Autor : SĂvori MartĂn, Pascansky Daniel
Pulmonology and Tuberculosis Unit, Hospital Dr. J. M. Ramos MejĂa, Buenos Aires, Argentina
Correspondencia :MartĂn SĂvori, Pulmonology and Tuberculosis Unit, Hospital General de Agudos Dr. J. M. Ramos MejĂa, Urquiza 609, 1221 Buenos Aires, Argentina Correspondence: sivorimartin@yahoo.com
Abstract
There is little information about direct costs of acute asthma hospitalization in our country. This study was conducted for the purpose of determining such costs in a public hospital of the city of Buenos Aires.
Clinical records of adult patients with acute asthma admitted to the Hospital General de Agudos Dr. J. M. Ramos Mejía of the city of Buenos Aires during 2016 were reviewed. The study determined direct costs from the funder’s perspective, according to the resource allocation of the Government of the City of Buenos Aires for hospitalizations as of January 2018. The cost was informed in American dollars given the variation of the peso/dollar relationship, taking into account the exchange parity of January 2018.
25 hospital admissions of 20 patients were reviewed ; age 49 years old (median, 25-75% IQR, 36.5-62 years); 56% female; smokers (20% ex-smokers and 30% current smokers). Ten patients (50%) had had severe exacerbations the previous year. Only 10% of the patients adhered to previous preventive treatment, including the use of β2 agonists the previous month, 2.55 aerosols per patient (25-75% IQR, 2-3). The length of hospital stay was 7 days (median, 25-75% IQR, 4-10) in patient rooms and 14 days in the Intensive Care Unit. The total direct cost was 1,853 dollars per each hospitalization (median, 25-75% IQR, 1,393-2,654) in patient rooms and 6,361 dollars for the Intensive Care Unit.
This is the first study in the country to deal with the direct costs of acute asthma hospitalization in a public hospital of Buenos Aires. Taking into consideration the low adherence rate to preventive treatment, we understand that a health system based on asthma management programs reduces and saves costs that could be used in many different ways within public health.
Key words: Asthma; Asthma attack; Costs; Hospitalization.
Introduction
Asthma is the most frequent obstructive pulmonary disease; it affects from children to older adults, and is characterized by the inflammation of the respiratory airways and variable obstruction of the airflow1. Given its epidemiological behavior and associated problems, international experts yearly update the known diagnostic and therapeutic guidelines such as the Global Initiative for Asthma (GINA)1. Estimations of the number of people who suffer from asthma throughout the world vary from 235 to 300 million, and the last information indicates that its prevalence increases both in children and in adults1. If the current tendency prevails, in 2025 there will be 100 million asthmatics1. In our country, asthma prevalence in adults ages 20 to 44 in 2015 was 9.53%2, according to a phone survey carried out by the Instituto Nacional de Enfermedades Respiratorias “E. Coni” and the Argentinian Ministry of Health, using the European Communities Respiratory Health Survey. According to the international standardized ISAAC questionnaire (International Study of Asthma and Allergies in Childhood), prevalence of asthma in adolescents ages 13-14 in Argentina is 9.3%3. There are approximately 239,000 asthma-related deaths every year (0.4% of all disease-related deaths), though there is a considerable regional variation regarding mortality rates4. Mortality around the world is still unconscionably high, as well as hospitalization for asthma. Asthma affects millions of patients in Latin America, and in most patients (more than 90%) the disease is not controlled, meaning that symptoms and quality of life become worse and there are more unscheduled medical consultations at the emergency services5-7. Asthma is probably the respiratory disease that has been researched the most in economic terms, and is a critical public health problem, since deaths can be prevented with the adequate treatment (in general they are young patients), and emergency hospital admissions and consultations prove that it is not adequately managed. This lack of control of the disease and the subsequent use of healthcare resources for unscheduled consultations at home care services, emergency services, hospitalizations and use of rescue drugs increase the cost of the disease, both from the perspective of the patient and also of health system funders. In different health systems with various structures, it became necessary to conduct studies to determine the direct and indirect costs (days lost from work and school, decline in life expectancy) of the poor control of the disease. Differences among countries and health systems make it difficult to compare costs; however, there are several studies that have tried to determine such comparison. Existent pharmacoeconomic studies tend to analyze only partial aspects8. The cost of assistance and treatment in industrialized countries are estimated between 1 and 2% of the total health-related costs8. The estimated figures of annual costs (direct and indirect) are 19,300 million € in Europe and 56,000 million in USA8. Current guidelines for the management of asthma, both national and international, take into account the economic impact as an aspect to be considered when making decisions related to the approach of this disease1,9. There isn’t any information in Argentina about the direct cost of acute asthma hospitalization in any of the different health systems of our country.
The purpose of this study is to determine the direct costs of patients hospitalized for acute asthma in a public hospital in the City of Buenos Aires (CABA) in year 2016 from the funder’s perspective.
Materials and Methods
We reviewed the clinical records of patients with acute asthma who were hospitalized in all the areas of the Hospital General de Agudos Dr. J. M. Ramos Mejía of the City of Buenos Aires (CABA) from January 1, 2016 to December 31, 20161. We included adults older than 18 years and excluded the clinical records of patients whose asthma diagnosis did not justify the main need for hospitalization.
We calculated the direct costs from the funder’s perspective, taking into account the costs of drugs and the resource allocation for clinical and Intensive Care Unit (ICU) hospitalization of the Government of the City of Buenos Aires (GCBA) as of January 2018, with a peso/dollar rate of 19. Due to the variation of the peso/dollar parity in the last 18 months, in this original text we will inform results in dollars. The resource allocation of the Government of the City of Buenos Aires for Public Hospitals as of January 2018 was: 191.35 dollars (3,635 pesos) for hospitalization in patient rooms per patient per day, and 418.47 dollars (7,951 pesos) for hospitalization in emergency rooms or in the Intensive Care Unit per patient and per day10. A number and type of service was already established within each module (blood chemistry, imaging, electrocardiogram, spirometry, mechanical respiratory assistance, oxygen, disposable supplies, drugs, etc., as well as shares that depend on salaries, taxes and rates, administrative expenses, equipment depreciation, feeding and laundry costs, etc.). In cases where there was an additional diagnostic practice or consultation, or if some treatment not included in the modules was used (for example, drugs), we determined the cost from the funder’s perspective after a private consultation to drugstores and providers, and the value was then added to the hospitalization cost.
We used descriptive statistics. For quantitative variables, we used the median as central measurement and the 25%-75% interquartile range (25-75% IQR) as dispersion measurement. For qualitative variables we used percentage.
Results
During 2016 there were 27 hospitalizations of 20 patients. 25 hospitalizations were analyzed (twenty patients) for having complete clinical records.
The age was 49 years (median, 25-75% IQR, 36.5-62 years). 56% of patients were female. With regard to smoking history, 10 patients (50%) had been smokers (20% ex-smokers and 30% current smokers), with a smoking load of 24 packages per year (median, 25-75% IQR, 12-45). In terms of comorbidities, five patients had history of tuberculosis, four overweight and bronchiectases, three with addictions and other three coexistence with COPD (chronic obstructive pulmonary disease).
Regarding the history of asthma, 10 patients (50%) had had severe exacerbations the previous year, and none had been ventilated or suffered a fatal episode of asthma. Only 10% of the patients adhered to previous preventive treatment, including the use of β2 agonists the previous month, 2.55 aerosols per patient (25-75% IQR, 2-3).
The function assessed by spirometry was forced expiratory volume in the first second of predicted 30% (median, 25-75% IQR, 24-49.5). There were no deaths.
For the analysis of direct costs of 25 hospitalizations: one patient had three hospitalizations and two patients had two hospitalizations each, thus 28% of hospitalizations occurred in 15% of patients. The length of hospital stay was: 1 day in emergency rooms (median, 25-75% IQR, 1-1.25), 7 days in patient rooms (median, 25-75% IQR, 4-10) and 14 days in the Intensive Care Unit (only one patient who was ventilated).
Direct Cost Analysis
With regard to the direct cost structure, 76.4% of services, consultations and treatments had been considered within the clinical module of the GCBA. However, 55.4% of the remaining costs were related to drugs and 44.6% to diagnostic practices not included in the module (Figure 1). But, if we consider the one hospitalization in the Intensive Care Unit, 92% of the costs were included in the corresponding modules (the rest was related to drugs) (Figure 2).
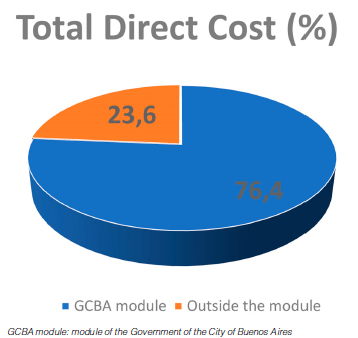
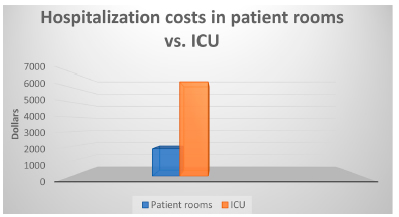
The total direct cost of each hospitalization was 1,853 dollars per patient (median, 25-75% IQR, 1,393-2,654) in the general ward. The cost for the one patient hospitalized in the Intensive Care Unit who was ventilated was 6,361 dollars (3.43 times higher than the cost of patient rooms). The annual total direct cost of hospitalization for severe asthma for all patients was 62,680 dollars.
Discussion
We have determined the direct cost of hospitalization for acute asthma in a public hospital in CABA with a methodology of primary data gathering from clinical records, which is a strength, but also supplementing this with the resource allocation modules of the GCBA. Our sample of hospitalized asthmatic patients is characterized by a slight predominance of middle-aged females with an extensive smoking history and comorbidities, previous severe exacerbations, bad adherence to treatment, little use of preventive medication and severe degree of airflow obstruction, showing inadequate control of asthma. A small number of patients justifies almost one third of hospitalizations. The direct cost for each hospitalization was 1,852 dollars per patient in the general ward and three times higher in the Intensive care Unit.
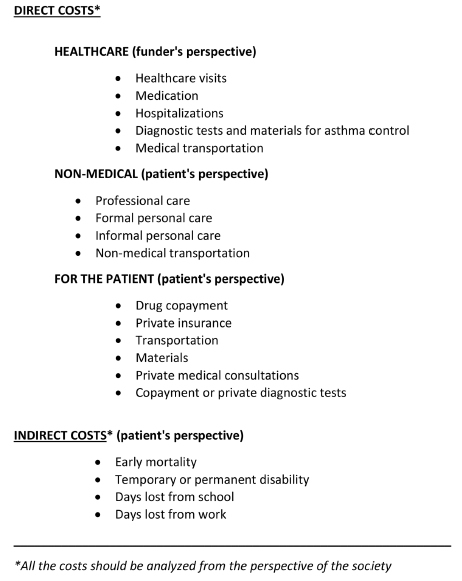
Both international guidelines and the guidelines of the Ministry of Health of our country include recommendations for the effective management of asthma, where anti-inflammatory preventive therapy with inhaled corticosteroids and beta 2 agonists with prolonged duration of action are the cornerstone1,9. However, many patients remain symptomatic and with poor asthma control. In Latin America and Argentina, two studies have shown an extremely poor control of asthma: less than 10% of patients have their asthma under control5, 6. In our study, we observed that 90% of patients didn’t adhere to treatment and that there had been a very high degree of consumption of short-acting beta 2 adrenergic bronchodilator during the previous month. It is well known that excessive consumption of salbutamol increases bronchial hyperreactivity and, consequently, the amplitude of oscillations of maximum peak expiratory flow.11-13. In our study, 50% of patients had had severe asthma attacks the previous year. The consequence is limitation to the quality of life, functional decline, increase in exacerbations and higher consumption of healthcare resources (unscheduled outpatient and emergency consultations and hospitalizations) and above all the increase in mortality14-16. All of this entails higher direct and indirect costs for the health system17-18. The Spanish Guideline on the Management of Asthma (GEMA, for its acronym in Spanish) has determined the different elements of direct and indirect costs of asthma, and the forty-seven most recommended characteristics to be used when conducting a cost study (Table 1)19.
This study meets those recommendations. We used mixed methods to determine direct costs: cost modules provided by the GCBA (top-down method) and also the review of all clinical records, including patient’s needs outside the government resource allocation modules (bottom-up method). The latter is a strength, since direct primary data have been gathered from the clinical records19. As we have already said, we conducted the cost study from the perspective of the funder (GCBA) in a public general hospital for acute illnesses, so the study conclusions could only be extrapolated to that health system. Cost comparison between countries, or direct extrapolation are not recommended, since the structure of the study varies from one country to another, with different health systems and different cost structures, but it may give us an idea of the magnitude of the problem and the qualitative strength of each variable20. We could estimate an average direct cost of USD 1,900 per year in Europe, taking into account the general cost of all the forms of severity of asthma, in comparison with USD 3,100 in the United States of North America20-24. Barnes et al reviewed 9 studies about the cost of asthma in different industrialized countries in order to find out which were the cost components associated with this disease8. They observed that indirect costs were higher than 40% of the total cost in most studies8. And in terms of direct costs, the pharmacological expenses were the highest percentage, exceeding 40%, followed by costs derived from visits to the emergency unit and hospital admissions (around 30%)8. One research about the annual cost of asthma in 462 adults with persistent asthma of 11 European countries between 1999 and 2002 showed that the mean annual cost per patient was € 1,583 and that also indirect costs predominated over direct costs on a global level25. The cost for controlled patients was only € 509; in partially controlled patients,€ 702, and in patients with uncontrolled asthma the cost was € 2,281. In controlled patients, drugs represented 87.6% of the cost, in partially controlled patients, 30.1% and in uncontrolled patients, 16.2% (in the cases of uncontrolled patients the indirect costs are higher, since days lost from work and limitations to the patient’s activities as a consequence of the disease represent 64% of the total cost)25. Around 70% of the total cost of the disease was determined by the fact that it was poorly controlled and managed. Most indirect costs and many direct costs were attributed to poor control of the disease, mainly the costs related to hospitalization and emergencies (three to four-fold increase in health costs) 25. Comorbidities, age, and severity of asthma were related to higher cost as well. The systematic review of economic studies of asthma published between 2004 and 2014 in Canada, United States and the European Union, supported similar conclusions26. England, Spain, Finland, Italy, France, and Germany have conducted the largest amount of cost studies of asthma21, 23, 27-32. For example, in 2013 an English study showed that patients with uncontrolled asthma and multiple exacerbations (almost 3% of patients) justified 7% of the total direct cost of asthma care (more than £750 million)15-18. In our study, 15% of patients justified almost one third of hospitalizations. Pavord et al showed, over 701 patients treated in the United Kingdom, that the greatest part of asthma wasn’t being controlled, and that was related to a larger proportion of unscheduled visits and emergencies (21 vs. 14%, P = 0.016), hospitalization (13 vs. 8%, P = 0.022), poorer quality of life (P < 0.001) and lower work productivity (days lost from work, 23 vs. 11%, P < 0.001) than controlled asthma27. Annual direct and indirect costs were almost double in patients with uncontrolled asthma, in comparison with controlled asthma (£6,592 vs. £3,220). The total annual cost for the society was estimated in £6,172 million (direct costs, £1,307 million and indirect costs, £4,865 million)27.
Spanish studies especially consider aspects such as the cost of maintenance treatment or hospital costs for asthma attacks29-31. In Spain, the indirect cost has been determined to almost 1,800 euros per trimester in patients with partially controlled asthma29, 30. Well-controlled asthmatics showed a mean cost per patient and per year of € 550; partially controlled asthmatics, € 746.3 and poorly-controlled € 1,451.3. Well-controlled asthma reduces health costs. The Spanish multicenter study ASMACOT analyzed global costs during 1 year in more than 600 adult patients with different degrees of severity31. If we make a comparison with previous Spanish studies, we find that annual average costs per patient are similar (€ 1,726 and € 1,964), but their structure is different: drug expenses changed from 19 to 32%, with predominance of direct costs over indirect costs (less asthma-related sick leave, less hospitalizations and fewer days lost from work) and compensating the increase caused by drugs29-31.
Finland is an exemplary country for its savings in health costs generated by the use of an effective asthma control program between 1994 and 2004. This program has included patient and health staff education, standardization of asthma management and easy access to preventive medication. For cost calculation between 1987 and 2012, it was determined that total costs were reduced 14%, average costs per patient decreased 72%, saving between 120 and 145 million euros depending on the variables, in comparison with the decade before its implementation32.
The United States of North America also have a lot of information about costs in asthma since the early 90s33. Weiss et al determined direct and indirect costs in 1990: 6,200 million dollars, with hospitalization cost being the highest (1,600 million dollars)33. 43% of the total cost derived from the use of emergencies, hospitalization and early death. Within indirect costs, the one deriving from school absence
is the most important. The total cost of asthma care in 2013 was almost 82,000 million dollars: 50,000 for direct costs, 29,000 for early deaths and 3,000 for work and school absence34.
In Latin America there aren’t many studies in this regard. Cruz et al in Brazil reported the impact of a program of severe asthma management: “The Programme for Control of Asthma and Allergic Rhinitis (ProAR)”35. A reduction of 74% was observed in hospitalizations and associated costs35. Our study is the first-in-class in Argentina. The total direct cost of hospitalization for acute asthma (median of 1,853 dollars) is similar to the European average for a 7-day stay. Just like other researches, the cost associated with hospitalization in the Intensive Care Unit was three times higher (3.43 times)24. In order to know the hospitalization costs of another obstructive chronic disease most prevalent in our country (COPD) for reference, our group also determined the direct cost of hospitalization for disease worsening (2,451 dollars) for an average stay of 14 days, also being the only information in our country about the cost of hospitalization for COPD exacerbation36.
Multiple factors have been associated with poor asthma control and a greater risk of hospitalization37, 38. Some of the most important factors are: treatment is not easily accessible, lack of adherence to treatment, errors in inhaler use and comorbidities37-39. In our study, less than one third of patients had social security and only 10% adhered to treatment. The high prevalence of errors during the administration of inhaled medication in patients with chronic obstructive diseases, such as asthma and COPD is well-known throughout the world, and is related to difficult-to-treat asthma7. Usmani et al determined that advanced age, low socioeconomic and educational level, lack of previous training in the correct inhalation therapy and the presence of comorbidities were the factors associated with errors in the administration method, thus, associated with poor asthma control and increase in the use of healthcare resources37. In terms of comorbidities, it has been determined that depression, chronic rhinitis, gastroesophageal reflux and obesity are more frequent in patients with asthma, causing a more complicated management of the disease and decrease in quality of life, thus greater use of healthcare resources39-41. It has been shown that if those conditions are treated, better control of asthma can be achieved41. In our study we observed a high rate of smoking, rhinitis, gastroesophageal reflux, obesity and addictions, all of them associated with poor asthma control39,42.
Among the limitations of this study, we may say that data collection from the clinical records was retrospective. Another limitation is the fact that extrapolation of study conclusions for other healthcare systems of our country or other regions (external validity) is not recommendable, due to the differences in cost structure mentioned before. Indirect costs (which are presumably higher than direct costs, from what has been previously reviewed) haven’t been evaluated, and costs weren’t determined from other perspectives (for example, the patient or the society). Initially, costs were determined in pesos, but due to currency volatility and the devaluation suffered by our country in recent times, we informed results in dollars (taking into account the peso-dollar parity at the beginning of the study). Finally, another limitation to this study could be the fact that the resource allocation modules used by the GCBA didn’t allow separating the internal cost structure in order to know which variables were considered and to what extent. In the study conducted in our hospital in patients with worsened COPD, more than fifteen years ago, we found that within the hospital cost structure, final medical care costs were 75% of the total cost, 57% was related to salaries (17.55% physicians, 37.41% nurses and 1.51% administrative staff) and 13% to drugs, disposable materials and medical practices (drugs: 8.8% of the total amount)36. The remaining 25% was related to the transference of costs from other services and general services, with 12.48 % of personnel expenses 36.
In conclusion, compliance with good medical practice guidelines, better education of patients, the correct use of the various preventive treatments and easy access to them (despite the increase in pharmacy expenses) have a significant positive global economic impact. If asthma is well controlled, less healthcare resources are used and indirect costs for society decrease. Our research summarizes direct costs related to hospitalization for acute asthma in a public hospital of CABA. Results should not be extrapolated to other healthcare systems or other regions of our country. Hospitalized patients have an extensive history of smoking and comorbidities, and findings of poor asthma control with previous severe exacerbations, poor adherence to treatment and underused preventive medication. A small number of
patients justifies almost one third of hospitalizations. The direct cost for each hospitalization was 1,852 dollars per patient in the general ward and more than three times higher in the Intensive care Unit. Probably, indirect costs are much higher. For that reason, programs for the systematized management of acute asthma should be arranged in order to identify poorly controlled patients and facilitate their access to preventive medication and treatment adherence, thus reducing hospitalizations that entail high costs for the healthcare system and could be avoided.
Conflicts of interest: Dr. Martin Sívori has participated in symposiums, educational videos and provided advice on asthma for Astra Zeneca. He has also participated in continuing medical education programs about asthma for Novartis.
Dr. Daniel Pascansky has participated in symposiums, educational videos, advice on asthma for Astra Zeneca, Glaxo SmithKline, Boehringer Ingelheim, Elea-Phoenix, Casasco, and also in continuing medical education programs about asthma for Novartis.
1. Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. Access on September 1, 2019 at www.ginasthma.org
2. Arias S. Primera Encuesta de Prevalencia de Asma en población de 20 a 44 años en Argentina. Ministry of Health of the Nation. 2015.
3. Forno E, Gogna M, Cepeda A, et al. Asthma in Latin America. Thorax 2015; 70: 898-905.
4. Ebmeier S, Thayabaran D, Braithwaite I, Benamara C, Weatherall M, Beasley R. Trends in international asthma mortality: analysis of data from the WHO Mortality Database from 46 countries (1993-2012). Lancet Respir Med 2017; 390: 935-45.
5. Neffen H, Moraes F, Viana K, et al. Asthma severity in four countries of Latin America. BMC Pulm Dis 2018; 19: 123.
6. Máspero J, Jardim JR, Aranda A, et al. Insights, atitudes and perceptions about asthma and its treatment : findings form a multinational survey of patients from Latin America. World Allergy Org J 2013; 6: 19.
7. Global Initiative for Asthma. GINA Difficult-to.treat& Severe Asthma in adolescent and adults patients: Diagnosis and Management. V2.0.April. Access on September 1, 2019 at www.ginasthma.org
8. Barnes PJ, Jonsson B. The costs of asthma. Eur Respir J 1996; 9: 636-42.
9. Calabrese C. Protocolo de Orientación para el diagnóstico y manejo del asma en adultos. Ministry of Health of the Nation. 2015. Access on September 1, at www.msal.gob.ar
10. Ministry of Health of the Government of the City of Buenos Aires. Personal Communication. January 2018.
11. Frey U, Brodbeck T, Majumdar A, Taylor DR, Town GI, Silverman M, Suki B. Risk of severe asthma episodes predicted from fluctuation analysis of airway function. Nature 2005; 438: 667-700.
12. Stanford RH, Shah MB, D’Souza AO, et al. Short-acting beta-agonist use and its ability to predict future asthma-related outcomes. Ann Allergy Asthma Immunol 2012; 109: 403–07.
13. Gonem S, Cumella A, Richardson M. Asthma admission rates and patterns of salbutamol and inhaled corticosteroid prescribing in England from 2013 to 2017. Thorax 2019; 74: 705-6.
14. Williams SA, Wagner S, Kannan H, Bolge SC. The association between asthma control and health care utilization, work productivity loss and health-related quality of life. J Occup Environ Med 2009; 51: 780-5.
15. Godard P, Chanez P, Siraudin L, Nicoloyannis N, Duru G. Costs of asthma is correlated with severity: a 1-yr prospective study. Eur Respir J 2002; 19: 61-7.
16. Watson L, Turk F, James P, Holgate ST. Factors associated with asthma mortality after an asthma admission: a national United Kingdom database analysis. Respir Med 2007; 101: 1659-64.
17. National Asthma Campaign. Report on the cost of asthma in Australia. 1992.
18. Thompson S. On the social cost of asthma. Eur J Resp Dis 1984; 65: 185–91.
19. Trapero Bertrán M, Oliva Moreno J. and GECA group of experts. Costo en asma GEMA. Guía Metodológica para la Estimación de Costos en Asma. LUZAN 5 SA, 2017. Pages 1-72.
20. Nunes C, Pereira AM, Morais Almeida M. Asthma costs and social impact. Asthma Research Pract 2017; 3: 1.
21. Jacob C, Bechtel B, Engel S, et al. Healthcare costs and resource utilization of asthma in Germany: a claims data analysis. Eur J Health Econ 2016; 17: 195-201
22. Lee LK, Obi E, Kavati A, Chipps B. Asthma control and disease burden in patients with asthma and allergic comorbidities. J Asthma 2018; 55: 208-19.
23. Antonicelli L, Bucca C, Neri M, et al. Asthma severity and medical resource utilisation. Eur Respir J 2004; 23: 723-9.
24. Chastek B, Korrer S, Nagar S, et al. Economic burden of illness among patients with severe asthma in a managed care setting. J Manag Care Spec Pharm 2016; 22: 848-61
25. Accordini S, Corsico AG, Braggion M, et al. The cost of persistent asthma in Europe : an international population-based study in adults . Int Arch Allergy Immunol 2013;160: 93-101.
26. Puig Junoy J, Pascual Argenté N. Costes socioeconómicos del asma en la Unión Europea, Estados Unidos y Canadá: revisión sistemática. Rev Esp Salud Pública 2017; 91: 1-15.
27. Pavord I, Mathieson N, Scowcroft A, Pedersina R, Isherwood G, Price N. The impact of poor asthma control among asthma patients treated with inhaled corticostoroids plus long-acting B2 agonists in the United Kingdom: a cross-sectional analysis. NPJ Primary Care Respir Med 2017; 27: 17.
28. Watson L, Turk F, James P, Holgate ST. Factors associated with asthma mortality after an asthma admission: a national United Kingdom database analysis. Respir Med 2007; 101: 1659-64.
29. Borderías Clau L, Zabaleta Murguiondola M, et al. Costo y manejo de una crisis asmática en el ámbito hospitalario de nuestro medio (estudio COAX en servicios hospitalarios). Arch Bronconeumol 2005; 41: 313-21.
30. Nieto A, Alvaréz-Cuesta E, Boquete M, Manzón A, de la Torre F. The cost of asthma treatment in Spain and rationalizing the expense. J Invest Allergol Clin Immunol 2001; 11: 139-48.
31. Martínez Moragón E, Serra Batlles J, De Diego A, et al. Costo económico del paciente asmático en España (Estudio AsmaCost). Arch Bronconeumol 2009; 45: 481-6.
32. Haahtela T, Herse F, Karjalainen J, et al. The Finnish experience to save asthma costs by improving care in 1987 - 2013. J Allergy Clin Immunol 2017; 139: 408-14.
33. Weiss KB, Gergen PJ, Hodgson TA. An economic evaluation of asthma in the United States. N Engl J Med 1992; 326: 862-6.
34. Nurmagambetov T, Kuwahara R, Garbe P. The Economic Burden of Asthma in the United States, 2008 – 2013. Ann Am Thorac Soc 2018; 15: 348-56.
35. Cruz AA, Souza-Machado A, Franco R, et al. The impact of a program for control of asthma in a low-income setting. World Allergy Organ J 2010; 3:1 67–74.
36. Sáenz CB, Sívori M, Blaho E, Sanfeliz NS. Experiencia en el Hospital Dr. J. M. Ramos Mejía y Revisión de la Literatura Rev Arg Med Respir 2001; 1: 45-51.
37. Usmani OS, Lavorini F, Marshal J, et al. Critical inhaler errors in asthma and COPD: a systematic review of impacto on health outcomes. Respir Res 2018; 19: 10.
38. Price D, Bosnic-Anticevich S, Briggs A, et al. The Inhaler Error Steering Committee. Inhaler competence in asthma: common errors, barriers to use and recommended solutions. Respir Med 2013; 107: 37-46.
39. Ferkh KE, Nwaru BI, Griffiths C, et al. Healthcare costs of asthma comorbidities: a systematic review protocol. BMJ Open 2017;7:e015102.
40. Wijnhoven HA, Kriegsman DM, Hesselink AE, et al. The influence of co-morbidity on health-related quality of life in asthma and COPD patients. Respir Med 2003; 97: 468-75.
41. Gershon AS, Wang C, Guan J, et al. Burden of comorbidity in individuals with asthma. Thorax 2010; 65: 612–8.
42. Bender BG. Depression symptoms and substance abuse in adolescents with asthma. Ann Allergy Asthma Immunol 2007; 99: 319-24.