Autor : JimĂ©nez Juan J.1, SĂvori MartĂn1
1Department of Pneumophtisiology, University Center of Respiratory Medicine “Dr. J. M. Ramos MejĂa”, Faculty of Medicine of the Universidad de Buenos Aires. Hospital General de Agudos “Dr. J. M. Ramos MejĂa”. Autonomous City of Buenos Aires. Argentina
Correspondencia : Juan J. Jiménez. Urquiza 609: Correo electrónico: juanjimenezalazar1984@gmail.com
Abstract
The
morbidity and mortality of chronic obstructive pulmonary disease (COPD) is
partly related to comorbidities. Many cohorts have shown that chronic
comorbidities are more frequent in patients with COPD than in those without it,
influencing the final prognosis of the patient.
Objective:
To
compare the Charlson and CO-morbidity Test (COTE) indices and their
relationship with mortality in COPD patients.
Materials
and Methods: A
prospective, observational cohort followed during ten years with one visit in
December 2016. The study included and evaluated patients with COPD (GOLD 2017
definition) who had comorbidities; we determined the Charlson and COTE indices
and established their relationship with mortality. Conventional statistics and
linear regression coefficient were used.
Results:
354
COPD patients were evaluated (age 66.5 ± 8.4, 66.7% male, 74.2% ex-smokers, 56
± 29.7 p/y). After ten years, 220 patients were alive (62%) and 134 had died
(38%). They had the following classification: GOLD 1 (10.16%), 2 (43.78%), 3
(37%), 4 (9.03%); A (9%), B (48.3%), C (0.6%) and D (41.8%); FEV1
post-bronchodilator 53.8 ± 20%. The Charlson Index was 4.1 ± 1.7 and the COTE
was 0.8 ± 0. The most frequent comorbidities were hypertension (AHT) 24.2%,
congestive heart failure (CHF) 12.4%, diabetes (DBT) 8.2%, cancer 7.3%, and
asthma-COPD overlap syndrome (ACOS) 3.6%. The diseases with the highest
mortality rate were CHF 21%, AHT 11.2%, DBT and cancer 8.2%, acute myocardial
infarction (AMI) 6%, obstructive sleep apnea-hypopnea syndrome (OSAHS) and ACOS
1.5%, and atrial fibrillation (AF) 0.75% %. The COTE index correlates poorly
with the Charlson index (r = 0.47). More than two-thirds of dead patients have
4 or more Charlson points. 85% of deceased patients have 1 point or less in the
COTE index.
Conclusion:Comorbidities
are very frequent in moderate to severe obstruction in COPD patients,
especially B and D. The most frequent are DBT and AHT. A Charlson index score
of ≥ 4 more accurately discriminates mortality compared to the COTE
index. There is a poor correlation between both indices.
Key
words: COPD;
Comorbidities; Mortality; Charlson; COTE
Introduction
Chronic
Obstructive Pulmonary Disease (COPD) is a respiratory condition characterized
by airflow limitation1, 2.
It affects more than 5% of the population and is associated with high morbidity
and mortality3, 4.
According
to the WHO (World Health Organization) estimates, 65 million people suffer from
mild to severe chronic obstructive pulmonary disease (COPD). The assessments
show that by 2030, COPD will be the world’s third leading cause of death5.
In
the 2015 review of Dal Negro et al it was observed that patients with COPD
showed cardiovascular, metabolic, digestive and osteoarticular comorbidities6.
The
GOLD guidelines (Global Initiative for Chronic Obstructive Lung Disease) of
2011, establish that comorbidities affect the “severity” and prognosis of the
disease and introduce CHAPTER 6: “AsÂsociated Comorbidities”7.
The
2013 chronic obstructive bronchopathy (COBP) cohort of Burgel et al shows the impact of coÂmorbidities on the quality of life
of COPD patients8.
COPD
has been associated with several comorbidities that significantly affect the
morbidity and mortality of these patients9.
The
most common cause of death in patients with severe or very severe COPD is
respiratory failure. But in mild-to-moderate COPD patients, mortality is
associated with cardiovascular comorbidities and lung cancer10.
The
first scientific communication regarding comorbidities of a cohort of COPD
patients was shown at the 2015 Congress of the Argentinian Association of
Respiratory Medicine (AAMR, for its acronym in Spanish) with the following
name: “COPD Comorbidities at the Central Region of the Country” and established
the mortality risk through the COTE Index11.
There
are well-known indices that evaluate the comorbidities of different chronic
diseases12-17.
The
Charlson Index, published in 1987, assesses comorbidities associated with
chronic diseases with the purpose of evaluating the risk of death in
hospitalized patients in a more objective manner12,
13.
The
COTE index is based on 10 diseases and has been developed for patients with
COPD17.
The
objective of this study is to compare the Charlston and COTE indices and relate
them to morÂtality in a cohort of COPD patients followed during ten years.
Materials and Methods
Prospective,
observational, cross-sectional cohort study, December 2016. The study included patients
with COPD (GOLD 2017 definition) classified according to their severity: GOLD 1
with post-bronÂchodilator FEV1 > 80% of the predicted value in relation to
FEV1/FVC < 0.7; GOLD 2 with FEV1 between 79-50%; GOLD 3 with FEV1 between
30-49% and GOLD 4 with FEV1 ≤ 29%; also taking into account the modified
combined assessment of COPD in ABCD groups exclusively based on symptoms and
history of exacerbations18.
Also,
functional evaluations were carried out ( spirometry
and 6-minute walk test). We calculated the BODE index (body-mass, airflow
obstruction, dyspnea, and exercise) and assessed comorbidities through the
BODE, Charlson and COTE indices, with survival follow-up from 1996 to December
201612,13,17,19. We
evaluated mortality according to the vital status from the date of diagnosis to
December 31, 2016.
The
Charlson index has 19 medical conditions classified in four groups according to
the importance assigned to each disease. In 1994, Charlson et al validated the
combined use of comorbidity and age12,13.
The
COTE index, created with 10 diseases, showed a mortality predictive value that
is independent from the BODE index; and a score of ≥ 4 increases the
predicted risk of death in every quartile of the BODE more than twice17.
Statistical analysis
Continuous
variables were expressed in mean ± standard deviation (SD, in case of Gaussian
distriÂbution) or median and interquartile range 25 and 75 (CI 25-75, in case
of non-Gaussian distribution). Categorical variables were expressed in
percentages. For the correlation test we used the Pearson’s linear test. An
alpha error of p< 0.05 was considered significant.
Results
Table
1 shows the demographic characteristics.
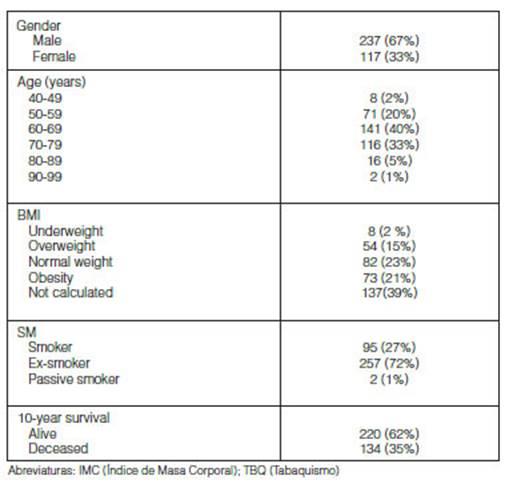
We included 354 COPD patients: age 66.5 ± 8.4, 66.7% male, 74.2% ex-smokers, (56 ± 29.7 p/y). After ten years, 220 patients were alive (62%) and 134 had died (38%), follow-up 28 (12-54.7) months (median, CI 25-75%) (Table 1).
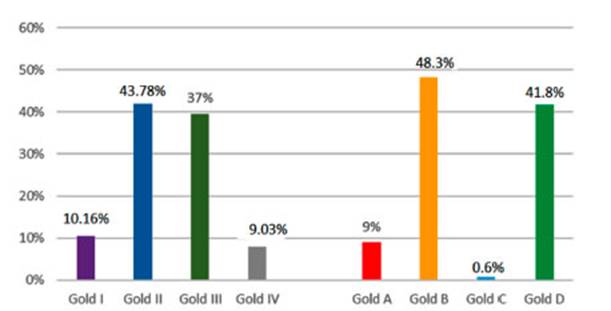
They had the following classification: GOLD 1 (10.16%), 2 (43.78%), 3 (37%), 4 (9.03%); A (9%), B (48.3%), C (0.6%) and D (41.8%) with a mean post-bronchodilator FEV1 of 53.8 ± 20% (Figure 1)
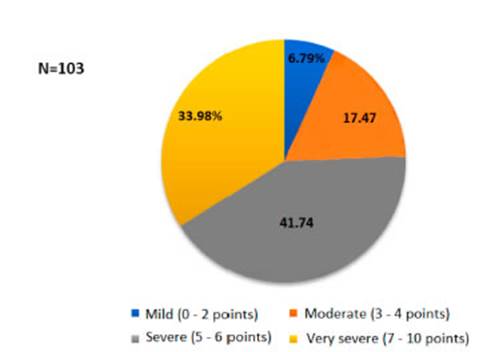
The
average distance covered in the 6-minute walk test was 294.76 ± 160.8 meters
and the BODE score was: mild (6.79%), moderate (17.47%), severe (41.74), and
very severe (33.98%) with an average of 5.5 ± 1.9 points (Figure 2).
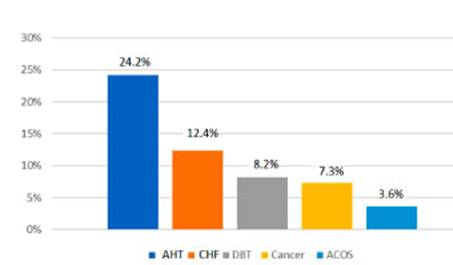
The
most common comorbidities were: arterial hypertension (AHT) 24.2%, congestive
heart failure (CHF) 12.4%, diabetes (DBT) 8.2%, cancer 7.3% and asthma-COPD
overlap syndrome (ACOS) 3.6% (Figure 3).
The
diseases with higher mortality rates were CHF 21%, AHT 11.2%, DBT and cancer
8,2%, AMI 6%, OSAHS and ACOS 1.5%, and AF 0.75%.
Also,
most comorbidities occurred in patients with Gold stages B and D and those with
mild and severe degrees of obstruction.
AHT,
CHF, AMI, and DBT were the most common comorbidities.
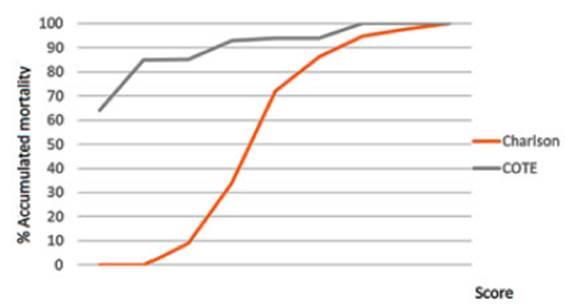
The
mean Charlson index was 4.1 ± 1.7. A cut-off point of ≥ 4 discriminates
66% of deceased patients. The mean Charlson index was 0.8 ± 0.1. 85% of
deceased patients have one point or less in the COTE index (Figure 4).
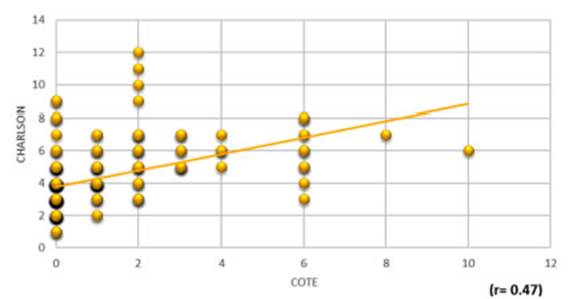
The
COTE index correlates poorly with the Charlson index (r = 0.47) (Figure 5).
In
a cohort of more than 350 patients with COPD who were followed up for twenty
years in a Department of Respiratory Medicine, most comorbidities were shown in
patients of GOLD stages B and D, with moderate and severe degrees of
obstruction; and AHT, CHF, AMI and DBT were the most common comorbidities.
There was a poor correlation between the Charlson and COTE indices. A Charlson
index score of ≥ 4 more accurately discriminated mortality compared to
the COTE index.
Cardiovascular
diseases and diabetes are the most prevalent comorbidities in patients with
COPD, and the ones mostly related to mortality.
In
the different cohorts such as ECLIPSE and PLATINO, the presence of
comorbidities in COPD is of great relevance and determines mortality in this
kind of patients20,21.
The most frequent comorbidities in the ECLIPSE study were osteoporosis, anxiety
and cardiopathies. The presence of cardiopathies and diabetes mellitus
increased the probability of death and even a C cluster was established, called
inflamÂmatory COPD with comorbidities, where it was observed that this group
showed a worse survival rate during follow-up20.
In the PLATINO study, most frequently reported diseases in the 5 cities were
arterial hypertension and cardiovascular diseases; the latter were associated
with higher rates of mortality21.
Most
of these comorbidities were found in patients with moderate and severe degree
of obstruction and groups B and D.
Ana
López et al showed in 2015, from a total of 811 evaluated patients: an
elevated prevalence of comorbidities (mean of 3.55 diseases x patient),
morbidity > 90% of the sample with > 2 comorbidities; the cardiovascular
disease was the most common comorbidity, psychiatric diseases were in third
place as regards frequency, with more anxiety than depression, a high
prevalence of comorbidities in early stages of COPD, higher percentage of
comorbidities in stages B and D, low COTE index for the general sample (2.25)
and higher risk of mortality in more symptomatic groups (B and D)12.
The
Charlson index was proposed by Mary Charlson et al in
1987 with the purpose of developing a prognostic instrument of comorbidities
that could have an impact on the short-term mortality risk of patients included
in research studies, either individually or in combination. It was initially
adapted for the evaluation of one-year survival, but finally adopted its
definite form to analyze survival after 10 years12.
In
1994, Charlson et al validated the combined use of comorbidity and age14. A score of 1 is assigned
to myocardial infarction, congestive heart failure, peripheral vascular
disease, cerebrovascular disease, dementia, COPD, connective tissue disease,
ulcerous disease, mild liver disease and diabetes. A score of 2 is assigned to
diabetes with terminally damaged organ, hemiplegia, renal disease and malignant
neoplasm, including leukemia and lymphoma. A score of 3 is assigned to moderate
or severe liver disease, whereas AIDS (acquired immunodeficiency syndrome) and
metastatic malignant tumors are assigned a score of 6. Results showed that the
relative risk of death for every decade of age was 1.42 (95% CI = 1.08- 1.88),
and for every increment in the degree of comorbidity, it was 1.46 (95% CI =
1.22-1.74). So, the estimated relative risk adjusted for every unit
(age/comorbidity) was 1.45 (95% CI = 1.25-1.68)11,
12.
The
Charlson Index, published in 1987, assesses comorbidities associated with
chronic diseases with the purpose of evaluating the risk of death in
hospitalized patients in a more objective manner, allowing us to know the
prognosis of patients with comorbidities in the geriatric population12, 13.
The
COTE index is based on 10 diseases and has been developed for patients with
COPD17. The values are
obtained by adding up the scores assigned to the patient’s diseases: if the
result is ≥ 4, it is associated with a 2 or 3-fold increase in the risk
of death17.
A
poor correlation has been shown between the two most widely used indices to
evaluate comorbiÂdities (Figure 5). The Charlson index of ≥ 4 points
more accurately discriminates mortality (66% of deceased patients), which is
not the case with the COTE index (85% of deceased patients have a 0 to 1 score)
(Figure 4). We believe this has to do with the fact that the COTE index
doesn’t adequately score the diseases that establish an important rate of
mortality in patients with COPD.
Divo
et al designed a prognostic influence study, in terms of mortality, of
comorbidities associated with COPD. A total of 79 comorbidities were reviewed
and even though AHT, dyslipidemia and obsÂtructive sleep apnea were the most
prevalent, they didn’t have a significant mortality risk. Only 12 of the
diseases that were found were independently associated with risk of death in
patients with COPD: lung cancer, anxiety in the female population, pulmonary
fibrosis, hepatic cirrhosis, atrial fibrillation, diabetic neuropathy, heart
failure and ischemic cardiopathy. The authors believe this index is easier to
calculate than the Charlson index, and better predicts the risk of mortality17.
Almagro
et al evaluated the impact on mortality after hospitalization for COPD. It was
observed that patients with 3-point Charlson index (corresponding to 2 chronic
diseases or one disease other than COPD) had twice the possibilities of dying,
as post-hospitalization predictor of mortality (P > 0.0006), regardless of
age, gender or FEV1. The most frequently associated comorbidity was chronic
heart failure, and it was the only significant comorbidity in the bivariate
analysis (p 0.001: OR 2.3; CI 1.39 to 2.83)13.
In
2010, in a new study by Almagro et al including 398 patients with COPD, the
most common coÂmorbidities were arterial hypertension (55%), arrhythmias (27%)
and diabetes mellitus (26%). 27% had heart failure, 17% coronary disease and 9%
had previous myocardial infarction with a Charlson index score of 2.72. No
relationship was found between hospital mortality and the number of
comorbidities (p = 0.8) or the Charlson index (p = 0.6)14.
The
PROFUND study from Spain reported a mean Charlson index score of 3.99, which is
clearly higher than that described by Almagro et al in
2010. Cardiovascular diseases, diabetes, dyslipidemia, renal failure and anemia
have been the most common comorbidities. It has been observed that, the higher
the number of comorbidities, measured with the Charlson index, the higher the
mortality rate15.
To
conclude, in a cohort of patients with moderate to severe COPD, with
predominance of group B and D who were followed for twenty years, the most
commonly found comorbidities were AHT, CHF, AMI and DBT. A poor correlation has
been shown between the two most widely used indices to evaluate comorbidities.
A Charlson index score of ≥ 4 points more accurately discriminates
mortality, in compaÂrison with the COTE index. It is important to identify
comorbidities in a COPD patient because they are related to a worse quality of
life, and an increase in the use of healthcare resources and mortality.
Conflict
of interests: The
authors declare that there are no conflicts of interest.
References
1.
Buist AS, McBurnie MA, Vollmer WM, et al. International variation in the
prevalence of COPD (the BOLD Study): a population-based prevalence study.
Lancet 2007; 370: 741.
2.
Gershon AS, Warner L, Cascagnette P, et al. Lifetime risk of developing chronic
obstructive pulmonary disease: a longitudinal population study. Lancet 2011;
378: 991.
3.
Centers for Disease Control and Prevention (CDC). Chronic obstructive pulmonary
disease among adults--United States, 2011. MMWR Morb Mortal Wkly Rep 2012; 61:
938.
4.
GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and
national deaths, prevalence, disability-adjusted life years, and years lived
with disability for chronic obstructive pulmonary disease and asthma, 1990-2015:
a systematic analysis for the Global Burden of Disease Study 2015. Lancet
Respir Med 2017; 5: 691.
5.
World Health Organization [consultado 23/5/2010]. Disponible en:
http://www.who.int/respiratory/copd/burden/en/index.html.
6.
Dal Negro et al. Prevalence of different comorbidities in COPD patients by
gender and GOLD stage. Multidisciplinary ReÂspiratory Medicine 2015; 10: 24.
7.
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the
diagnosis, management, and prevention of chronic obstructive pulmonary disease
(2011 Report).
8.
Pierre-Régis Burgel et al. Impact of comorbidities on COPD-specific
health-related quality of life. Respiratory Medicine 2013; 107: 233-41.
9.
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the
diagnosis, management, and prevention of chronic obstructive pulmonary disease
(2021 Report). https://goldcopd.org/ (Accessed on November 4, 2020).
10.
Soriano JB, Visick GT, Muellerova H, et al. Patterns of comorbidities in newly
diagnosed COPD and asthma in primary care. Chest. 2005; 128: 2099-107.
11.
Ana López et al. Comorbilidades de la EPOC en la Región Centro
del país. Congreso Argentino de Medicina Respiratoria. 2015.
12.
Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic
comorbidity in longitudinal studies: developÂment and validation. J Chronic Dis
1987; 40(5): 373-83.
13.
Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined
comorbidity index. J Clin Epidemiol 1994;47:1245-51.
14.
Almagro P, Calbo E, Ochoa de Echagüen A, et al. Mortality After
Hospitalization for COPD. Chest. 2002; 121(5): 1441-8.
15.
Almagro P, Salvadó M, García-Vidal C, et al. Recent improvement
in long-term survival after a COPD hospitalisation. Thorax. 2010; 65: 298-302.
16.
Díez Manglano J, Bernabeu-Wittel M, Escalera-Zalvide A, et al; en
representación de los investigadores del proyecto PROÂFUND.
Comorbilidad, discapacidad y mortalidad en pacientes pluripatológicos
con enfermedad pulmonar obstructiva crónica. Rev Clin Esp. 2011;211:504-10.
17.
Divo M, Cote C, De Torres JP et al. Comorbidities and risk of mortality in
patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med.
2012;186: 155-61.
18.
Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the
diagnosis, management, and prevention of chronic obstructive lung disease 2017
Report: GOLD Executive Summary. Am J Respir Crit Care Med 2017; 195: 557-82.
19.
Celli BR, Cote CG, Marin JM, et al. The Body-Mass Index, Airflow Obstruction,
Dyspnea, and Exercise Capacity Index in Chronic Obstructive Pulmonary Disease.
N Engl J Med. 2004; 350: 1005-12.
20.
J. Vestbo, W. Anderson, H.O. Coxson, et al. Evaluation of COPD Longitudinally
to Identify Predictive Surrogate End-points (ECLIPSE). Eur Respir J 2008; 31:
869-73.
21.
López Varela MV, Montes de Oca M, Halbert R, et al. Comorbilidades y
estado de salud en individuos con y sin EPOC en 5 ciudades de América
Latina: Estudio PLATINO. Arch Bronconeumol. 2013; 49: 468-47.