Autor : Carnero Echegaray JoaquĂn1,2, Larocca Florencia1,4, Bellon Pablo1,3, Di Yorio Rodrigo1,6, Cancino Jorge1,5, Bosso Mauro1,3
1 Kinesiology of Respiration Service, Santa Catalina NeurorehabilitaciĂłn ClĂnica, CABA, Argentina. 2 Hospital Universitario UAI, CABA, Argentina. 3 Hospital General de Agudos Dr. Ignacio Pirovano, CABA, Argentina. 4 Hospital Naval Cirujano Mayor Pedro Mallo, CABA, Argentina. 5 Hospital Alemán, CABA, Argentina. 6 Sanatorio Colegiales, CABA, Argentina.
Correspondencia : Santa Catalina NeurorehabilitaciĂłn ClĂnica. Servicio de KinesiologĂa Respiratoria. RepĂşblica Bolivariana de Venezuela 2592 C1096 - Ciudad autĂłnoma de Buenos Aires, RepĂşblica Argentina - Tel: 54901150419343 - E-mail: jcarneroechegaray@gmail.com
Abstract
Objectives: To describe the characteristics of a cohort of decannulated patients admitted to a Neuro-rehabilitation and Critical Care Center and their condition upon discharge. The secondary objective was to analyze the existence of possible risk factors associated with referral of patients to a high complexity center.
Materials and Method: Descriptive, cross-sectional, retrospective study in the Clínica de Neurorehabilitación Santa Catalina, Autonomous City of Buenos Aires, Argentina.
Results: 87 patients were decannulated. 29 patients were admitted with IMVA and could be completely weaned. The median of TQT days was 35 days (IQR 22-68). 21% of decannulated patients were still hospitalized at the institution upon the end of the study. 53% were discharged home alive, whereas 23% had to be referred to a high complexity center. Two decannulated patients died while they were hospitalized. Some variables independently associated with referral to a high complexity center were found, the presence of a neurological history before ICU admission (OR [odds ratio] = 4.22, 95% CI [confidence interval] (1.03-10.5), p = 0.02) and ICU admission for respiratory causes (OR = 4.44, 95% CI (1.22-16.1), p = 0.02).
Conclusion: Most decannulated patients were discharged home alive. Neurological history and respiratory disease as reasons for ICU admission could be risk factors to be referred to a high complexity center.
Key words: Decannulation; Tracheostomy; Prolonged mechanical ventilation; Discharge destination.
The tracheostomy (TQT) is one of the most frequently used procedures at the Intensive Care Unit (ICU) for patients with prolonged invasive mechanical ventilatory assistance1, 2. It is performed in 34% of patients presenting invasive mechanical ventilatory assistance (IMVA) for more than 48 hours3.
Performing a TQT provides more comfort and facilitates the hygiene of the airway as well as the possibilities to move quickly to Neuro-rehabilitation and Critical Care Centers (NRCCC). The ideal time to indicate a TQT is still a matter of discussion, since there isn’t enough evidence to determine that4.
The prolonged use of the TQT involves an increased risk of developing complications, including respiratory infections, tracheal stenosis, tracheomalacia, bleeding, granuloma, etc., that could delay and even make decannulation impossible5. This increases the length of stay in the NRCCC and also the morbidity and mortality, with an even greater impact on health costs when the patient has to be referred to a high complexity center in case of complications.
Prioritizing decannulation facilitates patient discharge6. There is consensus about the importance of identifying factors that during rehabilitation may cause the referral of these patients to a high complexity center. It is very important to recognize and analyze those factors in order to improve our approach. However, the factors which could cause the referral to a high complexity center of patients who were decannulated in the NRCCC are unknown. The literature in our country only carries out a global evaluation of factors predictive of difficulty or success for decannulation6, 7.
The main objective of our study is to describe the characteristics of a cohort of decannulated patients admitted to a NRCCC and their condition upon discharge. The secondary objective was to analyze the existence of possible risk factors associated with referral of patients to a high complexity center.
Materials and Methods
We conducted a descriptive, cross-sectional, retrospective study in the Clínica de Neurorehabilitación Santa Catalina, Autonomous City of Buenos Aires, Argentina. This institution has two centers that admit tracheostomized patients with or without prolonged mechanical ventilation.
The study has been approved by the Research and Ethics Committees of the institution.
Patient Selection
The study included patients older than 18 years who after having been tracheostomized during their stay in the ICU were decannulated at the NRCCC between January 1, 2016 and December 30, 2018.
Patients referred from other weaning centers with a tracheostomy and those who were missing data and could not complete the study variables were excluded.
Procedures
We collected patients’ demographic and clinical data during their admission to our institution as part of the frequently used general database of the NRCCC. The variables of interest were then recorded in forms specifically designed for this study.
Pathological history was obtained upon admission from the discharge summary of the referral center. Also, during hospitalization one direct family member was interviewed (secondary source) in order to complete the health condition evaluation of the patient before admission to the ICU.
Upon the patient’s discharge, the variables associated with the decannulation process and with the discharge of decannulated patients were recorded in the database. With regard to the subgroup of alive patients who had to be referred to a high complexity center, we evaluated the existence of possible risk factors independently associated with their referral to an acute care center.
Patient decannulation was performed applying the protocol used in our institution.
In order to be admitted to the decannulation protocol, the patient had to meet certain requirements:
• Not having required IMVA for the last 72 hours.
• 72 hours must have passed since admission to the institution.
• Maximal expiratory pressure (PEmax) > 40 cmH2O.
• Reduced secretions.
• TQT cannula with subglottic suction port.
• Suction of the oropharyngeal secretions (OPS) of less than 10 cm3.
Our decannulation protocol started by observing tolerance to balloon deflating and cannula occlusion to evaluate the permeability of the upper airway (UA). If the patient showed stridor or absence of airflow at the UA (signs of potential obstruction), the diameter of the TQT cannula was reduced. If
signs of obstruction persisted, a fibrobronchoscopy (FBC) was performed to evaluate anatomopathological alterations of the UA.
But if the patient showed good flow through the UA, we evaluated tolerance to the phonation valve/ button. At this point, we observed the efficacy of cough, phonation and deglutition of saliva. If during the test the patient showed persistent cough or increased work of breathing (WOB), we proceeded to inflate the balloon and continue rehabilitation treatment, to be re-evaluated after 10 days.
If the patient showed good tolerance to the phonation valve/button, we conducted the Blue Dye Tests (BDT) with blue paste dye for 3 days with the patient seating, lying down and at night. If the BDT was positive, the balloon of the TQT cannula was inflated and the test was repeated after 10 days. If the BDT was negative, the patient continued having the phonation valve/button for one week.
If after one week, the patient still showed with good tolerance and his/her clinical condition was not compatible with signs of aspiration, we performed blood gas tests, FBC to evaluate anatomopathological alterations of the airway (AW) and peak cough flow (PCF). If blood gas tests and the FBC were normal, and the PCF was > 160 l/m, the patient was decannulated.
Study Variables
“Decannulated patient” was defined as the patient whose tracheostomy cannula could be successfully removed during his/her hospitalization in the NRCCC. We considered the cases as successful when there was no need to replace the tracheostomy cannula during hospitalization in our institution.
We analyzed the demographic and clinical characteristics of decannulated patients, as for example: age; gender; maximal inspiratory pressure (PImax) and PEmax; respiratory history (asthma, chronic obstructive pulmonary disease, pneumonia, AW disorders, other), neurological history (stroke, Parkinson’s disease, cranio-encephalic trauma, reversible or non-progressive neuromuscular diseases), toxic-metabolic history (diabetes, dyslipemia, alcohol abuse, illegal drug abuse, hypothyroidism, renal failure, obesity, smoking, other) and cardiovascular history (myocardial revascularization surgery, high blood pressure, myocardial infarction, other); admission to the ICU for neurological reasons (defined as every patient admitted to the ICU with peripheral or central nervous system disease, reversible or non-progressive), for respiratory reasons (COPD exacerbation, acute respiratory failure, pneumonia or AW disorders), for cardiovascular reasons (valvular disease, pump failure, heart attack, cardiac arrest, other) and infectious-metabolic reasons (ketoacidosis, sepsis); conscious awareness on admission, assessed through the coma recovery scale-revised (CRS-R) with the patient in a conscious state, in a minimally conscious state (MCS), with unresponsive wakefulness syndrome (UWS) or coma8; number of IMVA weaning days (considering weaning successful after 72 hours without requiring invasive ventilatory support); number of IMVA days; number of TQT days at the NRCCC; number of days from the last negative BDT until decannulation; number of days from decannulation until closure of tracheocutaneous stoma; and length of stay in the NRCCC.
The condition of decannulated patients upon discharge was classified as “alive” or “dead”. Patients who were discharged alive were classified according to the reason for their discharge, as “institutional discharge” (the patients go home or to a center for less complexity patients) or “referral to a high complexity center” (referral of patients to an acute care center).
Statistical Analysis
The descriptive statistical values were expressed as median and interquartile range (IQR) 0.25-0.75 or mean and standard deviation, according to the results obtained in the Lilliefors Normality Test.
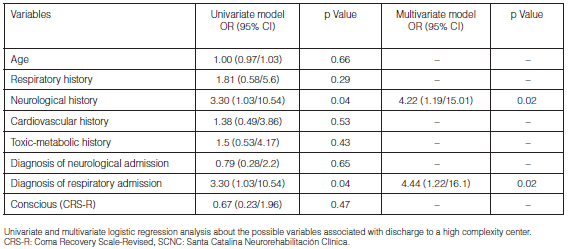
We conducted a univariate and multivariate logistic regression analysis of the group of patients referred to a high complexity center.
Results
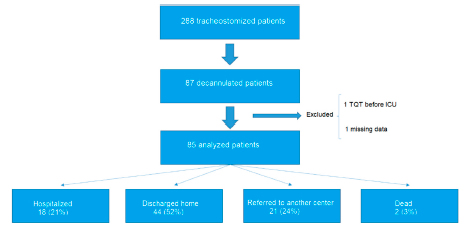
During the period under evaluation, 288 tracheostomized patients were admitted to our institution. The TQT could be removed from 87 of the 288 patients (Figure 1). Two patients were excluded from the study (one had had a previous TQT before being admitted to the ICU and the other one failed to provide some information for the statistical analysis). The clinical-demographic characteristics of decannulated patients can be observed in Table 1. 60% of them had been admitted to the ICU for central nervous system disease. 17 of them showed chronic disorder of consciousness.
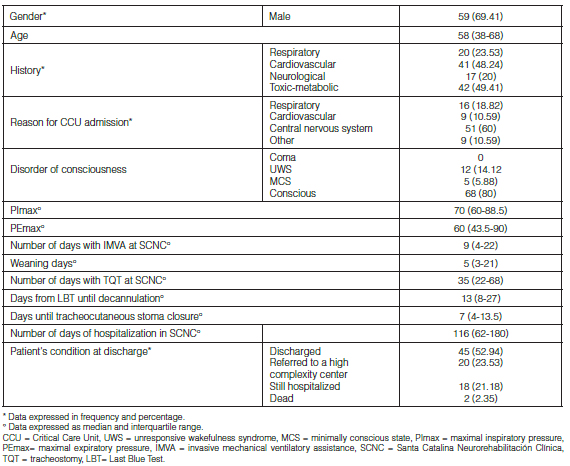
29 (34.1%) of the decannulated patients were admitted with IMVA and could be successfully weaned from it, with a median of weaning days and days with IMVA at the NRCCC of 5 (IQR = 3-21) and 9 (IQR = 4-22), respectively.
The median of TQT days was 35 days (IQR 22-68). Once the tracheostomy cannula was removed, the median time for tracheocutaneous stoma closure was 7 days (IQR 4-13.5).
21% (18) of the 85 patients who could be decannulated were still hospitalized in the institution at the end of the study. 53% (45) of the remaining patients were discharged home alive, whereas 23% (20) had to be referred to a high complexity center. Discharged patients showed a median of TQT days and hospitalization days in our institution of 35 (IQR = 22-68) and 116 (IQR = 62-180), respectively. Two decannulated patients (3%) died while they were hospitalized.
Table 2 shows the univariate and multivariate logistic regression analyses of the possible variables that could be associated with the referral to a high complexity center. Some variables independently associated with referral to a high complexity center were found, the presence of a neurological history before ICU admission (OR = 4.22, 95% CI (1.03-10.5), p = 0.02) and ICU admission for respiratory causes (OR = 4.44, 95% CI (1.22-16.1), p = 0.02).
Discussion
There is scarce literature in our country describing a population of subjects decannulated at a critical care center for chronically ill patients. The percentage of decannulation (29.5%) presented by our population of patients is very similar to the one reported in the literature, approximately within the lowest limits, from 31% to 44%1, 7, 9-11.
The median age of decannulated patients was 58 (IQR 38-68) years old, consistent with the published literature6, 7, 12.
Regarding the length of stay in the NRCCC, the median of days was relatively higher than the one reported in the literature6, 7, 13. This could be caused by socioeconomic factors that complicate patient discharge.
34.11% (29) of patients were admitted with IMVA. Their median of weaning days was 5, with 22 days of IMVA in 75% of the cases, just like the information reported by Diaz Ballve et al.6 However, the values were lower than those published by Heidler et al (regarding days of IMVA); the reason is because like in most international institutions, there is an area for the management of acute patients, thus they record the information about their whole stay12.
The median of TQT days at the institution was 35 days, around 7 to 10 more days than those reported in the literature. The reason for this may be the strict compliance with our protocol6, 7, 14, 15.
To the best of our knowledge, there aren’t any published studies that analyze the amount of days from decannulation until the closure of the stoma. This is a very important factor in our institution, being a protocol requirement for the patient’s discharge. On the other hand, the presence of a permeable tracheocutaneous stoma is a factor that facilitates infections and complicates both deglutition and phonation. According to Kubler et al, the patients showed closure of the tracheocutaneous stoma within 14 weeks after decannulation, whereas 70% of those who couldn’t do it within that period developed tracheocutaneous fistula. This agrees with the information reported by Van Heurn et al, where only two patients developed a fistula requiring surgical closure after 16 weeks. It is important to say that 75% of our sample showed closure of the tracheocutaneous stoma within two weeks (13.5 days) and no surgical procedure was required in any case, as described by various authors16,17.
The presence of a prolonged TQT may be detrimental to functional recovery and could be associated with longer hospital stay and greater use of resources16. More than 50% of decannulated patients were discharged home alive. Two patients (3%) died at the institution. These values are also consistent with the published literature, showing the importance of removing the TQT cannula in terms of mortality6, 7, 9, 13, 19.
A high percentage of decannulated patients didn’t show chronic consciousness disorder upon admission to the NRCCC, but 14.12% (12) showed UWS. This is not consistent with the work reported by several authors who in some cases don’t include that condition in their work protocols or consider it a relative contraindication12, 20-24.
More than 20% of discharged patients were referred to a high complexity center. There aren’t any published studies evaluating whether there is an associated factor that explains why those patients were referred to another center. Several authors have made a quantitative analysis of the subjects who upon discharge had to be referred to a high complexity center, went home or died, within a more general population. Del Bono et al described the discharge of a group of tracheostomized patients from an ICU, where 30% of the subjects died or had some intercurrent conditions. Unlike our study, their sample included patients who could not be decannulated. On the other hand, Scrigna et al observed that a great percentage of patients who could be decannulated were discharged home and 13% had worsening conditions or died at the institution, without evaluating possible causes associated with their intercurrent condition. Bonnici et al couldn’t calculate the percentage of patients with worsened conditions since they had a high complexity center, but were able to observe that 14.5% of patients with tracheostomy and difficult weaning died at the hospital; they didn’t evaluate the causes of possible associated complications7, 25, 26, either.
In our study we observed that the presence of a neurological history and hospitalization in the ICU for respiratory reasons were associated with a greater chance of discharging to a high complexity center. Although no evidence was found in other weaning centers, Hernández et al showed that TQT patients with neurological disease have higher mortality at the ICU. Pilcher et al observed that tracheostomized patients with neuromuscular disease were not associated with higher mortality but had low probabilities of being weaned from IMVA. Alternatively, Choate et al described that patients admitted to the ICU for respiratory causes may worsen their prognosis by increasing IMVA days. Bertrand et al concluded that admission to the ICU for respiratory reasons may worsen the patient’s prognosis and increase IMVA days9, 13, 14, 27.
Regarding study limitations, we can mention missing ICU data that could have allowed a better analysis of causes for referral to an acute care center from the NRCCC, and its retrospective nature.
Conclusion
Most decannulated patients were discharged home alive. Neurological history and respiratory disease as reasons for ICU admission could be risk factors associated with referral to a high complexity center.
Conflicts of interest: The authors declare there is no conflict of interest.
References
1. O’ Connor HH, Kirby KJ, Terrin N, et al. Decannulation Following Tracheostomy for Prolonged Mechanical Ventilation. J Intensive Care Med 2009; 24 (3): 187-94.
2. Tobin AE, Santamaria JD. An intensivist-led tracheostomy review team is associ ated with shorter decannulation time and length of stay: a prospective cohort study. Crit Care 2008; 12: R 48.
3. Dhand R. Johnson JC. Care of Chronics Tracheostomy. Respir Care. 2006; 51(9): 984-1004.
4. Añón JM. Does early versus late tracheotomy afford benefits in ventilated patients? Med Intensiva. 2015; 39(9): 573-4.
5. Epstein SK. Late complications of tracheostomy. Respir Care 2005, 50: 542-9.
6. Diaz Ballve P, Villalba D, Andreu M, et al. DecanulAR. Factores predictores de dificultad para la decanulación. Estudio de cohorte multicéntrico. Rev Am Med Resp 2017; 1: 12-24.
7. Scrigna M, Plotnikow G, Feld V, et al. Decanulación después de la estadía en UCI: Análisis de 181 pacientes traqueostomizados. Rev Am Med Resp 2013; 2: 58-63.
8. Giacino JT, Kalmar K, Whyte J. The JFK Coma Recovery Scale-Revised: Measurement, Characteristics and Diagnostic Utility. Arch Phys Med Rehabil. 2004; 85: 2020-9
9. Hernández Martínez G, Fernández R, Sánchez Casado M, et al. Tracheostomy Tube in Place at Intensive Care Unit Discharge Is Associated With Increased Ward Mortality. Resp Care. 2009; 54:1644-52.
10. Mackiewicz-Nartowicz H, Mackiewicz-Milewska M, Lach S, et al. Decannulation factors in patients after serious brain injuries. Advances in Palliative Medicine 2008; 7: 69-72.
11. Scheinhorn DJ, Stearn Hassenpflug M, Votto JJ, et al. Post- ICU mechanical ventilation at 23 long-term care hospitals: a multicenter outcomes study. Chest 2007; 131 (1): 85-93.
12. Heidler MD, Salzwedell A, Jöbges M, et al. Decannulation of tracheotomized patients after long-term mechanical ventilation – results of a prospective multicentric study in German neurological early rehabilitation hospitals, Heidler et al. BMC Anesthesiology. 2018; 18: 65.
13. Herer B. Outcomes of Tracheostomized Subjects Undergoing Prolonged Mechanical Ventilation in an Intermediate-Care Facility. Respiratory Care. 2018; 63: 282-8.
14. Choate K, Barbetti J, Currey J. Tracheostomy decannulation failure rate following critical illness: A prospective descriptive study. Australian Critical Care. 2009;22: 8-15.
15. Budweiser S, Baur T, Jorres R. Predictors of successful decannulation using a tracheostomy retainer in patients with prolonged weaning and persisting respiratory failure. Respiration 2012; 84: 469-76.
16. Kulber H, Passy V. Tracheostomy Closure and Scar Revisions. Arch Otolaryngol. 1972; 96: 22-6.
17. van Heurn E, Goei R, De Ploeg I, et al. Late Complications of Percutaneous Dilatational Tracheostomy. Chest 1996; 110: 1572-6.
18. Leung R, MacGregor L, Campbell D, et al. Decannulation and survival following tracheostomy in an intensive care unit. Ann Otol Rhinol Laryngol. 2003; 112: 853-8.
19. Ponfick M, Wiederer R, Nowak D. Outcome of Intensive Care Unit–Dependent, Tracheotomized Patients with Cerebrovascular Diseases. J Stroke and Cerebrovasc Dis. 2015; 24: 1527-31.
20. Hernández G, Ortiz R, Pedrosa A, et al. La indicación de la traqueotomía condiciona las variables predictoras del tiempo hasta la decanulación en pacientes críticos. Med Intens. 2012; 36: 531-9.
21. Garuti G, Reverberi C, Briganti A, et al. Swallowing Disorders in Tracheostomised Patients: A multidisciplinary/multiprofessional Approach in Decannulation Protocols. Multidiscip Respir Med. 2014; 9(1): 36.
22. Ceriana P, Carlucci A, Navalesi P, et al. Weaning from tracheotomy in long-term mechanically ventilated patients: feasibility of a decisional flowchart and clinical outcome. Intensive Care Med. 2003; 29: 845–8.
23. Pandian V, Miller CR, Schiavi AJ, et al. Utilization of a Standardized Tracheostomy Capping and Decannulation Protocol to Improve Patient Safety . Laryngoscope. 2014; 124: 1794–800.
24. Zanata Ide L, Santos RS, Hirata GC. Tracheal decannulation protocol in patients affected by traumatic brain injury. Int Arch Otorhinolaryngol. 2014; 18: 108–14.
25. Del Bono M, Santana McKinley JA, Sosa A, et al. Retrospective study from tracheostomies patients in the British Hospital related with the time of invasive mechanical ventilation. Fronteras de Medicina 2017; 12: 137-9.
26. Mifsud Bonnici D, Sanctuary T, Warren A, et al. Prospective observational cohort study of patients with weaning failure admitted to a specialist weaning, rehabilitation and home mechanical ventilation centre. BMJ Open 2016;6:e010025.
27. Pilcher DV, Bailey MJ, Treacher DF, et al. Outcomes, cost and long-term survival of patients referred to a regional weaning centre. Thorax 2005; 60: 187-92.