 and 9% (N = 1) had diagnosis code J46, according to the ICD-10 (International Classification of Diseases- Tenth Edition). The mean duration of the HFNC connection was 7.5 ± 5.1 days. We used a mean flow of 35 ± 5.2 L/min, FiO2 of 33 ± 6.1% and a temperature of 32.3 ± 5.1 Degrees Celsius (°C). The clinical signs with statistically significant changes were (Kruskal Wallis, p < 0.05) the BORG Scale, UAM, RR and the SAFI Index. The SpO2 and HR didn’t show statistically significant differences.
Conclusion: Despite the fact that the number of patients under treatment was low, there are potentially significant effects in parameters of relevance for this type of diseases, and this may serve as a basis for future studies.
Key words: Hospital at Home; Respiratory kinesiology; Respiratory physiotherapy, High-flow nasal cannula.
Introduction
The lung is a vital organ of our respiratory system, vulnerable to lesions due to constant exposure to particle pollution in the air and infectious organisms. Respiratory diseases are one of the main causes of death and disability in the world, generating an enormous healthcare burden at world level. One of the most prevalent diseases is the Chronic Obstructive Pulmonary Disease (COPD), which is the third cause of death in the world1, 2.
COPD prevalence varies depending on each country, but it is estimated that 35 out of 1,000 hospitalizations in Latin America are due to COPD exacerbations, with ranges of inhospital mortality that vary from 6.7% to 29.5% generating an estimated cost of 909.5 euros per year per patient3, 4. Another group of diseases that generate high costs and a high number of hospitalizations worldwide are the infections of the lower airways, the fourth cause of death2, 5. In Chile, these diseases have low mortality in ambulatory patients (less than 1.5%); however, the mortality of users requiring hospitalization may reach 10% to 25%, being a problem of Public Health and also generating an enormous economic
cost6. In Chile, the Department of Statistics and Health Information (DEIS, according to its acronym in Spanish) reported 1842 deaths for this cause in 1990 (ratio of 14/105), and 3251 deaths in 2010, with a ratio of 36.08/100,000 inhabitants7.
Hospital at Home (HAH) is positioned as an extremely important service, showing great efficacy in the treatment of this type of diseases4, 6. Also, even though the economic impact of HAH is still under discussion, there is evidence that it entails the saving of significant resources related to these diseases8, 9.
Apart from contributing to the economic sphere, many experts consider HAH as beneficial for the management of patients with acute respiratory diseases, since it avoids the possibility of getting infections associated with healthcare assistance, improves the efficacy of treatments such as oxygen therapy, mechanical ventilation and home rehabilitation, and fosters adherence to chronic treatments4, among other benefits of HAH itself6.
Since it was first used, the complexity of HAH has been continuously developing, basing on the use of different technological resources with the purpose of avoiding the readmission of the patient to traditional hospitalization, thus increasing its resolution capacity. One of these resources is the high-flow nasal cannula (HFNC), used for the treatment of respiratory decompensation at home.
Various benefits associated with HFNC treatment have been reported, as for example, increased oxygenation, reduction in dead space, improvement of the ventilatory and hemodynamic pattern, reduction in work of breathing and metabolic cost of gas conditioning, better lung volumes and greater comfort for the patient10-13. The majority of the evidence is based on studies carried out with neonate and paediatric subjects; the volume of studies with adults is lower, and those have been conducted mostly in emergency care services and Units of Critically Patients UCP14. These services have used HFNC treatment for a variety of patients with various diseases and underlying conditions such as: hypoxemic respiratory failure, acute COPD exacerbation, postextubation, oxygenation before intubation, sleep apnea, acute respiratory failure, among other conditions15. On the other hand, it is important to indicate that most evidence compares HFNC treatment with noninvasive mechanical ventilation (NIMV) or traditional high-flow oxygen therapy in patients with moderate to severe respiratory failure16, 17.
Information regarding the use of protocols for HFNC is limited, but there is a study conducted by the Ischaki group et al in patients with acute hypoxemia of almost any cause18, and there is also another study that is being carried out by the group of Kim et al comparing the use of three different protocols for the use of this therapy19, all of this within the inhospital sphere of the UCP.
When analyzing the use of this therapy within the home context, the available evidence focuses mainly on the treatment of patients with stable chronic respiratory diseases, obtaining results such as reduced number of exacerbations and episodes of hospitalization20, 21, stimulation of mucociliary clearance22, reduction of stable hypercapnia23 and optimization of the postsurgical process of patients with chronic respiratory disease24.
Objectives
To evaluate the effects of the high-flow nasal cannula (HFNC), describe and define the type of patient treated with this therapy as HAH and propose a protocol that standardizes the use of this equipment in the context of an acute respiratory disease.
Materials and methods
Quasi-experimental study of patients admitted to the Unit of Home Care (UHC) of the Dr. Sótero del Río Care Complex who met the inclusion criteria and underwent HFNC therapy from May to September, 2019. We used the Minitab 17.0 for the statistical analysis.
Inclusion criteria
• 18 years or older.
• Medical indication for respiratory kinesiology.
• Not life-threatening acute respiratory failure.
• Hemodynamically stable, understanding the hemodynamic instability as a heart rate (HR) of more than 140 beats per minute and/or a 20% change in basal and/or systolic pressure of more than 180 mmhg or less than 90 mmhg and/or a decrease of more than 40 mmhg in the basal values18.
• SAFI (oxygen saturation [SpO2] / fraction of inspired O2 [FIO2]) of more than 200.
• Social worker evaluation of the HAH, ensuring that the patient has a tutor that is responsible for him/her, and a home that is appropriate for his/her treatment, with basic hygiene services, stable power connection and drinkable water.
Exclusion Criteria
• Bad adherence to the indications.
• History of bad tolerance to therapy.
• Need for more than 5 liters of oxygen per minute.
• Use of invasive mechanical ventilation (IMV) or noninvasive mechanical ventilation (NIMV).
• Diseases and/or malformations compromising the upper airway.
• Cognitive impairment that doesn’t allow the patient to follow indications.
• Neuromuscular disease.
• Unstable or unresolved cardiopathy.
• Voluntary rejection to therapy.
Beginning of HFNC therapy in a user with acute respiratory failure.
The FiO2 used by the user at the moment of the home visit will be kept the same, plus 60 L/min of airflow with a temperature of 34 °C.
• Taking into account that a maximum FiO2 of 60%, equals 5 L/min of oxygen with 10 L/min of airflow or a minimum FiO2 of 28% that corresponds to 5 L/min of oxygen with 60 L/min of airflow.
• Increase the FiO2 until reaching a minimum SpO2 of 90% measured with pulse oximeter or the normal (basal) SpO2 of the user in case it is lower than 90%, measured with pulse oximeter.
• Change parameters and evaluate according to the clinical response and well-being of the patient.
• Use the HFNC for at least 4 hours, then evaluate according to clinical signs, continuity or decrease in the initially set parameters.
• Ask for arterial blood gas (ABG) if the user shows any clinical sign of hypercapnia, such as nausea, vomiting, confusion and generalized weakness.
Weaning Protocol
• Reduce flow to 10 L/min every day and evaluate response until reaching a minimum of 15 L/min and 40% FiO2 that equals 4 L/min of oxygen or lower, with stable vital signs.
• Use a Venturi or nose mask, as needed. Continue with the normal protocol of progressive removal of oxygen.
Criteria for Interrupting the procedure
• Unfavorable response within the first hour of clinical evolution, evaluated with vital signs and/or worsening of respiratory failure, according to the classification. In this case, the user must be referred to the emergency care services.
• If the patient shows symptoms of hypercapnic encephalopathy such as nausea, vomiting, cephalea, disorientation, weakness, convulsions, asterixis, memory loss and/or sleep disorders. Request ABG exam, consider referral to emergency services and remove from research protocol.
• Voluntary interruption of treatment requested by user.
Registration
Every user was registered at the beginning of treatment, one hour later, and in each visit on a page designed for that purpose (Figure 1) specifying the following information: personal data, clinical signs related to a sensation of dyspnea (modified BORG scale), use of accessory muscles (UAM), heart rate (HH), respiratory rate (RR), SpO2, arterial pressure (AP) and SAFI, set parameters of flow, FiO2 and temperature in Celsius degrees (°C), ABG exam if needed, observations related to possible complications and/or positive or negative manifestations of the users and/or caretakers regarding the use of the equipment.

Results
User Characteristics
11 users met the inclusion criteria. 64% (N = 7) were female and 36% (N = 4) were male. The mean age was 73 ± 7.8 years. Regarding the geographical location of the users’ place of residence, 100% (N = 11) belonged to the Puente Alto Commune; and 100% (N = 11) of health prevision was responsibility of the National Health Fund (FONASA, for its acronym in Spanish), category B. As regards the formal educational level, 91% (N = 10) had a basic level and 8% (N = 1) had medium level.
100% (N = 11) of subjects were referred with O2 requirements from the emergency services of the Dr. Sótero del Río Care Complex (CASR), located in the Puente Alto Commune, Santiago de Chile. 18% (N = 2) of all the registered users had to be referred to the emergency services from their homes because HNFC therapy couldn’t stabilize the exacerbation.
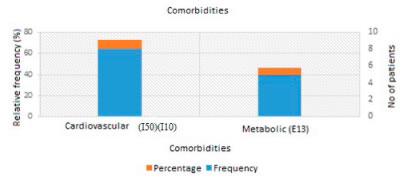
Medical diagnosis upon admission and comorbidities were classified according to the International Classification of Diseases (ICD-10)25. These are detailed in Figure 2 for the main diagnosis and Figure 3 for comorbidities.
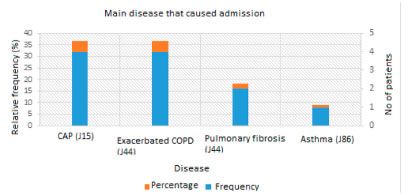
73.2% (N = 8) of users were admitted with main diseases classified as J15 and J44, these being bacterial pneumonia and exacerbated COPD; 18.1% (N = 2) were admitted with a diagnosis classified as J84, and 9% (N = 1) with J46, which corresponded to exacerbated pulmonary fibrosis and asthma attack.
Comorbidities were classified in I50, I10 and E13, which correspond to congestive heart failure, arterial hypertension and diabetes mellitus type II, respectively. We calculated the Charlson Index26 of all users, obtaining as a result an average of 4.8 ± 1.2 points and a 10-year survival percentage of 29.7%.
Intervention
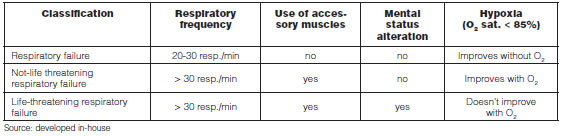
All the users received medical assistance, pharmacologic and kinesiological treatment during their stay, without exception. If the users suffered a respiratory exacerbation, they were classified according to the criteria in Table 1. Classification adapted by the authors according to the needs of HAH, using the 2019 GOLD initiative as reference27. 90.9% (N = 10) of users were classified as not-life threatening respiratory failure and 9.1% (N = 1) as respiratory failure.
The average number of days of HFNC connection was 7.5 ± 5.1 days, and 100% of the users had medium-sized cannulas. On average, we used a flow of 35 ± 5.2 L/min, FiO2 of 33± 6.1% and a temperature of 32.3 ± 5.1 Celsius degrees (°C).
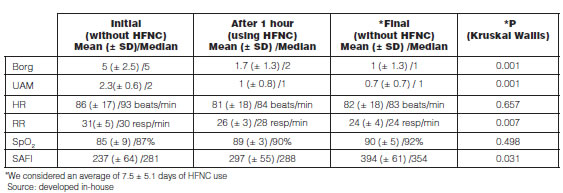
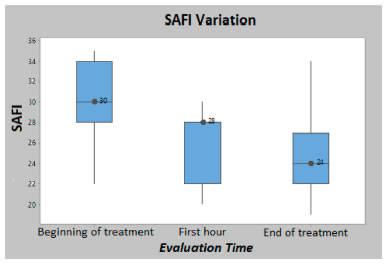
The clinical signs that showed statistically significant changes (Kruskal Wallis, p < 0.05) from the beginning of the connection until the final disconnection were: BORG Scale score, RR, SAFI Index and UAM, which was assigned a score according to severity, for example: 0 points for no use of accessory muscles, 2 points for use of supraclavicular muscles and 3 points for use of abdominal muscles. The SpO2 and HR didn’t show statistically significant differences. Detailed information is shown in Table 2. Figure 4 and Figure 5 show the mean evolution of respiratory distress clinical signs (UAM, BORG and RR); and Figures 6 and 7 show the clinical signs of hypoxia (SpO2 and SAFI).
With regard to qualitative findings, every user answered the following questions in each visit: What difference can you find with the new therapy compared to the conventional kinesiological therapy performed before HFNC connection? Do you find the used parameters comfortable? Do you think it is important to discuss any other aspect related to the HFNC? Table 3 shows the comments and observations, both positive and negative, of users and their caretakers.
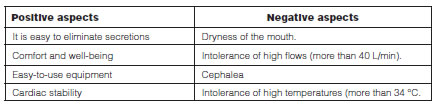
At first, none of the users tolerated high flows (> 40 L/min) or temperatures of more than 34°C, also, 25% (N = 2) of users indicated dryness of the mouth and cephalea during connection to HFNC. As regards the positive aspects, 100% of users (N = 11) claimed it was an easy-to-use equipment; 81.8% (N = 9) indicated that it was easier for them to eliminate bronchial secretions; 63.6 % (N = 7) claimed to be in a state of relaxation and well-being and, finally, 18.2 % (N = 2) said they felt less agitated or had less tachycardia symptoms.
Discussion
Users connected to HFNC were 11 adults with an acute respiratory pathological process (pneumonia) and/or exacerbations of their chronic diseases (COPD and asthma) with an average Charlson Index of 4.8 points and a survival of 29.7% after 10 years, somewhat evidencing the complexity of users admitted to HC.
Users who failed did it within the first hours of use, as opposed to the literature that indicates failure within the first 60 to 120 minutes18; thus, it is important to consider surveillance within the first hour in order to evaluate the evolution of the patient in case he/she needs another alternative treatment or, eventually, the referral to the emergency service. Nevertheless, considering the fact that the protocol was based on existing evidence, which is mostly from emergency or critical care units, the favourable evaluation of patients under observation in this research was 81.8% (N = 9). The main signs of respiratory complication showed positive changes, both clinically and statistically significant, turning this experience into a beneficial one for this group of users.
As regards the proposed protocol, we believe it should be modified for the context of HAH, since none of the users tolerated 60 L/min at the beginning of therapy, and both the connection and weaning from HFNC therapy shall be guided according to the objectives and benefits to be obtained with HFNC.
We think that one of the most important clinical signs for starting the treatment or referring the patient to the emergency services from their home is mental state, followed by the signs of breathing effort (RR and UAM). Also, the SAFI Index28 turned out to be a very useful tool for measuring the severity of pulmonary compromise in cases of HAH, since it is possible to make decisions in an adequate manner always taking into account the basal condition of the user. This experience showed a favourable evolution from a mild-moderate pulmonary compromise to normal after 7.5 ± 5.1 days of use.
We believe the qualitative benefits of this therapy are important for HAH, mainly those that make reference to easy-to-use equipment, comfort and well-being, allowing for the safe management of the equipment by the patient’s family and caretakers and reducing risks in equipment handling. Also, the kinesiological therapy focused on the permeabilization of the airway, it is positively affected, given the benefits of humidification and the temperature delivered by the equipment.
Some of the limitations of this study are: the limited size of the sample, the evaluation of the HFNC experience in only one Center, the heterogeneity of connected patients, the subjectivity of the HFNC connection criteria and the lack of a scale that measures the breathing difficulty transversally validated and applied to all users. However, the results we obtained allowed for detecting the potential beneficial effects of HFNC regarding important parameters for mild to moderate acute respiratory diseases, which will hopefully be useful for future studies.
Conclusion
This study has made a small-scale evaluation of some of the effects of the HFNC as HAH for the treatment of users with mild to moderate acute respiratory diseases. The number of treated patients was low, but there are potentially significant effects as relevance parameters for this type of diseases, and this may be useful for future studies about the beneficial effects of HFNC, a tool to be taken into account for the treatment of this type of diseases in an area that has been growing during the last years.
1. Foro de las Sociedades Respiratorias Internacionales. El impacto global de la Enfermedad Respiratoria – Segunda edición. México, Asociación Latinoamericana de Tórax, 2017.
2. World Health Organization. Top 10 causes of death [web] Geneva: WHO; 2018. [cited on January 30, 2020]. Global Health Observatory (GHO) data. Available at: http://www.who.int/gho/mortality_burden_disease/causes_death/top_10/en/
3. Ciappini A, Alison L, Agustina M, Demian G, Silvana C, Edgardo S. The epidemiology and burden of COPD in Latin America and the Caribbean: systematic review and meta-analysis. Copd 2014; 11: 339-50.
4. Ruiz-Sada P, Esquillor-Rodrigo M J, Palacios-García L, Iguzquiza-Pellejero M J, Oroz-Segura I, Resano García I. Estudio comparativo entre pacientes EPOC ingresados en hospitalización a domicilio y hospitalización convencional. Hosp Domic. 2017; 1(4): 189-97.
5. Bernal Aguirre C, Carvajal Sierra H, Alvis-Zakzuk NJ. Costos económicos de la infección respiratoria aguda en un Municipio de Colombia. Rev Univ Ind Santander Salud. 2017; 49(3): 470-7.
6. Freire Figueroa F, Marín Navarro V. Descripción e impacto económico de los pacientes con patologías respiratorias ingresados con indicación de kinesiología en la Unidad de Hospitalización Domiciliaria del Hospital Dr. Sótero del Río. Hosp Domic. 2019; 3(4): 243-54.
7. Guía Clínica Enfermedad Pulmonar Obstructiva Crónica de tratamiento ambulatorio. Santiago de Chile, MINSAL, 2013
8. Caplan GA, Sulaiman NS, Mangin DA, Aimonino Ricauda N, Wilson AD, Barclay L. A Meta-analysis of hospital in the home. Med J Aust. 2012; 197(9): 512-9.
9. Levine DM, Ouchi K, Blanchfield B, et al. Hospital-Level Care at Home for Acutely in adults: A Randomized Controlled Trial. Ann Intern Med. 2020; 172: 77-85. [Epub ahead of print 17 December 2019].
10. Mauri T, Turrini C, Eronia N, Grasselli G, Volta CA, Bellani G, Pesenti A Physiologic Effects of High Flow Nasal Cannula in Acute Hypoxemic Respiratory Failure. Am J Respir Crit Care Med. 2017; 195(9): 1207-15.
11. Drake MG. High-Flow Nasal Cannula Oxygen in Adults: An Evidence-based Assessment. Ann Am Thorac Soc.2018; 15(2): 145-55.
12. Möller W, Feng S, Domanski U, Franke KJ, Celik G, Bartenstein P, Becker S, Meyer G, Schmid O, Eickelberg O, Tatkov S, Nilius G. Nasal high flow reduces dead space. 2017; 122(1): 191-7.
13. Okuda M, Kashio M, Tanaka N, Matsumoto T, Ishihara S, Nozoe T, Fujii T, Okuda Y, Kawahara T, Miyata K. Nasal high-flow oxygen therapy system for improving sleep-related hypoventilation in chronic obstructive pulmonary disease: a case report. J Med Case Rep. 2014; 13: 341.
14. Lenglet H, Sztrymf B, Leroy C, Brun P, Dreyfuss D, Ricard JD. Humidified high flow nasal oxygen during respiratory failure in the emergency department: feasibility and efficacy.Respir Care. 2012; 57 (11): 1873-8.
15. Nishimura M. High-flow nasal cannula oxygen therapy in adults. J Intensive Care. 2015; 3 (1):15.
16. Cortegiani A, Longhini F, Carlucci A, Scala R, Groff P, Bruni A, et al. High-flow nasal therapy versus noninvasive ventilation in COPD patients with mild-to-moderate hypercapnic acute respiratory failure: study protocol for a noninferiority randomized clinical trial. Trials. 2019; 20(1): 450.
17. Sun J, Li Y, Ling B, Zhu Q, Hu Y, Tan D, et al. High flow nasal cannula oxygen therapy versus non-invasive ventilation for chronic obstructive pulmonary disease with acute-moderate hypercapnic respiratory failure: an observational cohort study. Int J Chron Obstruct Pulmon Dis. 2019; 14: 1229-37.
18. Ischaki E, Pantazopoulos I, Zakynthinos S. Nasal high flow therapy: a novel treatment rather than a more expensive oxygen device Eur Respir Rev. 2017; 26(145).
19. Min Chul Kim, Yeon Joo Lee, Jong Sun Park, et al. Simultaneous reduction of flow and fraction of inspired oxygen (FiO2) versus reduction of flow first or FiO2 first in patients ready to be weaned from high-flow nasal cannula oxygen therapy: study protocol for a randomized controlled trial. 2020; 21: 81. Pending publication. 2020.
20. Bonnevie T , Elkins M , Paumier C, et al. Nasal High Flow for Stable Patients with Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-Analysis. COPD. 2019; 16(5-6): 368-77.
21. Rea H, McAuley S, Jayaram L, et al. The clinical utility of long-term humidification therapy in chronic airway disease. Respir Med. 2010; 104(4): 525-33.
22. Hasani A, Chapman TH, McCool D, et al. Domiciliary humidification improves lung mucociliary clearance in patients with bronchiectasis. Chron Respir Dis. 2008; 5(2): 816.
23. Nagata K, Kikuchi T, Horie T, et al. Domiciliary High-Flow Nasal Cannula Oxygen Therapy for Patients with Stable Hypercapnic Chronic Obstructive Pulmonary Disease. A Multicenter Randomized Crossover Trial. Ann Am Thorac Soc. 2018; 15(4): 432-9.
24. Hamada S, Tsukino M. The clinical utility of domiciliary nocturnal high-flow nasal cannula in a post-gastrectomy patient with chronic lower respiratory tract infection Pulmonology. 2018; 24(5): 312-3.
25. World Health Organization. Calcific of diseases [web]: WHO; 2018. [cited on January 30, 2020] Available at: https://www.who.int/classifications/icd/en/
26. Md Calcl. Charlson comorbidity index.2020 [cite don January 30, 2020]. Available at: https://www.mdcalc.com/charlson-comorbidity-index-cci
27. Global Initiative for Chronic Obstructive Lung Disease. Pocket Guide to COPD Diagnosis, Management and Prevention. A Guide for Health care Professional. Edition 2019.
28. Bilan N, Dastranji A, Ghalehgolab Behbahani A. Comparison of the Spo2/Fio2 Ratio and the Pao2/Fio2 Ratio in Patients With Acute Lung Injury or Acute Respiratory Distress Syndrome. J Cardiovasc Thorac Res. 2015; 7(1): 28-31.