Autor Santamaria Alza Yeison, Romero MarĂn MĂ³nica P, Romero RondĂ³n Silvia K, Herrera Herrera Milena, Robayo-SĂ¡nchez Kelly Johana, Bautista-Granados Diana
Internal Medicine Service of the Hospital Universitario de Santander - Universidad Industrial de Santander
Correspondencia : Diana Patricia Bautista Granados. Correo electrĂ³nico: bautistadiana32@gmail.com. - Address: Calle 35 # 27-79 Olivara Building 1205 Bucaramanga - Santander.
Abstract
A prolonged hospital length of stay during an episode of exacerbation of chronic obstructive pulmonary disease is a condition that increases the risk of suffering associated medical complications.
Objective: The objective of this study was to determine the factors associated with a prolonged hospital length of stay in exacerbations of chronic obstructive pulmonary disease through a prediction model.
Materials and Methods: In a cross-sectional study we gathered the data of the medical records of a hospital located in the Eastern region of Colombia, between years 2012 and 2014. We carried out a descriptive, bivariate and multivariate analysis.
Results: A total of 212 patients were included in this study. 61.32% showed a prolonged hospital length of stay. We found a significant statistical association between the prolonged hospital stay and the independent variables of the bivariate analysis: dyspnea (OR [Odds Ratio]: 2.87 p = 0.04), fever (OR: 2; p = 0.02), inpatient oxygen (OR: 2.34, p = 0.003), inpatient anticholinergics (OR: 2.91, p = 0.002), inpatient antibiotic (OR: 2.25, p= 0.004), segs (OR: 1.02, p= 0.01) and lymphocytes (OR: 0.95, p = 0.003). The predictive model had a p value of 0.4950 in the analysis of goodness (Pearson Test) and a p value of 0.2689 in the goodness of fit test (Hosmer-Lemeshow Test), indicating an adequate fit. Also, the model showed an area under the curve of 0.6588.
Conclusions: Our prediction model included the following variables: age, anticholinergics and segs, for their significant association. It has an adequate fit and a good pattern of prediction.
Key words: COPD; Hospitalization/length of stay; Infection; Statistical model; Prevention.
Introduction
Chronic obstructive pulmonary disease is defined as a common disease that can be prevented and treated, characterized by the persistence of respiratory symptoms and the limitation of the airway, due to alveolar or airway abnormalities usually caused by significant exposure to gases and harmful particles1. Its prevalence in the city of Bucaramanga, Santander, diagnosed by spirometry, is of 7.9% according to data obtained from the PREPOCOL study2. Nearly 80% of the patients show periodic exacerbations of their respiratory symptoms at some point during the course of the disease. These exacerbations tend to increase progressively in frequency and intensity, determining a poor quality of life3, 4. These are episodes that worsen the respiratory symptoms and require a change in the management of the disease, and may be classified as mild, moderate and severe. Severe exacerbations are associated with hospitalization or consultation at the emergency department1.
Hospital length of stay in the case of a chronic obstructive pulmonary disease (COPD) exacerbation episode is conditioned not only by its characteristics but also by other factors such as: the comorbidities and individual, sociodemographic and clinical factors of each patient. In the literature there are studies about the association of these factors5-9, but few studies have analyzed factors associated with prolonged hospitalizations10, 11.
Hospitalization in COPD patients increases the risk of suffering associated complications such as deep vein thrombosis, hydroelectrolytic alterations and infections caused by nosocomial germs12-16. Also, the cost of the disease increases significantly in relation to the number of exacerbations and the number of hospitalization days17. For that reason, the objective of this study was to determine the risk factors associated with a prolonged length of stay, in order to be able to identify at an early stage which are the patients that could require a longer hospitalization stay, so that in the future COPD patients can be treated in a timely manner.
Materials and Methods
Study Design
Cross-sectional study carried out at the Hospital Universitario de Santander, between years 2012 and 2014, including patients with established diagnosis of COPD (spirometric criterion + clinical criterion and use of inhalation therapy). Data were obtained from medical records, respecting the patients’ privacy by assigning codes to them. The study has been approved by the Ethics Committee of the Hospital Universitario de Santander and the Universidad Industrial de Santander, in accordance with current regulations.
Patients
We included patients with an established diagnosis of COPD, older than 18 years old, who had consulted the emergency department with COPD exacerbation diagnosis defined as the increase in one of the following symptoms: dyspnea, sputum volume or change in sputum characteristics (purulent). Patients with any other chronic respiratory disease (asthma, tuberculosis sequelae, respiratory neoplasia) were excluded from the study.
Independent Variables
For the evaluation of patients with COPD exacerbation we took into account variables of general characterization (age, sex), associated comorbidities (heart failure, diabetes mellitus type 2, stroke, arterial hypertension and history of exacerbations), respiratory exposure (smoking and exposure to wood smoke), use of outpatient inhalation drugs (inhaled anticholinergics, inhaled beta 2-agonists, inhaled corticosteroids, home oxygen), symptoms upon admission (dyspnea, cough, increase in sputum, fever, thoracic pain, cyanosis), signs upon admission (alterations in respiratory auscultation, vital signs upon admission), inpatient drugs (oxygen, systemic corticosteroids, inhaled corticosteroids, inhaled anticholinergics, inhaled beta 2-agonists or antibiotics) and laboratory tests upon admission (hemogram, reactive-C protein).
Result
The primary result to be evaluated was the presence of a prolonged length of stay, defined as the number of days from hospital admission to discharge (> 5 days).
Statistical Analysis
The analysis of the gathered data was carried out using Stata 12.0 software. Quantitative variables were processed, and mean and median values of central tendency and dispersion were determined (mean
and median; standard deviation and interquartile range). Qualitative variables were analyzed with absolute frequencies and percentages. Subsequently, the association between each one of the independent variables and the result was evaluated using Chi2 or Fisher Tests for qualitative variables and Student T or Wilcoxon tests for quantitative variables. We selected variables with the greatest association, defined by a p < 0.20. We carried out a Spearman correlation analysis to determine the final variables to be included in the logistic regression analysis to predict the presence of prolonged hospitalization. The Backward methodology was used, until a statistically significant model was obtained (p<0.05). Then, we conducted a goodness of fit test, discrimination ability, sensitivity, specificity and area under the ROC curve of the model.
Results
Characteristics of Patients
258 patients were included in this study, taken from the medical records of 2012-2014. 46 patients did not comply with inclusion criteria, so, the final number of subjects included in the study was 212.
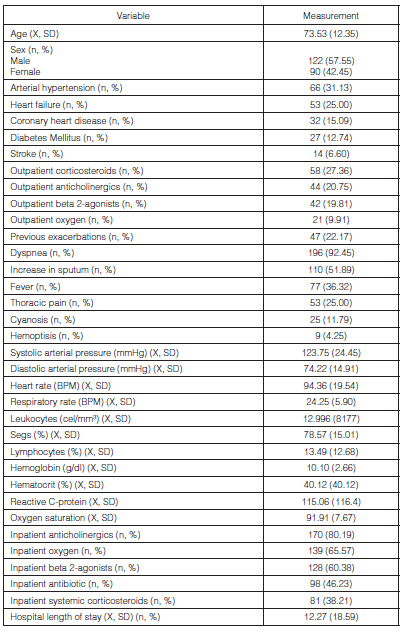
The mean age of the subjects under evaluation was 73.52 ± 12.35 years; the mean hospital stay was 12.27 ± 18.59 days with a minimum value of 1 day and a maximum value of 86 days. 57.55% of patients were male; 61.32% had a prolonged hospitalization (of more than 5 days). The most common comorbidities were: arterial hypertension (31.13%), heart failure (25%), coronary heart disease (15.09%) and diabetes mellitus (12.74%).
Subjects under evaluation show history of smoking and exposure to wood smoke in 51.42% and 37.74%, respectively, whereas 22.17% of the individuals reported previous exacerbations.
At hospital admission, the most common symptoms were: dyspnea (92.45%), cough (69.81%), increase in sputum volume (51.89%) and fever (36.32%). Regarding the respiratory test, decrease in respiratory sounds (58.49%) and presence of rales (44.34%) were most frequently found. As for the percentage of segs, we found an average of 78.57% ± 15.01.
The drugs that were indicated upon hospital admission were inhaled anticholinergics (80.19%), oxygen (65.57%), inhaled beta 2-agonists (60.38%), antibiotics (46.23%), systemic corticosteroids (38.21%) and inhaled corticosteroids (35.38%). Table 1 summarizes other patient-characterization variables.
Bivariate Analysis
As a result of the bivariate analysis, we found a significant statistical association between the prolonged hospital stay and the independent variables: dyspnea (OR: 2.87 p = 0.04), fever (OR: 2; p = 0.02), heart rate (OR: 1.01; p = 0.03), respiratory rate (OR: 1.05; p = 0.02), inpatient oxygen (OR: 2.34, p = 0.003), inpatient anticholinergics (OR: 2.91, p = 0.002), inpatient antibiotic (OR: 2.25, p = 0.004), segs (OR: 1.02, p = 0.01) and lymphocytes (OR: 0.95, p = 0.003). Table 2 shows the results of the bivariate analysis.
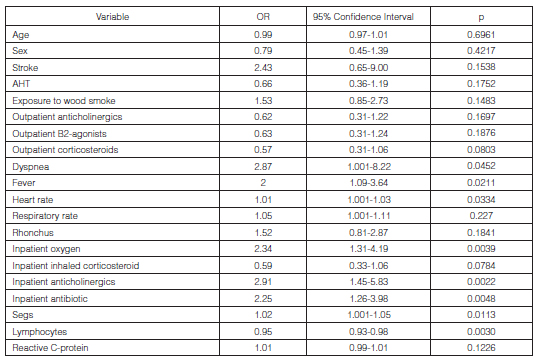
Using the Backward methodology, modeling was carried out in order to find a prediction model. With the prediction model, the following variables were obtained: age, need for inpatient anticholinergics and percentage of segs in the admission hemogram:
Prolonged hospitalization = 0.6 - (Age)*0.03 + (Inpatient anticholinergics) *0.91 + (segs)* 0.02
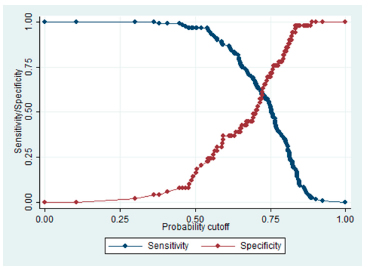
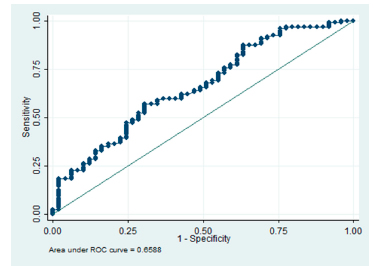
Then, the goodness of fit analysis was made, by means of the Pearson test, showing a p value of 0.4950; thus, the already mentioned values are not statistically different. Also the Hosmer- Lemeshow test was carried out, calculating a p value of 0.2689, concluding that the model fits adequately.
The calculated classification statistics were: sensitivity, 96.64%; specificity, 16.33%; positive predictive value, 73.72%; negative predictive value, 66.67% and correct classification, 73.21%. (Figure 1). We found an area under the curve of 0. 6588, which was the product of the construction of a ROC curve. (Figure 2).
Discussion
According to the relevant findings of our study, the mean age of the subjects under evaluation was 73 years. This information is similar to that found in other studies9, 18. 19. We find a positive association between age and length of hospital stay, which in previous studies have also been related7, 9. Most of the individuals under study are male (57.55%), like other studies evaluating risk factors associated with hospitalization for COPD18, 19.
It is important to underline the fact that hospital length of stay in this study was 12.27 ± 18.59 days. This finding is similar to the findings of C, Terzano, who found a mean hospitalization stay of 12.25 days7 during follow-up of a retrospective cohort in his study.
In our study, the most common associated comorbidities found in evaluated patients were arterial hypertension, heart failure, coronary heart disease and diabetes mellitus. In the study conducted by Manino, a stronger relationship was found between prolonged hospitalization stay and arterial hypertension20. Likewise, another study carried out by C, Terzano found that patients with COPD exacerbations show at least one comorbidity during hospitalization7. Comorbidities such as cardiovascular disease and diabetes mellitus type 2 are mostly associated in patients hospitalized for COPD20, and it is the increase in glucose level concentration that prolongs the length of hospital stay in acute COPD exacerbations21. However, in our study we weren’t able to determine such association, possibly due to the sample size used.
Among the most prevalent symptoms of patients with COPD exacerbations in our study we find dyspnea in 92.45% of the subjects, as well as an increase in the risk of having prolonged hospital stay. In the literature there are previous studies where dyspnea measured by the mMRC scale (modified Medical Research Council scale) was associated with a prolonged hospital length of stay, as was described by Angeliki M. Tsimogianni22. Other studies, such as the one conducted by Quintana et al have worse scores regarding the degree of dyspnea during an exacerbation measured in this case by the mMRC scale. These are a predictive factor of a prolonged hospitalization23.
Other symptoms frequently found in our study were cough and increase in the sputum volume, with a frequency of 69.81% and 51.89%, respectively. In the literature there are previous studies that showed the positive relationship between productive cough and a high risk of exacerbations24. The same happens with the increase in the sputum volume: this symptom is related to the increase in moderate and severe exacerbations, as well as in the amount of exacerbations25. It is relevant to mention that in our study, the presence of fever at hospital admission was related to a hospital stay of more than 5 days. This information hadn’t been previously reported in the literature.
22.17% of the individuals reported upon admission that they had suffered previous exacerbations. This condition is associated with a higher risk of future hospitalizations5, 26, 28. In our study we didn’t determine an association with this variable; future studies will be required with larger sample sizes in order to define if patients with recurrent exacerbations in the Colombian population could have prolonged hospitalizations.
Inhaled anticholinergics were the most frequently indicated drugs upon admission (80.19%). The literature states that the administration of this drug may reduce severe exacerbations and mortality29. In our study, the use of outpatient inhalation therapy tended to show a decrease in the risk of having prolonged hospitalizations; nevertheless, statistical significance was not achieved. On the other hand, the use of inpatient anticholinergics was associated with a higher probability of having a prolonged hospitalization; however, we believe it is not an effect of the drug but the fact that patients requiring anticholinergics possibly have a worse clinical status or require longer time for an adequate stabilization of the disease and so need prolonged hospitalizations.
In the bivariate analysis we find a positive association between the value of the segs and the prolonged hospital stay. This finding was similar to other studies that also found an association between elevated levels of segs as a risk factor for respiratory hospitalizations in patients diagnosed with COPD4.
In the literature there are studies that have previously tried to make statistical models predictive of prolonged hospitalizations after an acute exacerbation, as for example the model made by Ying Wang and Knut Stavem; however, in that study the statistical model wasn’t statistical, so it wasn’t possible to establish a prediction model10.
Other authors have created punctuation scales that try to predict prolonged hospitalizations during a current hospitalization, as for example the case of Filia Diamantea MD and associates, who designed a punctuation scale based on 7 parameters (AECOPD, Acute Exacerbations of COPD):
Anthonisen exacerbation type, number of exacerbations of the previous year, Charlson Comorbidity Index, oxygenation, partial pressure of the PaCO2 in arterial gasometry, dyspnea according to the Borg Scale and history of chronic respiratory failure, score with positive results, taking into account that the score may be useful for clinical practice30 and the duration of hospital stay is directly related to this cost. The aim of this study was to investigate possible associations of demographic, clinical, laboratory, and functional parameters with stay of subjects admitted for COPD exacerbations and to provide a score for the prediction of the need for prolonged hospitalization. METHODS: We included 164 consecutive subjects admitted to 2 respiratory medicine departments of 2 tertiary hospitals for a COPD exacerbation, and we evaluated laboratory, clinical, and functional parameters possibly related to the duration of hospital stay. RESULTS: Seven parameters evaluated on subject admission (Antonisen type of exacerbation, number of Exacerbations in the previous year, Charlson index of comorbidities, Oxygenation, Partial pressure of P(aCO2.
On the other hand, in our prediction model we determined an association with age, use of inpatient anticholinergics and the number of segs in the admission hemogram. With our model we have a more simple and quick way of determining which are the patients who will be having hospitalizations of more than 5 days. The model has an adequate fit and a good pattern of prediction.
Among the strengths of the study, there is the fact of being the first one in the region to evaluate prolonged hospitalizations, which has an important impact on the health system. When determining a prediction model for a prolonged hospital stay, it is possible to previously identify the patients who are more likely to undergo that condition. Important and relevant personal data from Colombian patients are provided for a more suitable use.
As regards the disadvantages of this work, we could mention the fact that it is retrospective, so there is an inherent bias that we tried to mitigate with the most precise measurement possible of the variables. Also, data interpretation must be cautious, since the study has been conducted in a third-level institution where patients have a higher degree of complexity.
Funding: No funding was received for conducting this study.
1. Global initiative for chronic obstructive lung disease. 2018.
2. Caballero A, Torres-Duque CA, Jaramillo C, et al. Prevalence of COPD in five Colombian cities situated at low, medium, and high altitude (PREPOCOL study). Chest. 2008; 133(2): 343-9.
3. Calle M, Morales B, Rodríguez J. Exacerbación Aguda de la EPOC. Arch Bronconeumol. 2010; 46(7): 21-5.
4. Veljanovski J, Ouellette DR. Risk factors for respiratory hospitalizations in a population of patients with a clinical diagnosis of COPD. Int J Chron Obstruct Pulmon Dis. 2018; 13: 1061-9.
5. Müllerova H, Maselli DJ, Locantore N, et al. Hospitalized exacerbations of COPD: Risk factors and outcomes in the ECLIPSE cohort. Chest. 2015; 147(4): 999-1007.
6. Rubinsztajn R, Chazan R. An analysis of the causes of mortality and co-morbidities in hospitalised patients with chronic obstructive pulmonary disease Analiza przyczyn zgonów i chorób współistniejących u hospitalizowanych chorych na przewlekłą obturacyjną chorobępłuc. Pneumonol Alergol Pol. 2011; 79(5): 343-6.
7. Terzano C, Colamesta V, Unim B, et al. Chronic obstructive pulmonary disease (COPD) exacerbation: impact of comorbidities on length and costs during hospitalization. Eur Rev Med Pharmacol Sci. 2017; 21: 3680-9.
8. De la Iglesia F, Valino P, Pita S, et al. Factors predicting a hospital stay of over 3 days in patients with acute exacerbation of chronic obstructive pulmonary disease. J Intern Med. 2002; 251(6): 500-7.
9. Agboado G, Peters J, Donkin L. Factors influencing the length of hospital stay among patients resident in Blackpool admitted with COPD: A cross-sectional study. BMJ Open. 2012; 2(5): 1-10.
10. Wang Y, Stavem K, Dahl F, Humerfelt S, Haugen T. Factors associated with a prolonged length of stay after acute exacerbation of chronic obstructive pulmonary disease (AECOPD). Int J Chron Obstruct Pulmon Dis. 2014; 9: 99-105.
11. De Miguel-Díez J, Jiménez-García R, Hernández-Barrera V, et al. Readmissions following an initial hospitalization by COPD exacerbation in Spain from 2006 to 2012. Respirology. 2016; 21(3): 489-96.
12. Chen C, Liao K. The Incidence of Deep Vein Thrombosis in Asian Patients with Chronic Obstructive Pulmonary Disease. Medicine (Baltimore). 2015; 94(44): 1-6.
13. Köhler D, Schönhofer B. Prevalence of Deep-Vein Thrombosis of the Leg in Patients with Acute Exacerbation of Chronic. Respiration. 1998; 65: 173-7.
14. Terzano C, Stefano F Di, Conti V, et al. Mixed Acid-Base Disorders , Hydroelectrolyte Imbalance and Lactate Production in Hypercapnic Respiratory Failure : The Role of Noninvasive Ventilation. PLoS One. 2012; 7(4): 1-9.
15. Rouzéa A, Cottereaua A, Nseir S. Chronic obstructive pulmonary disease and the risk for ventilator-associated pneumonia. Curr Opin Crit Care. 2014; 20(5): 525-31.
16. Nseir S, Pompeo C Di, Soubrier S, et al. Impact of Ventilator-Associated Pneumonia on Outcome in Patients With COPD *. Chest. 2005; 128: 1650-6.
17. Li F, Sun Z, Li H, Yang T, Shi Z. Factors associated with hospitalisation costs in patients with chronic obstructive pulmonary disease. Int J Tuberc Lung Dis. 2018; 22(4): 458-63.
18. Chan FW, Wong FY, Yam CH, et al. Risk factors of hospitalization and readmission of patients with COPD in Hong Kong population: Analysis of hospital admission records. BMC Health Serv Res. 2011; 11: 186.
19. Alcázar B, García-Polo C, Herrejón A, et al. Factores asociados a la hospitalización por exacerbación de la enfermedad pulmonar obstructiva crónica. Arch Bronconeumol. 2012; 48(3): 70-6.
20. Mannino DM, Thorn D, Swensen A, Holguin F. Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur Respir J. 2008; 32(4): 962-9.
21. Burt MG, Roberts GW, Aguilar-Loza NR, Quinn SJ, Frith PA, Stranks SN. Relationship between glycaemia and length of hospital stay during an acute exacerbation of chronic obstructive pulmonary disease. Intern Med J. 2013; 43(6): 721-4.
22. Tsimogianni AM, Papiris SA, Stathopoulos GT, Manali ED, Roussos C, Kotanidou A. Predictors of outcome after exacerbation of chronic obstructive pulmonary disease. J Gen Intern Med. 2009; 24(9): 1043-8.
23. Quintana JM, Unzurrunzaga A, Garcia-Gutierrez S, et al. Predictors of Hospital Length of Stay in Patients with Exacerbations of COPD: A Cohort Study. J Gen Intern Med. 2015; 30(6): 824-31.
24. Lindberg A, Sawalha S, Hedman L, Larsson LG, Lundbäck B, Rönmark E. Subjects with COPD and productive cough have an increased risk for exacerbations and death. Respir Med. 2015; 109(1): 88-95.
25. Burgel PR, Nesme-Meyer P, Chanez P, et al. Cough and sputum production are associated with frequent exacerbations and hospitalizations in COPD subjects. Chest. 2009; 135: 975-82.
26. Sadatsafavi M, Xie H, Etminan M, Johnson K, FitzGerald JM. The association between previous and future severe exacerbations of chronic obstructive pulmonary disease: Updating the literature using robust statistical methodology. PLoS One. 2018; 13(1): 1-11.
27. Wei X, Ma Z, Yu N, et al. Risk factors predict frequent hospitalization in patients with acute exacerbation of COPD. Int J Chron Obstruct Pulmon Dis. 2017; 13: 121-9.
28. Molinari N, Briand C, Vachier I, et al. Hospitalizations for COPD exacerbations: Trends and determinants of death. COPD J Chronic Obstr Pulm Dis. 2015; 12(6): 621-7.
29. Salpeter S, Buckley N, Salpeter E. Meta-analysis: Anticholinergics, but not b-agonists, Reduce Severe Exacerbations and Respiratory Mortality in COPD. J Gen Intern Med. 2006; 21: 1011-9.
30. Diamantea F, Kostikas, K, Bartziokas K, et al. Prediction of Hospitalization Stay in COPD Exacerbations: The AECOPD-F Score. Respir Care. 2014; 59(11): 1679-86.